Rethinking false positive exercise electrocardiographic stress tests by assessing coronary microvascular function
Selected in JACC by A. N. Calik , A. Kerem Yılmaz
This study aims to compare the results of EST in patients reporting angina with those having non-obstructive coronary artery disease (ANOCA), against the reference standard of microvascular function.
References
Authors
Aish Sinha, Utkarsh Dutta, Ozan M. Demir, Kalpa De Silva, Howard Ellis, Samuel Belford, Mark Ogden, Matthew Li Kam Wa, Holly P. Morgan, Ajay M. Shah, Amedeo Chiribiri, Andrew J. Webb, Michael Marber, Haseeb Rahman, and Divaka Perera
Reference
J Am Coll Cardiol. 2024 Jan, 83 (2) 291–299
Published
January 2024
Link
Read the abstractReviewers
Our Comment

Figure 1: Exercise electrocardiographic stress testing in the contemporary era
Source: Journal of the American College of Cardiology
Why this study – the rationale/objective?
The exercise electrocardiography stress test (EST) is a non-invasive diagnostic tool used to assess angina pectoris. It offers advantages over other non-invasive imaging methods, such as no radiation exposure and lower cost. However, its usage has declined in recent years due to high false positive rates and the growing use of alternative methods. The high false positive rates are believed to be linked to the assessment based on obstruction.
This study aims to compare the results of EST in patients reporting angina with those having non-obstructive coronary artery disease (ANOCA), against the reference standard of microvascular function.
How was it executed – the methodology?
The study included patients who presented with angina complaints and had a fractional reserve of 0.80 or above, as well as a preserved left ventricular ejection fraction (> 5 0%).
Patients with chronic kidney disease (estimated glomerular filtration rate < 30 mL/minute/m2), those unable to undergo assessment with adenosine or acetylcholine, severe valvular pathology, bundle branch block on EKG, active paced rhythm, history of acute coronary syndrome, or history of revascularization, were excluded from the study.
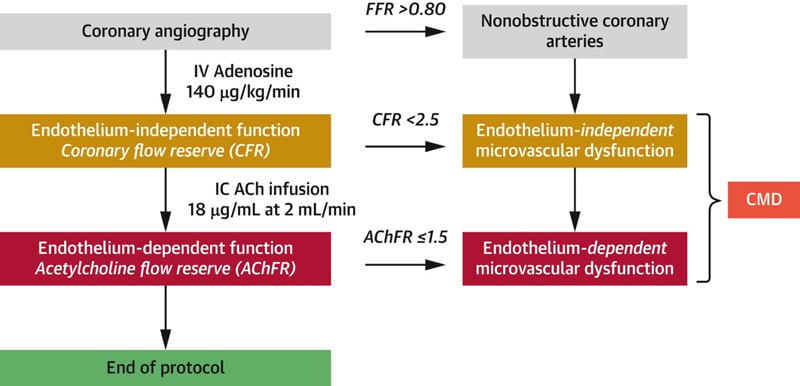
All physiological measurements were conducted in the left anterior descending coronary artery. Endothelium-independent microvascular function was assessed with intravenous adenosine, while endothelium-dependent microvascular function was evaluated with intracoronary acetylcholine infusions.
EST was performed in accordance with the guidelines of the American College of Cardiology and the American Heart Association, following invasive assessment. Patients who developed ischemic ECG changes were categorized into the "ischemic" group, while those who did not develop changes were placed in the "non-ischemic" group.
The specificity of EST results was assessed against different reference standards for ANOCA:
- Endothelium-independent microvascular function (CFR < 2.5)
- Endothelium-dependent microvascular function (AChFR ≤ 1.5)
- Endothelium-independent and/or endothelium-dependent microvascular dysfunction [i.e., coronary microvascular dysfunction (CMD); coronary flow reserve (CFR) < 2.5 and/or AChFR ≤ 1.5]. (Figure 2)
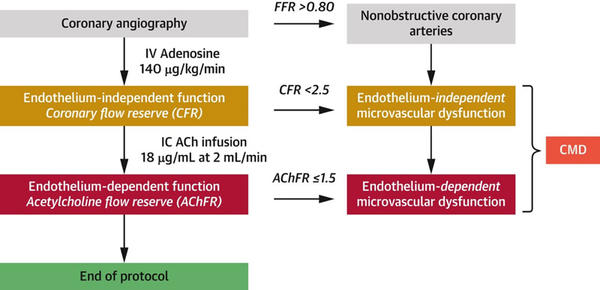
Figure 2: Coronary physiological assessment protocol
Source: Journal of the American College of Cardiology
What is the main result?
