Treatment of coronary bifurcation lesions, part I: implanting the first stent in the provisional pathway. The 16th expert consensus document of the European Bifurcation Club
Selected in EuroIntervention Journal by D. Milasinovic
Part I of the 16th EBC consensus document presents a detailed analysis of possible pitfalls associated with each step of the provisional single stent approach and it provides a compendium of the pertinent strategies for rescue and prevention. Also included in this review: lead author Remo Albiero provides answers to some burning questions!
References
Authors
Remo Albiero, Francesco Burzotta, Jens Flensted Lassen, Thierry Lefèvre, Adrian P. Banning, Yiannis S. Chatzizisis, Thomas W. Johnson, Miroslaw Ferenc, Manuel Pan, Olivier Daremont, David Hildick-Smith, Alaide Chieffo, Yves Louvard, Goran Stankovic
Reference
DOI: 10.4244/EIJ-D-22-00165
Published
15 May 2022
Link
Read the abstract
Reviewer
My Comment
Historically, European Bifurcation Club (EBC) consensus documents have offered comprehensive overviews of percutaneous coronary bifurcation treatment strategies and have laid the foundation for a step-by-step approach to bifurcation PCI that is grounded in the idea to replicate the underlying bifurcation anatomy.
Such a systematic approach, while ensuring progress in understanding how to adapt different stenting strategies to the realities of bifurcation anatomy, has also resulted in a cumulative experience of potential pitfalls at each step along the way.
The 16th EBC consensus document is a precedent among other EBC consensus documents inasmuch as it, for the first time, provides an extensive list of pitfalls, solutions, and prevention strategies for each step of bifurcation PCI.
Part I of the document concentrates on implantation and optimization of the 1st stent, which is how a great majority of bifurcation PCI procedures are completed. Part II focuses on different techniques of the 2nd stent implantation when necessary and their respective optimization steps.
In the introduction to Part I of the 16th EBC consensus document, the authors revisit the rationale for the general recommendation to proceed with provisional side branch (SB) stenting strategy in most cases, i.e. starting with the intention to treat the patient with a single stent, which is largely built on the follow-up data from randomized trials suggesting excessive mortality risk in patients treated with 2 stents.
In addition, the authors point to the parity of one- vs. two-stent strategies in the shorter term, across a spectrum of bifurcation anatomy, and up to true left main bifurcations with a short CX disease (the EBC MAIN trial).
Part I describes in detail how to manage and prevent potential complications in
- A) wiring,
- B) lesion preparation
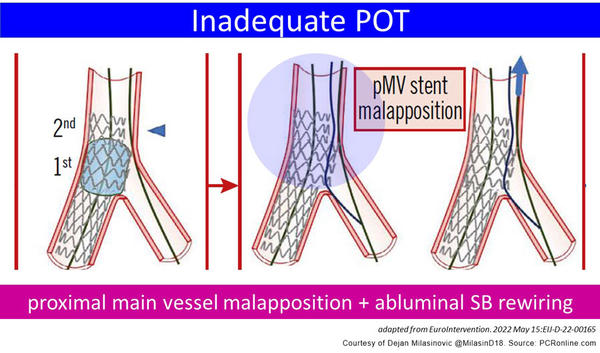
- C) and during first stent implantation and its optimization, assigning a pivotal role to the correct technique of proximal optimization (POT) (See Figure).
Wiring
- Recognize difficult SB access based on
- 1. angulation
- 2. presence of calcifications
- 3. and severity and the extent of stenosis.
- Overcome difficulties in wiring by modifying the tip shape and with the use of dual-lumen microcatheters.
- Prevent wire wrap by promptly reacting to retrograde movement of the non-instrumented wire and/or any difficulties in advancing devices over the wire without overt intracoronary obstruction.
MV and SB predilatation
- SB lesion preparation appears to be advocated in cases of angulated SB with severe, long (> 10 mm) and/or calcified ostial stenosis.
