Transcatheter or surgical aortic valve implantation: 10-year outcomes of the NOTION trial
Selected in European Heart Journal by N. Ryan
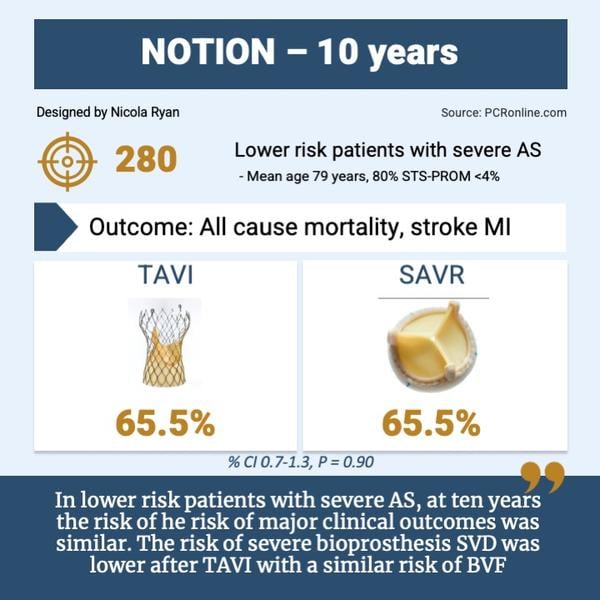
The NOTION trial provides the first ten-year data comparing clinical outcomes and valve durability between TAVI and SAVR in the lower risk population.
References
Authors
Hans Gustav Hørsted Thyregod, Troels Højsgaard Jørgensen, Nikolaj Ihlemann, Daniel Andreas Steinbrüchel, Henrik Nissen, Bo Juel Kjeldsen, Petur Petursson, Ole De Backer, Peter Skov Olsen, Lars Søndergaard
Reference
European Heart Journal, ehae043, https://doi.org/10.1093/eurheartj/ehae043
Published
07 February 2024
Link
Read the abstractReviewer
Latest contributions
Balloon lithotripsy added to conventional preparation before stent implantation in severely calcified coronary lesions Impact of pullback pressure gradient on clinical outcomes after percutaneous coronary interventions Validation of intravascular ultrasound-defined optimal stent expansion criteria for favorable 1-year clinical outcomesMy Comment
The NOTION trial was an investigator-initiated, multicentre, non-blinded clinical trial randomising patients at lower surgical risk to transcatheter aortic valve implantation (TAVI) with the self-expanding CoreValve, or surgical aortic valve replacement (SAVR) between 2009-2013.
Up to eight years follow up, no significant difference in clinical outcomes, structural deterioration or reintervention on the bioprostheses have been demonstrated.
In this study, the authors report the clinical and bioprosthesis outcomes at ten years.
Designed by Nicola Ryan
Why this study – the rationale/objective?
The development of TAVI has revolutionised the field of aortic valve intervention with TAVI, now recommended above surgery in high surgical risk, suitable moderate risk patients, and in those over the age of 75 years in current European guidelines1.
Recent registry data from the United States demonstrated that approximately 50 % of patients under the age of 65 with isolated AS underwent TAVI2. Given the increased life expectancy of younger and lower risk patients, the long-term durability of TAVI compared to SAVR is of interest.
How was it executed – the methodology?
Patients aged 70 years or older with severe symptomatic AS deemed anatomically suitable for either procedure were eligible for inclusion. Patients randomised to TAVI had first or second generation CoreValve bioprosthesis implanted, whilst the choice of a porcine or bovine stented bioprosthesis was left to the discretion of the surgeon in patients undergoing SAVR.
- The primary outcome was a composite of all-cause death, stroke or MI at one year
- In this study, the composite outcome and its components at 10 years are reported
- Key clinical endpoints of TIA, new onset atrial fibrillation, pacemaker implantation and endocarditis are reported
- Echocardiographic outcomes were the EOA of the bioprostheiss and the mean transprosthetic gradient, degree of ventral regurgitation and paravalvular leak (PVL), according to VARC-2 criteria.
- Bioprosthetic valve failure (BVF) and bioprosthetic valve dysfunction (BVD) were classified using VARC-3 criteria.
What is the main result?
Overall, 280 patients were included in the NOTION trial, of whom 145 were randomised TAVI and 135 to SAVR. Baseline characteristics were similar amongst the groups, with 47 % of patients female, with a mean age of 79.1 ± 4.8 years.
