24 Jan 2024
Coronary physiology guidance vs conventional angiography for optimization of percutaneous coronary intervention: the AQVA-II Trial
Selected in JACC: Cardiovascular Interventions by S. Brugaletta
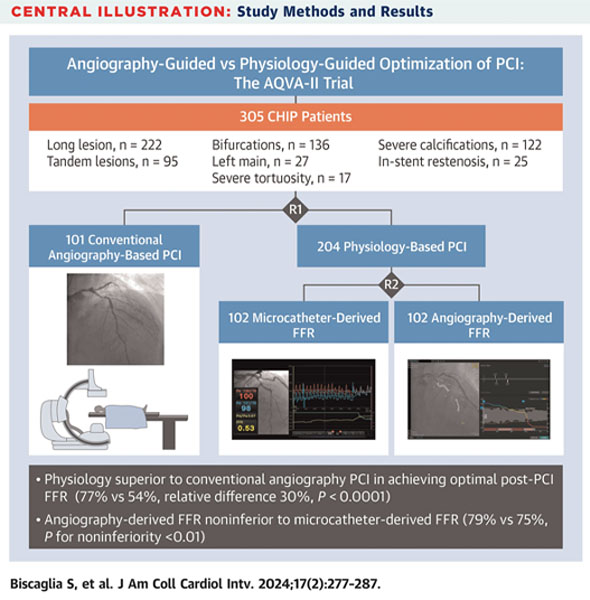
The primary aim of this study was to demonstrate the superiority of physiology-guided PCI, using either angiography or microcatheter-derived FFR, over conventional angiography-based PCI in complex high-risk indicated procedures (CHIPs) in obtaining a higher FFR post-PCI.
References
Authors
Simone Biscaglia, Filippo Maria Verardi, Andrea Erriquez, Iginio Colaiori, Marta Cocco, Anna Cantone, Graziella Pompei, Andrea Marrone, Serena Caglioni, Carlo Tumscitz, Carlo Penzo, Marco Manfrini, Antonio Maria Leone, Francesco Versaci, and Gianluca Campo
Reference
J Am Coll Cardiol Intv. 2024 Jan, 17 (2) 277–287
Published
January 2024
Link
Read the abstractReviewer
My Comment
Why this study – the rationale/objective?
There is still a debate about the efficacy of coronary physiological guidance compared with conventional angiography in achieving optimal post–percutaneous coronary intervention (PCI) fractional flow reserve (FFR) values.
The primary aim of this study was to demonstrate the superiority of physiology-guided PCI, using either angiography or microcatheter-derived FFR, over conventional angiography-based PCI in complex high-risk indicated procedures (CHIPs) in obtaining a higher FFR post-PCI.
How was it executed – the methodology?
Patients with obstructive coronary lesions and meeting CHIP criteria were randomized 2:1 to receive physiology- or angiography-based PCI. Those assigned to the former were randomly allocated to angiography- or microcatheter-derived FFR guidance.
CHIP criteria were long lesion (> 28 mm), tandem lesions, severe calcifications, severe tortuosity, true bifurcation, in-stent restenosis, and left main stem disease.
The optimal post-PCI FFR value was defined as > 0.86.
What is the main result?
A total of 305 patients (331 study vessels) were enrolled in the study (101 undergoing conventional angiography-based PCI and 204 physiology-based PCI). Optimal post-PCI FFR values were more frequently obtained in the physiology-based PCI group compared with the conventional angiography-based PCI group (77 % vs 54 %; absolute difference 23 %, relative difference 30 %; P < 0.0001). The occurrence of the primary outcome did not differ between the 2 physiology-based PCI subgroups, demonstrating the noninferiority of angiography- vs microcatheter-derived FFR (P < 0.01).
JACC : Cardiovascular Interventions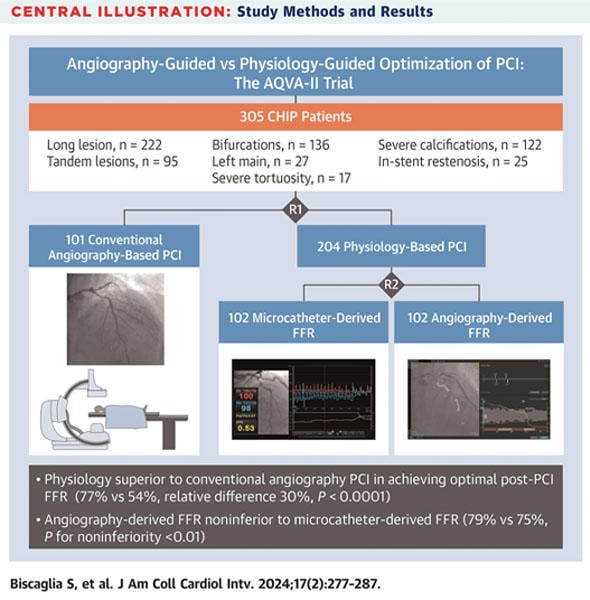
Critical reading and the relevance for clinical practice
In our daily practice, we face every day more and more complex patients than years ago. For this reason, it is important to offer to these patients the best-in-class PCI, by revising our concept of how a PCI should be performed.
This study shows that physiology-based PCI is superior to angiography-based PCI in obtaining a higher FFR post-PCI, which has been previously linked to clinical outcomes. The concept of physiology-based PCI goes beyond a single point FFR whether to decide to implant a stent, but it includes the concept of FFR pullback to understand if we are treating a focal or diffuse disease and to choose our procedural planning.
Physiology-based PCI together with imaging-based PCI should be well known by the interventional cardiology community when performing a complex PCI, as their use translates to obtaining a better outcome for our patients. For this reason, we may talk about an update of our concept of PCI to a 2.0 level beyond a simple coronary angiography.
How many of you use FFR or intracoronary imaging in treating CHIP patients?




3 comments
For complex lesions/CHIP procedures, intracoronary imaging is the preferred option (also because it provides PCI guidance)
According to the existing evidence. It is important to convince the interventional cardiologist to adopt, in a generalized way, a new way of working, which involves angiography, physiology and intracoronary imaging, basing decisions on the last two. I think it is a problem of training in these techniques and of some pride on our part. The clinical cardiologist should demand this paradigm shift.
thanks Michail. I tend to agree with you, although I am surprised to see some data about physiology and according to increasing clinical experience with physiology and with stent optimization based on physiology, the best would be to have both, maybe in the same catheter.