EBC MAIN Late-breaking trial analysis
Selected in European Heart Journal
Examination of the study methodology and results according to the PICOT principle, SWOT analysis and real-world applicability of the EBC MAIN trial presented at EuroPCR 2021.
References
Authors
David Hildick-Smith, Mohaned Egred, Adrian Banning, Philippe Brunel, Miroslaw Ferenc, Thomas Hovasse, Adrian Wlodarczak, Manuel Pan, Thomas Schmitz, Marc Silvestri, Andreis Erglis, Evgeny Kretov, Jens Flensted Lassen, Alaide Chieffo, Thierry Lefèvre, Francesco Burzotta, James Cockburn, Olivier Darremont, Goran Stankovic, Marie-Claude Morice, Yves Louvard
Reference
ehab283
Published
May 2021
Link
Read the abstractMy Comment
Examination of the study methodology and results according to the PICOT principle

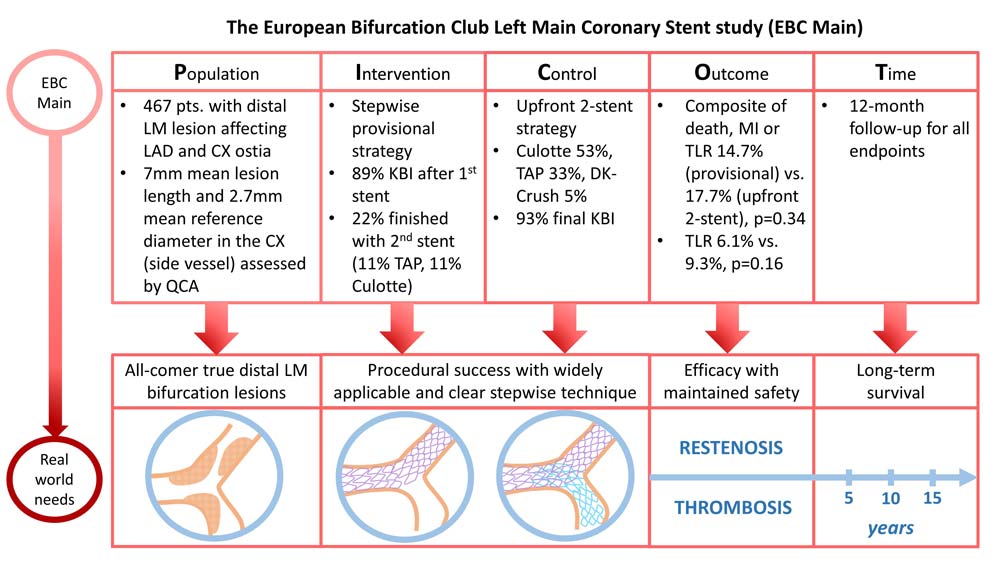
Population of interest:
- 467 patients with true unprotected left main (LM) bifurcation disease (Medina 1,1,1 or 0,1,1) with a side vessel reference diameter > 2.75 mm were randomly assigned to a stepwise provisional strategy or an up-front two-stent strategy.
- Included patients were symptomatic, with documented ischemia (non-invasive testing or invasively measured fractional flow reserve) or a LM intravascular ultrasound (IVUS)-derived minimum luminal area (MLA) < 6 mm2.
- The mean age was 71 ± 10 years, 77 % were male and 28 % were diabetic.
- Two-thirds of patients were treated electively.
- Exclusion criteria: included Acute ST-elevation myocardial infarction, cardiogenic shock, chronic total occlusion, patient life expectancy < 12 months or known allergies.
Intervention of interest:
- Stepwise provisional strategy with mandatory POT (85 %), kissing balloon inflation (89 %) and final POT (81 %).
- After mandatory kissing balloon inflation, no further treatment to side vessel unless TIMI flow < 3, severe (90 %) ostial pinching or > type A dissection.
- 22% required a bail-out 2nd stent, with either Culotte (11%) or T / TAP (11%).
Control:
- Upfront systematic two-stent strategy, with the technique left to the discretion of the operator: Culotte (53 %), DK-Crush (5 %), T or TAP (33 %).
- Kissing balloon mandatory (95 %) +/- final POT (84 %).
