08 Jan 2025
Coronary revascularisation deferral based on quantitative flow ratio or fractional flow reserve: a post-hoc analysis of the FAVOR III Europe trial
Selected in EuroIntervention by G. Occhipinti , S. Brugaletta
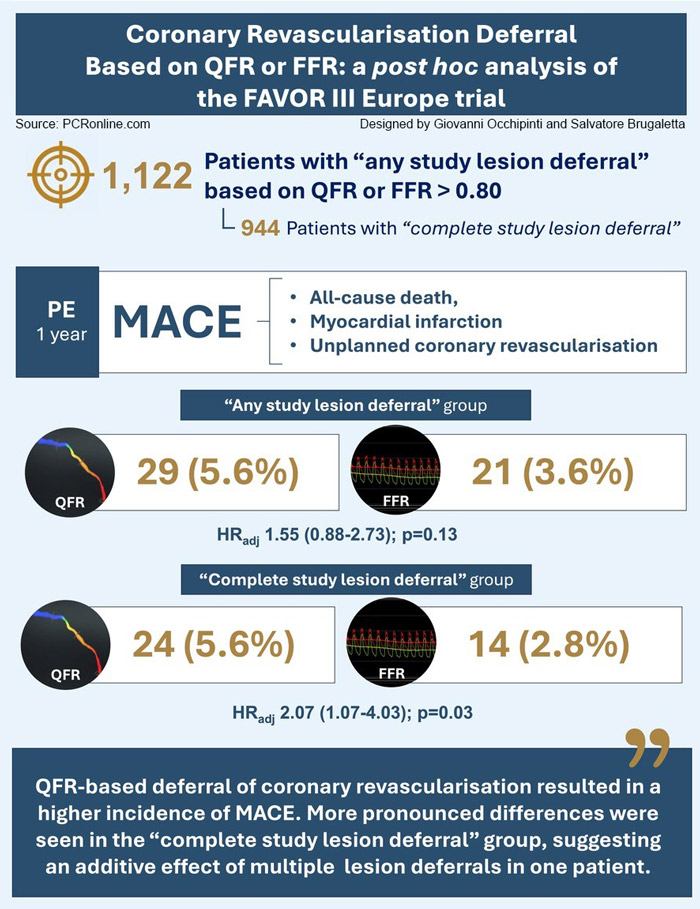
The post-hoc analysis found that quantitative flow ratio (QFR)-based deferral of coronary artery revascularisation resulted in a higher incidence of 1-year major adverse cardiac events (MACE) as compared with fractional flow reserve (FFR)-based deferral.
References
Authors
Birgitte K. Andersen, Niels R. Holm, Lone J.H. Mogensen, Luc Maillard, Truls Råmunddal, Andrea Erriquez, Evald H. Christiansen, Javier Escaned; on behalf of the FAVOR III Europe study team
Reference
DOI: 10.4244/EIJ-D-24-01001
Published
January 2, 2025
Link
Read the abstractReviewers
Our Comment
Source: PCRonline. Designed by Giovanni Occhipinti and Salvatore Brugaletta.
Why this study – the rationale/objective?
Safe deferral of revascularisation is a key aspect of physiology-guided percutaneous coronary intervention (PCI). While recent evidence from the FAVOR III Europe trial showed that quantitative flow ratio (QFR) guidance was inferior to fractional flow reserve (FFR) guidance, it remains unknown if QFR might have a specific value in revascularisation deferral.
How was it executed – the methodology?
The FAVOR III Europe trial was an investigator-driven randomised, multicenter, open-label, controlled trial conducted at 34 European centers.
All patients had at least one intermediate non-culprit coronary stenosis (40-90 % diameter stenosis by visual estimate) with an indication for physiology-guided revascularisation. For the aim of this post hoc sub-analysis, patients randomised in the FAVOR III trial in whom PCI was deferred in at least one coronary artery, based on QFR or FFR > 0.80, were included.
