20 Aug 2019
Rotational atherectomy in anterior STEMI
Euro4C Case
Author
Let’s exchange opinions on this case. This could happen to you tomorrow…
Patient’s history
- 83-year-old woman with arterial hypertension, hypercolesterolemia
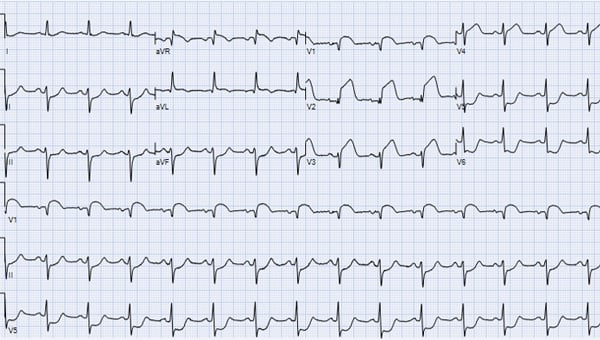
- Onset of continuous chest pain at rest with anterior STEMI on ECG
- Medicated with ASA and Ticagrelor and transferred to the cathlab
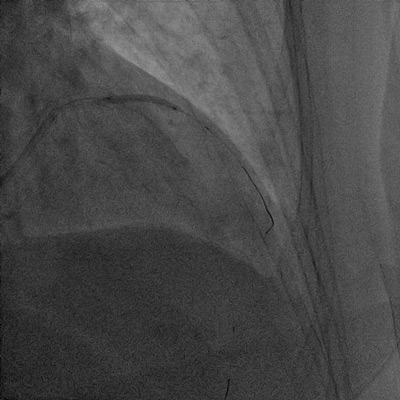
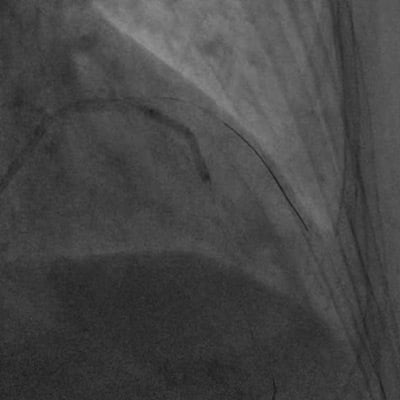
Urgent coronary angiography: non culprit lesion
Urgent coronary angiography: culprit lesion
- Proximal LAD sub-occlusion with severe calcifications
PCI strategy
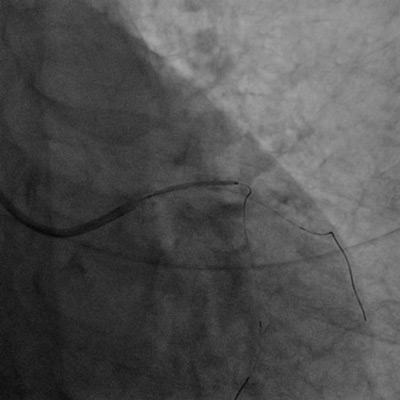
- LAD and D1 wiring
- Failure to cross the lesion with 2.0 x 20mm semi compliant balloon

- Emergency surgery (this would be a very last option)
- Try smaller balloon (maybe, but balloon may not dilate)
- Remove the guide-wire from the diagonal branch and try again with the same or a smaller balloon (same as above)
- Shock wave balloon (may not cross the lesion)
- Remove the guide wire from the diagonal branch and try rotational atherectomy (this is our approach).