Outcomes of interest:
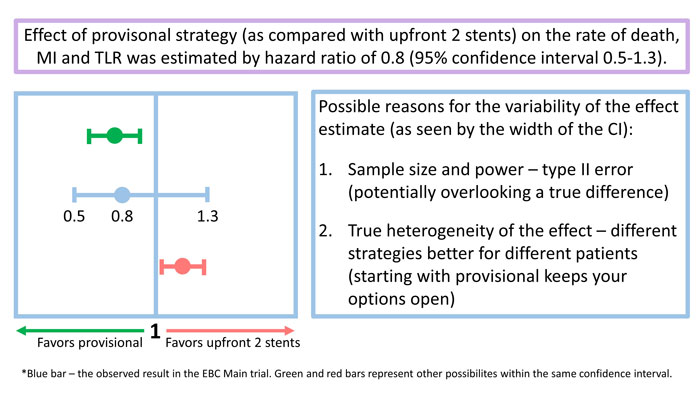
- Composite endpoint of all-cause death, any MI, and TLR was similar: 14.7 % (provisional) vs. 17.7 % (2-stent) (HR 0.8 [0.5–1.3], P = 0.34)
- There was no difference in secondary endpoints: death (3 % vs. 4.2 %), MI (10 % vs. 10.1 %), TLR (6.1 % vs. 9.3 %; p = 0.16) or stent thrombosis (1.7 % vs. 1.3 %)
Time frame of interest:
- Follow-up was 12 months for all endpoints.
Strengths – Weaknesses – Opportunities – Threats (SWOT) analysis
Strengths
- Randomized study with a well-defined methodology and technical strategy (stepwise provisional versus upfront systematic two-stent).
- The techniques used in both arms reflect daily practice in different centres: Culotte, T/TAP, DK-miniCRUSH.
- The primary endpoint selected (a composite of all-cause death, myocardial infarction, and target lesion revascularization at 12 months) reflects daily practice.
Weaknesses
- This was a superiority study with overall neutral results. While the assumed rates of the primary endpoint were 25 % in the upfront 2-stent group and 14 % in the provisional group, the actually observed rates were 17.7 % vs. 14.7 %, respectively. This may have two implications:
- Firstly, the statistical power may be less than originally planned, thus increasing the risk of the type II error (overlooking a true difference between the two groups).
- Secondly, the originally assumed large difference in favour of provisional (absolute reduction of 11 %) may have biased the study towards neutrality by decreasing the sample size.
- 467 patients were randomized at 31 centres over a period of 45 months: potentially, this could have led to an uneven distribution with very few patients per centre, raising the question of selection bias. On the contrary, there is a lack of information concerning the overall number of patients with true distal LM bifurcation disease treated with PCI during the same period in the enrolling centres.
- Only 85% of patients had appropriate cardiac enzyme measurement, which may have implications for the assessment of periprocedural MI, a component of the primary endpoint.
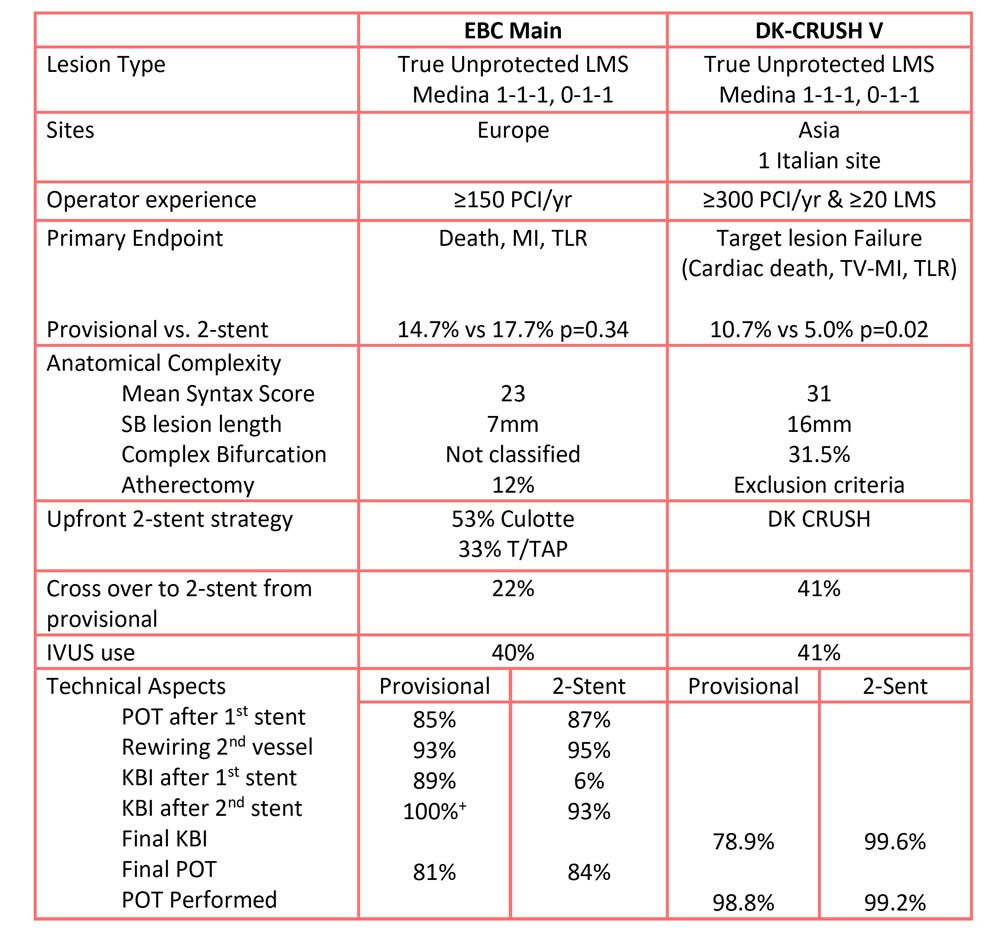
- The 1-year adverse event rate was markedly higher when compared to the similarly designed DK-Crush V trial (15 % vs. 18 % in provisional vs. 2-stent in the EBC Main and 10 % vs. 5 % in the DK-Crush V), although the overall coronary artery disease complexity seems to have been lower (mean syntax score 23 in the EBC Main vs. 31 in the DK-Crush V).