The primary outcome was 1-year rate of major adverse cardiac events (MACE), defined as all-cause death, myocardial infarction (MI) or unplanned coronary revascularisation. Secondary endpoints included the individual components of MACE, target vessel failure (TVF), subclassifications of MI, and revascularisation at 1 year.
The results were reported for two subsets of deferred patients:
- any study lesion deferral (at least one study lesion was deferred),
- and complete study lesion deferral (all the study lesions were deferred).
What is the main result?
A total of 523 patients (55.2 %) in the QFR group and 599 patients (65.3 %) in the FFR group had at least one coronary revascularisation deferral. Of these, 433 patients (82.8 %) and 511 (85.3 %) patients, respectively, had complete study lesion deferral.
- In the “complete study lesion deferral” patient group, the occurrence of MACE was significantly higher in QFR-deferred patients (5.6 %) as compared with FFR-deferred patients (2.8 %) (adjusted hazard ratio [HRadj] 2.07, 95 % confidence interval [CI]: 1.07-4.03; p = 0.03).
- In the “any study lesion deferral” patient group, the occurrence of MACE was 5.6 % in QFR-deferred patients vs 3.6 % in FFR-deferred patients (HRadj 1.55, 95 % CI: 0.88-2.73; p = 0.13).
- Unplanned revascularisation was the biggest contributor to the total MACE rate (“any study lesion deferral”: 3.7 % vs 2.4 %, HRadj 1.52, 95 % CI: 0.76-3.04; p = 0.23; “complete study lesion deferral”: 4.0 % vs 1.8 %, adjusted HRadj 2.21, 95 % CI: 0.98-4.96; p = 0.06).
Critical reading and the relevance for clinical practice
In line with the main analysis, the present post-hoc analysis shows that PCI-deferral based on QFR results led to higher MACE, questioning its safety in identifying non-functionally significant lesions. The more pronounced differences were seen in the “complete study lesion deferral” group, suggesting an additive effect of multiple lesion deferrals in one patient.
Although, from a statistical standpoint, these results are hypothesis generating, some arguments deserve discussion. The first one is about reliability of a QFR negative value in a real-world setting. While QFR analysts were required to complete the vendor’s training and certification process, a lower diagnostic accuracy compared to earlier validation studies is highly probable, as recently reported in non-randomized studies on the topic.
Consistent misclassification between QFR and FFR has been also reported among patients presenting with acute coronary syndrome (especially ST-elevation myocardial infarction), those with high index of microvascular resistance, or those with borderline FFR values.
To account for this high variability, current analysis explored the outcomes of a hybrid “grey zone” strategy with deferral based on a QFR threshold that ensures a high negative predictive value: no definitive conclusions were derived, leaving the debate alive, and opening for further investigation.
In addition, the role of the different diagnostic performance based on anatomical lesion location emerged for PCI deferral, with more right coronary artery lesions and fewer circumflex coronary artery/obtuse marginal branch lesions found to be deferred by QFR than by FFR.
Another important point is lack of data about medical treatment at baseline and follow-up: it may be hypothesized that a complete deferral strategy could have led to a variation in the pharmacological treatment for secondary prevention, potentially influencing occurrence of events.
This may be supported by the open-label nature of the study, as treating physicians unblinded to the patient treatment may have been influenced not only in choosing medical treatment but also in asking non-invasive ischemia studies or a repeated coronary angiography within the study period. Primary endpoint included indeed any unplanned revascularisation rather than ischemia-driven revascularisation of the deferred lesion.
Future studies are urgently needed to evaluate the reliability of angiography-derived functional assessment tools compared to FFR and explore their potential to advance clinical practice in both deferring and indicating coronary revascularisation.






1 comment
I respectfully disagree with the characterization of these findings as “hypothesis-generating.” The results show that QFR was inferior to FFR with regard to the primary outcome, given the significantly higher occurrence of MACE in QFR-deferred patients. The angiography-derived group had twice the risk of experiencing the primary endpoint compared to those in the wire-based group.