PCI strategy
- Re-positioning a side wire on the diagonal branch
- LAD dilatation with 2.5 mm and 3.0 mm NC balloons


Side-branch dilation with 2.0 mm semi compliant balloon
Proximal LAD stenting with 3.0 x 22 mm DES
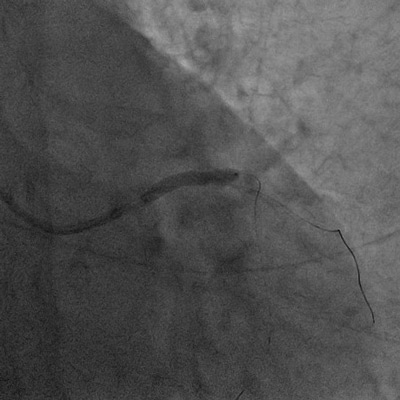
Proximal LAD stenting with 3.0 x 22 mm DES
Mid LAD dilatation with 2.5 mm NC balloon
Final result
Post-procedural ECG
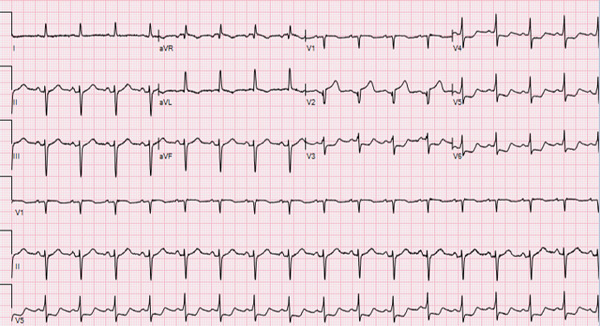
Post-procedural ECG
- Echocardiography: LVEF 45%, anterior and apical hypokinesia
- Uneventful hospital stay
- Patient discharged on day 7 on DAPT for 12 months
- Three years follow-up uneventful with EF improvement to 58%
Key learning messages
- Patients presenting with STEMI may have calcified, undilatable lesions.
- Rotational atherectomy can be used in this emergency setting.
- Appropriate step by step technique may offer a good result also in STEMI.
- Training of the emergency interventional team is crucial to perform safely the RA procedure in a non-elective setting
- Adequate stent expansion is crucial to reduce the risk of stent thrombosis and restenosis.
"Few situations are more “psychologically demanding” in our daily work than that of felling obliged to open a large LAD in a patient with recent onset of a large STEMI. Similarly, frustration in case of failure in this context is a huge burden for the operator and the team, but more important, could also have dismal consequences for the patient.
Nasty calcifications may put the whole cathalb team to test in an emergency like the one we presented in this case. Your comments largely underscore the importance of this clinical situation that we wanted to share.
Again, the way we faced and solve it is one among others but the one we are confident with. Good planning based on a simplified strategy and experience with the use of RA even in a non-elective context are key, and this is what we wanted to share. Certainly, as with any other technique, substantial training of the operators and the whole team is crucial to achieve this level of confidence with the device.
Our next case is certainly controversial under many points of view….. We share this with the hope of fueling a lively and likely passionate discussion…"
Flavio Ribichini for Euro4C






12 comments
This is an everyday life emergency PCI situation that should not be left to a beginner, but needs tuition from a senior operator...
Very important issue, can happend every night and every weekend!
Case: 83y female with anterior STEMI in progress due to heavily thrombo-calcified prox. LAD lesion with large co-dominant LCX. Discussion with heart team. The patient has already treated with ASA and Ticagrelor. According to guidelines ticagrelor should be discontinued at least 24 h before urgent on-pump CABG (Class I) due to high (x6) bleeding risk. I always load with ADP inhibitors after the diagnostic part. Based on that we should try 1st with PCI having as a 2nd option the emergent CABG. You need a cardiac anesthesiologist, heart surgery team and IABP/Impella to be standby or in place in case of hemodynamic compromise. If you are a beginner you NEED support. Access: I would prefer the transfermoral. TF approach can lead to better support than the transradial approach along with the option of larger caliber catheters with more back-up characteristics. PCI : I would try several attempts with smaller SC balloons (1.5 or 1.25mm) or balloons like Sapphire II PRO. RA: Rotational atherectomy is relatively contraindicated in the setting of acute coronary thrombosis such as STEMI because of the risk of potential platelet activation by the rotablator. However there are many acute cases in the literature where RA was successfully used in such thrombo-calcified lesions. Therefore, in our case may be considered. However, there is a high risk for slow flow, burr entrapment or perforation. Therefore, the Rotafloppy wire must in good distal position and you should use small 1.25mm burrs. Temporary transvenous pacing wire: must be in place due to the risk of developing high-grade AV block. Microcatheter: may need for guidewire exchange. DES: Single-stent crossover technique from ostial-prox LAD to distal UPLM. Heparin: ACT must remain above 300s throughout the procedure by checking it every 30 min.