Four patients died pre-procedure, 3 TAVI patients crossed over to SAVR, and 3 SAVR patients did not receive a bioprosthesis. The as-implanted population was 274, 139 TAVI and 135 SAVR with 10-year follow up available in 98.9 %, with 101 patients alive at ten years (36.1 %). Ten-year echo data was missing in 12/52 (23.1 %) of TAVI and 7/49 (14.2 %) of SAVR patients.
- There was no difference in all-cause mortality between the two arms: TAVI 62.7 % vs SAVR 64.0 %, HR 1.0, 95 % CI 0.7-1.3, p = 0.8, when analysed by age group (< 75, 75-85, > 85) there were no differences in all-cause mortality between TAVI and SAVR.
- The primary outcome was similar in both arms (TAVI 65.5 % vs SAVR 65.5 %, HR 1.0, 95 %CI 0.7-1.3, p = 0.9) with no difference in components of the primary outcome.
- Atrial fibrillation was more common post-SAVR 20.5 % vs 13.0 %, p < 0.01, with pacemaker implantation more common post-TAVR 44.7 % vs. 14.0 % p < 0.01.
- Increased EOA and decreased mean transprosthetic gradients remained more pronounced for TAVI compared to SAVR at ten years.
- Bioprosthesis regurgitation after 10 years was more common in TAVI (25.4 % vs 2.5 % p < 0.01)
- At ten years, the risk of severe SVD was lower for TAVI (1.5 % vs 10.0 %, HR 0.2, 95 % CI 0.04-0.7, p = 0.02) and the risk of moderate or severe SVD similar between TAVI and SAVR (15.4 % vs 20.8 %, HR 0.7, 95 % CI 0.4-1.3, p = 0.30).
- Severe BVD was less common in the TAVI group (20.5 % vs. 43.0 %, p < 0.01) with no difference in BVF between groups (TAVI 9.7 % vs SAVR 13.8 %, HR 0.7, 95 %CI 0.4-1.5, p = 0.40)
Critical reading and the relevance for clinical practice
The NOTION trial provides the first ten-year data comparing clinical outcomes and valve durability between TAVI and SAVR in the lower risk population. It demonstrated that at 10 years, the rates of all-cause mortality, stroke and MI were similar between groups, with increased a.fib in SAVR patients and pacemaker implantation in TAVI patients. Severe SVD was more common post-SAVR, but rates of BVF were not significantly different between groups. Patients with TAVI had higher EOA and lower mean transprosthetic gradients which persisted to ten years but increased rates of PVL.
Despite being classified as a lower risk population, 80 % of patients had an STS-PROM score < 4 %, the mean age of enrolled patients was 79 years, perhaps explaining the relatively high mortality with only slightly over a third of patients were alive at ten-year follow up.
The new pacemaker implantation rate was significantly higher in the TAVI group, with the majority implanted in the first year post-TAVI. The rates of PVL were relatively high in this study, however were not associated with increased mortality. One must bear in mind that first and second generation self-expanding valves were implanted in this trial, evolution in valve design, delivery systems and implantation techniques have led to lower rates of PVL, conduction disturbances and vascular complications. From a SAVR perspective, the increased rates of severe BVD can in part be explained by the use of valves with externally mounted leaflets as well as a lack of use of annular enlargement techniques.
Re-intervention rates were low 4.3 % TAVI vs 2.2 % SAVR p = 0.30, (restenosis: 5 TAVI, 2 SAVR, central regurgitation 1 TAVI, 1 SAVR) with all re-do procedures TAVI. Importantly, there was no clinical valve thrombosis reported in the trial, and the rates of endocarditis was low and similar (TAVI 7.2 % vs. SAVR 7.4 %, p = 1.0).
The main limitation of this study is the small number of patients that were alive at ten-year follow up, which limits the assessment of the potential impact of increased PVL and pacemaker rates on long-term survival.
Overall, this data supports the current recommendation of TAVI in patients over the age of 75. However the lifetime management of AS remains a complex discussion, and longer term outcomes with newer generation valves as well as TAVI in SAVR and TAVI in TAVI interventions are required to understand the most appropriate treatment of aortic stenosis.
References
- A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561–632.
- Sharma T, Krishnan AM, Lahoud R, Polomsky M, Dauerman HL. National Trends in TAVR and SAVR for Patients With Severe Isolated Aortic Stenosis. Journal of the American College of Cardiology. 2022 Nov 22;80(21):2054–6.
For a more in-depth look at the subject, watch or re-watch the interview with Troels Højsgaard Jørgensen conducted by Luigi Biasco at ESC 2023!






No comments yet!