Between March 2021 and July 2023, 262 patients with stable angina were screened for eligibility. Among these, 122 diagnosed with ANOCA underwent evaluation with adenosine and acetylcholine and were considered suitable for inclusion in the study. The final analysis involved 102 patients.
The EST was conducted around 29 days after coronary angiography with physiological assessment (range: 20-139 days). Of these, 32 patients developed ischemic ECG changes (ischemic group), while 70 patients did not (non-ischemic group). There were no significant differences between the two groups in terms of gender, age, body mass index, cardiovascular risk factors, NYHA functional class, mean fractional flow reserve (> 0.90 in both groups), exercise time, or the presence of exercise-induced angina during EST.
All patients in the ischemic group had CMD, while 66 % of patients in the non-ischemic group also had CMD (P < 0.001). Additionally, 63 % of patients in the ischemic group had impaired CFR (< 2.5) compared with 43 % of patients in the non-ischemic group (p = 0.066). On the other hand, 97 % of patients in the ischemic group had impaired AChFR (≤ 1.5) compared with 56 % of patients in the non-ischemic group (p < 0.001).
Coronary endothelium-dependent microvascular dysfunction, but not coronary endothelium-independent microvascular dysfunction, was associated with ischemic ECG changes during exercise. When AChFR ≤ 1.5 was added as a reference standard for obstructive CAD to determine the specificity of EST, the default false positive rate of EST decreased from 31 % to 0 %.
Ischemic ECG changes during EST showed excellent specificity in detecting endothelium-dependent microvascular dysfunction. However, the combination of ischemic ECG changes during EST and/or exercise-induced angina exhibited excellent sensitivity and positive predictive value for detecting CMD but demonstrated poor specificity and negative predictive value.
Critical reading and the relevance for clinical practice
Recently, there has been a significant change in how ischemic heart disease is diagnosed and assessed. The research focus has shifted from simply detecting obstructive coronary lesions to confirming the physiological basis of myocardial ischemia.
This study assesses the accuracy of the non-invasive diagnostic test, EST, against modern standard references for CMD.
The key findings of the study are as follows (Figure 1):
- Ischemia during EST showed 100 % specificity in detecting CMD in ANOCA patients.
- AChFR (or endothelium-dependent CMD) emerged as the strongest predictor of ischemia during exercise.
The study highlights that, when compared against the physiological assessment of coronary circulation rather than the presence of obstructive coronary lesions, the specificity and positive predictive value of EST are significantly improved. Moreover, the study suggests that angina experienced during an EST actually demonstrates low specificity for the underlying ischemic substrate. Therefore, previous acceptance of angina as a positive result in studies may have contributed to the low specificity of the EST.
The study also emphasizes the physiological significance of the acetylcholine test in assessing patients with ANOCA. It suggests that AChFR, which evaluates the functionality of both endothelial and vascular smooth muscle pathways (nitric oxide-cGMP-protein kinase G pathway), compared to adenosine, could serve as a better criterion for physiological flow-mediated vasodilation. Currently, coronary computed tomographic angiography is a well-established method in the initial approach to angina in clinical practice. In cases where obstructive stenosis is confirmed to be absent in the epicardial coronary arteries, EST can be utilized as a secondary rule-in strategy for evaluating CMD.
In summary, the study's results indicate that when obstructive coronary disease is absent, a positive EST outcome strongly suggests the likelihood of CMD diagnosis and invasive microvascular physiological assessment may not be required in these instances.
When interpreting the data from this study, it's important to consider several factors. Firstly, this is a single-center study, and the findings may require validation from larger multicenter studies. Additionally, the applicability of these results to patients whose primary complaint is not angina is uncertain. The study mainly concentrates on the diagnostic effectiveness of EST, and it does not compare with other non-invasive stress imaging methods. In the future, conducting such comparisons may offer a better understanding of the diagnostic capabilities of EST.
Although it has limitations, EST continues to be a valuable diagnostic tool, especially when incorporated into a comprehensive evaluation strategy that involves invasive physiological assessment. It is important to conduct larger, multicenter studies and investigate the long-term outcomes and treatment implications based on EST findings to further enhance the role of EST in managing patients with ANOCA.






No comments yet!