Nice case, Flavio! And you are right, can occur anytime. My thoughts on this: Straightforward interventional in 84y and STEMI. As you had managed to get in a 6F radial sheath in this old lady I would have switched to a 7 F sheathless (same outer diameter) considering that LAD is diseased up to the ostium. Offers more backup and space for bifurcation stenting in case LM gets hurt. The diagonal I would not even have wired as ostium looks nice and no prognostic impact from mid-diagonal PCI (even though it is a large vessel and I might change my mind if flow does not improve after LAD-PCI). But as 6F is already in place and two wires and a balloon have entered LAD I would have proceeded with bare rota floppy wire instead of this is diagonal wire, and then retracted the LAD-wire so option to use microcatheter remains if there were issues with rotawire passage. I would not expect to need Impella. First run with 1,25mm burr should improve flow quickly, then step up to 1.75. Shockwave balloon would be nice to have instead of 1.75mm burr as it promises better lesion preparation. But it cannot replace the 1.25mm burr as its profile is too large. And for stenting I expect that single stent with POT would suffice for LAD/ALA and another single stent plus POT for LAD-LM.
Very hard case, especially if occurring in the middle of the night! I would try to pass and dilate a smaller balloon, if the flow in both LAD and diagonal improves and the st elevation reduces, even if larger balloon does not expand properly, I could start thinking about stopping the procedure after this "minimal POBA" and bring the patient again on the table after 24 h of heparin infusion aiming to perform rotablation, in order to reduce risks of emergent rotational atherectomy in the acute thrombotic setting.
Nice case, tough, however, although the use of rotablation in acute MI is off label, it can be used when there are no other options. In view of the potential existence of thrombus and the increased risk of slow flow, I would definitely start with small burr 1.25 mm at low rpm, 140000. After that I would stop rotablating and I would try a 2.0 mm non compliant balloon in order to improve distal flow. If this doesn't cross or doesn't dilate the lesion I would repeat rota with no more than 1.5 mm burr again at low speed, trying to leave longer intervals between the passages of the burr in order to release the flow and decrease the chances of now reflow. I would use ic nitroprusside more freely provided BP is stable. Then I would use a 2.5 mm noncompliant balloon and if this crosses and dilates the lesion I would continue in the conventional way. If not, I would consider the 1.75 mm burr again at slow speed. This is called balloon assisted rotablation and is pretty usefull and safe in cases like this, where there is increased risk of slow flow due to increased thrombotic burden.
Definitely I would try any option but RA. My experience with RA in primary PCI is limited only to 2 cases where I had to finish using it, but they were two cases of activation of the Code Infarct which they were not actually STEMI and they were calcified lesions in patients with NSTEMI. The only case of real STEMI that I saw when I was a fellow finished in a complete disaster with TIMI 0 flow in a large LAD with no options of restoring better flow. My stepwise approach would be: 1. Smaller balloons of 1.0 with low profile as the mentioned Shapiro II. 2. Try to change the wire to a Grand Slam with a Caravel microcatheter. 3. Remove the wire of the diagonal. 4. Corsair or Turnpike microcatheters. Only after failure of all these attempts I would consider RA, and as has been pointed out, if it were possible to improve the ischemia and program the RA in a less thrombotic situation, I would prefer it.
Real-life case Flavio! Absolutely agree with you: this is not a case for a beginner. Many arguments could be discussed before the procedure. But the best is enemy of the better. I mean, at the point we are with the data you shared with us a 6F GC, LAD-D1 disease with TIMI flow 1-2 and two wires in an STEMI patient on DAPT treatment I think it makes no sense to switch to a femoral approach, to call surgeons, wait 5 days, etc. We should think the better for the patient. And that is to restore as son as posible the flow in both arteries. As we have definite thrombus I will leave the 2 wires and try a smaller balloon (1.25 or 1.5 mm) I will use up to a 3.0 mm balloon. If the balloons did not expand properly, hoping the flow has been improved after balloon dilatation, I will try with a cutting-balloon in this case. In this case, I´ll only will use RA if smaller balloons did not advance. If a balloon equal or greather tan 2.0 mm advance, surely the role of a larger rotablation burr will not be enough. Shockwave? We got it. However, none have data concerning its safety in this setting. As bail-out situation everything could help, but I will not use it.
I have a similar case , but i think there is a Poor soport , si necesary to change ángel Extra backup system o AL. And use NC Ballons with stepimg size
Great learning case.
Fantastic result. Definitely it is neccessary to see that someone else has tried cases like this one. I have to congratulate you for the case. I still think I would only approach it with RA if there is not any other chance and I would also do it with the smallest burr. My concern still is how to forsee the behavior of the flow before performing the RA.
Do you concern about no flow after rotational atherectomy during primary PCI? How to prevent no flow in this situation?