- In the absence of above criterial, routine SB predilatation seems to be discouraged, as it may contribute to the risk of proximal rewiring following main vessel stenting.
First stent implantation and optimization
- The existing recommendation for standardized sizing according to main vessel distal reference diameter followed by mandatory POT, i.e. post-dilatation of the proximal stent segment with a short balloon sized according to the proximal main vessel reference diameter, is reinforced.
- Acute SB occlusion is listed as a complication of main vessel stent oversizing or too distal POT balloon positioning, with the possible remedy being rescue balloon jailing technique performed with a low-profile balloon dilataton over the jailed wire (in case a low-profile balloon cannot pass beyond the stent struts and into the SB, the use of a Corsair Pro microcatheter to create space between the MV stent and the vessel wall, is advocated).
- Inadequate POT results in proximal main vessel malapposition and enhances the risk of abluminal rewiring of the side branch (See Figure). If balloon dilatation is performed over such abluminal SB wire, it distorts the main vessel stent by pushing its struts towards the main vessel lumen. To remedy it, first a re-POT over the correctly positioned MV wire is recommended, followed by intraluminal SB rewiring via a double lumen catheter. Of note, X-ray stent enhancement technology or intracoronary imaging may be used to confirm the wire position in relation to the MV stent at any stage of the procedure, ideally prior to any SB ballooning.
- Increase of stent length in the proximal segment following overexpansion with a POT balloon is a new phenomenon recognized in bench tests and confirmed by OCT in patients. It needs to be taken into account especially when treating the left main, due to possible strut protrusion in the aorta.
- Longitudinal stent deformation caused by guiding or extension catheter interaction with the proximal stent edge may be prevented by timely catheter disengagement when retracting devices from the coronary tree and by avoiding deep intubation once left main has been stented.
Conclusion
In summary, Part I of the 16th EBC consensus document presents a detailed analysis of possible pitfalls associated with each step of the provisional single stent approach and it provides a compendium of the pertinent strategies for rescue and prevention.
Questions to the lead author
Remo Albiero agreed to answer Dejan Milasinovic's questions to go even further!
One of the main risks of the provisional single strategy may be the acute side branch occlusion. Bearing this in mind, how do you see the role of SB predilatation in true bifurcations?
SB predilatation in true bifurcation is recommended in “complex” true coronary bifurcation lesions (CBL): SB stenosis >90%, long SB lesion length >10 mm, severe ostuial SB calcification, bifurcation angle >75 degrees). In contrast, when dealing with a CBL that does meet the DEFINITION criteria for complex lesions, we recommend predilating only the MV toward the branch receiving the first stent, in order to facilitate the rewiring of the SB through a distal strut, close to the carina. This should ensure adequate stent expansion while minimising the risk of ostial dissection of the SB and subsequent difficulty in rewiring.
Proximal optimization is central to adapting the main vessel stent to the fractal geometry of coronary bifurcations. How should inadequate POT and consequent abluminal SB rewiring be avoided and/or checked for in routine practice?
Inadequate POT is the result of: 1) proximal 2nd POT not performed (indicated when the pMV stent is longer than the POT balloon length) or 2) Proximal 2nd POT performed incorrectly with a POT balloon too small and/or too distal. To avoid an inadequate POT, and the consequent risk of abluminal SB rewiring, we suggest large use of enhanced angiographic visualisation (to increase precision of POT balloon positioning) in routine practice and optimal POT balloon sizing.
At which step(s) of provisional SB strategy do you think a growing use of intracoronary imaging may be expected?
A growing use of intracoronary imaging (IVUS/OCT) may be expected in case of suspected abluminal SB rewiring to confirm the wire position. In addition, during provisional LM stenting to confirme optimal stent expansion and apposition.
EuroIntervention Twitter discussion
#EIJonAir 12 - The 16th EBC consensus document https://t.co/h2hxBpp3Ki
— EuroIntervention (@EuroInterventio) June 21, 2022







No comments yet!