Optical coherence tomography to guide percutaneous coronary intervention of the left main coronary artery: the LEMON study
Selected in EuroIntervention Journal by M. Kovacevic , D. Milasinovic
The aim of the LEMON study was to assess the applicability of a predefined standardized protocol, which included three OCT runs.
References
Authors
Nicolas Amabile, Grégoire Rangé, Geraud Souteyrand, Matthieu Godin, Mohamed Mehdi Boussaada, Nicolas Meneveau, Guillaume Cayla, Frederic Casassus, Thierry Lefèvre, Radwane Hakim, Imane Bagdadi, Pascal Motreff, Christophe Caussin
Reference
10.4244/EIJ-D-20-01121
Published
June,11 2021
Link
Read the abstractReviewers
Our Comment
Why this study? – the rationale/objective
Intracoronary imaging guidance for LM PCI is gaining increasing attention and its use has gone from 30 % to 50 %, according to recent data from the British Cardiovascular Intervention Society1.
However, most of the evidence base comes from studies utilizing IVUS rather than OCT.
Recently, observational data from the ROCK I trial showed the superiority of OCT over angiography guidance in distal LM PCI2.
The here presented pilot study evaluated the feasibility and safety of OCT-guided left main stem (LMS) PCI.
How was it executed? – the methodology
The LEMON study (Left Main Oct-guided iNterventions) is a prospective, multicenter, open-label, interventional, non-randomized trial that investigated the feasibility of OCT guidance for LMS PCI. The trial included 70 patients with mid/distal LMS or ostial LAD or LCx (Medina 0.1.0 or 0.0.1) and with SYNTAX score < 23. Patients with ostial LMS, STEMI, and cardiogenic shock were excluded.
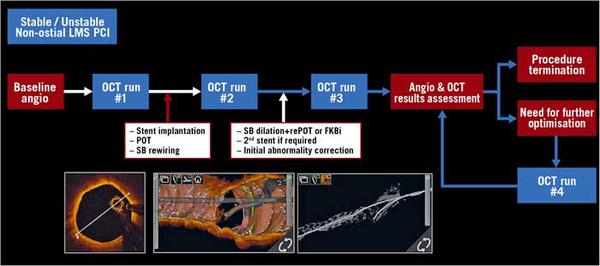
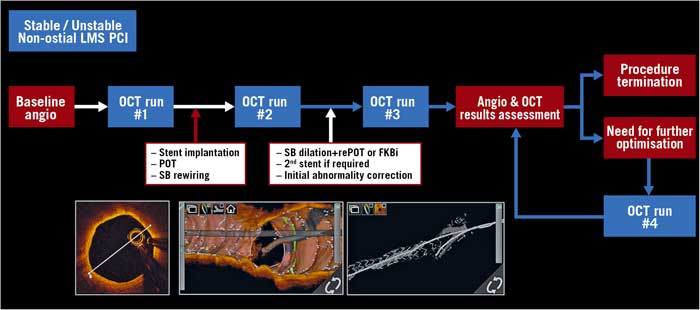
The aim of the study was to assess the applicability of a predefined standardized protocol which included three OCT runs (first run was performed before lesion predilatation, the second run was performed after stent implantation, POT, and rewiring, and the last run was performed at the end of the procedure, after the stent optimization).
The primary endpoint was procedural success, defined as Thrombolysis In Myocardial Infarction (TIMI) 3 flow in all vessels + residual stenosis < 50 % by QCA + adequate stent expansion according to LEMON criteria (Prox MSA/ref MLA & Dist MSA/ref MLA ≥ 80 %, with the carina as a level of stent division to proximal and distal segment).
Secondary endpoints included: 30-day and one-year incidence of major adverse cardiovascular events (MACE: a composite of cardiovascular death/stent thrombosis/target vessel revascularization), percentage of appropriate wire position on the second OCT run, stent expansion according to DOCTORS and ILUMIEN III criteria, contrast agent volume and radiation dose (safety endpoints).
Source: EuroIntervention Journal
What is the main result?
The primary endpoint, adequate stent expansion according to LEMON criteria, was achieved in 86 % of subjects, although when evaluated according to DOCTORS and ILUMIEN III criteria, this number significantly reduced to 40 % and 37 %, respectively.
Residual significant strut malapposition was noticed in 24 % of the cases (13 % in the proximal part) with a significant reduction of malapposed struts between the post-POT OCT run and the final OCT run (51 % vs. 19 % in the proximal and 30 % vs. 11 % in the distal segment, p < 0.001).
Concerning the secondary endpoint, the rate of one-year survival free from major adverse clinical events was 98.6 % (97.2-100).
According to the core lab analysis, wire position after the second OCT run was inappropriate in 19 %, which influenced wire repositioning in 15 % of cases.
In total, OCT guidance modified the operators’ strategy in 26 % of the patients (in every fourth patient).
Critical reading and the relevance for clinical practice
The LEMON study is considered to be the first one to report the feasibility of OCT-guided mid/distal LM PCI according to a predefined standardized protocol.
Although this protocol allowed complete assessment of LMS with the first OCT run for proper stent or balloon selection, there was a surprisingly high percentage of malapposed struts after the second, post-POT OCT run (51 % in proximal and 30 % in distal segments), with a reduction in the final OCT run (to 19 % and 11 % in proximal and distal segments, respectively) and with residual strut malapposition in 24 % of cases.
Furthermore, even with the standardized OCT protocol, 14 % of patients still did not reach the prespecified criteria for optimal expansion according to LEMON criteria, and even more when defined by DOCTORS or ILUMIEN III criteria.
Multivariable analysis revealed that larger proximal reference EEL/EEL diameter was a predictor of inadequate stent expansion.
When assessing achievement of different MSA cut-off values among the bifurcation segments, it was noticed that the most difficult was to achieve cut-off MSA in ostial LAD (only 63 % of patients had MSA ≥ 6.3 mm2 in LM-LAD stent direction) and in ostial LCx (75 % of patients had Cx MSA ≥ 5 mm2 in LM-LCx stent direction). The possible explanation could be in the SB opening technique in provisional single stent technique (83 % of patients) which in the majority of cases was done with POT/side/rePOT (64 %), thus influencing less ostial LAD or LCx optimization.
The main message of this paper is that standardized OCT guidance is feasible and safe in mid/distal left main PCI and moreover very useful since it influenced the modification of operator decision in ¼ of patients. However, randomized trials are necessary to answer the question of whether OCT guidance may improve clinical outcomes as well.
References
- Kinnaird T, Johnson T, Anderson R, Gallagher S, Sirker A, Ludman P, de Belder M, Copt S, Oldroyd K, Banning A, Mamas M, Curzen N. Intravascular Imaging and 12-Month Mortality After Unprotected Left Main Stem PCI: An Analysis From the British Cardiovascular Intervention Society Database. JACC Cardiovasc Interv. 2020 Feb 10;13(3):346-357. doi: 10.1016/j.jcin.2019.10.007. PMID: 32029252.
- Cortese B, Burzotta F, Alfonso F, Pellegrini D, Trani C, Aurigemma C, Rivero F, Antuña P, Orrego PS, Prati F. Role of optical coherence tomography for distal left main stem angioplasty. Catheter Cardiovasc Interv. 2019;1–7.








No comments yet!