- Operators were expected to be undertaking ≥ 150 PCI procedures per year (compared to > 300 in DK-Crush V). Therefore, potentially lower experience of some operators in complex LM PCI could have influenced the high rate of primary endpoint events.
- In addition, formal requirements in terms of experience with LM PCI in general and planned 2-stent techniques in particular, were not reported in the EBC Main trial, whereas in the DK-Crush V trial, only operators who had performed 3-5 adjudicated DK Crush procedures were allowed enroll patients.
- Nevertheless, the latter two points may mean wider applicability of the EBC main trial results, as it may better reflect real-world practice.
- In the EBC Main trial, there was a numerically slightly lower technical success in the provisional approach compared to the systematic dual stenting approach driven mainly by failure to adhere to the protocol mandated POT, rewiring of the side branch, and final kissing balloon. Given the recognized benefit of POT, the longer-term outcomes, particularly in those in whom POT was omitted, will be of interest.
- Intracoronary imaging was not mandated, and rates were low within both trials, likely reflecting real-world practice. The rates of further optimization post IVUS in EBC Main appear relatively low (12 % vs 6 %); however, it may reflect operators sizing stents and carrying out initial post-dilatation based on pre-PCI IVUS.
- In general, given the neutral results of a superiority trial, one may question the conclusion that the provisional approach should remain the philosophy of choice in the majority of left main stem true bifurcation procedures, especially as no information is provided regarding the number and anatomical characteristics of the patients screened but not included in the study.
Opportunities
- This trial gives the interventional cardiology community confidence that the stepwise provisional single stent strategy is safe in carefully selected patients with true bifurcation left main stem lesions.
- Adopting a stepwise provisional stent strategy preserves the option of implanting a 2nd stent, which was needed in 22 % of the patients in the EBC Main trial. The results of the EBC Main trial may encourage such an approach, which may result in the overall fewer patients being treated with a 2-stent strategy (itself known to be a predictor of stent-related events including stent thrombosis).
- However, this objective requires that interventional cardiologists with limited experience in the field of LM bifurcation procedures (patients with LM stem lesion represent around 4 % to 6 % of patients with symptomatic coronary artery disease) develop a self-critical reflection on both this EBC LM trial and the DK Crush trial.
Threats
- On the contrary, this trial and the comments raised in the paper could stimulate interventional cardiologists to pursue the stepwise provisional single stent strategy in the majority of patients presenting with complex lesions affecting the distal LM. Thereby, it should not be forgotten that the EBC Main trial was not designed to compare one vs. two stents and that it did not show non-inferiority of the one-stent approach. This was rather a superiority trial, which showed neutral results of a provisional strategy that entailed a 2nd stent in at least one-fifth of the cases versus an upfront 2-stent strategy that comprised Culotte and T/TAP technique in over two-thirds of patients.
- In terms of practical applicability, it is important to keep in mind that there may not be side branches in the sense of clinical unimportance when treating left main disease; embryology studies showed that there are two main branches (LAD and LCX, which themselves give side branches), that in the majority of people meet in a common LM stem to the aorta. So, everyday procedural logic would entail treating a severely diseased and large epicardial coronary artery (such as CX) with a stent if unsatisfactory results with a balloon dilatation only are achieved.

Comparison of EBC MAIN vs. DK CRUSH V
Related links
- EuroPCR 2021 Hotlines / Late-Breaking Trials in bifurcation lesions: EBC MAIN and more!
- EBC Main: Behind the curtain
- EBC MAIN trial results – what is new and what will change in left main stenting?
- The European Bifurcation Club Left Main Study (EBC MAIN): rationale and design of an international, multicentre, randomised comparison of two stent strategies for the treatment of left main coronary bifurcation disease





No comments yet!