13 Jan 2025
Precision PCI in the era of AI and multimodality imaging
#CardioTwitterCase originally published on Twitter
Nailing the ostium of LAD, although technically challenging, can be precisely done with mandatory intracoronary imaging. It is essential to rule out disease extension into left main artery as, otherwise, cross over LM-LAD stenting strategy would be preferable. CTCA can help the interventionist plan the PCI, while OCT can precisely guide the positioning of the stent. Utility of such technology helps avoid "geographical miss" leading or floating struts in LM, which could be a nidus for future complications.
This case was originally published on Twitter by @FBardooli
Case description
This is the case of a 55 years old lady, known to have dyslipidemia, diabetes mellitus type 2 and hypertension on medical therapy. She presented with progressively worsening dyspnoea for the last 3 months. Her 2D ECHO showed preserved left ventricular function with no significant valve disease.
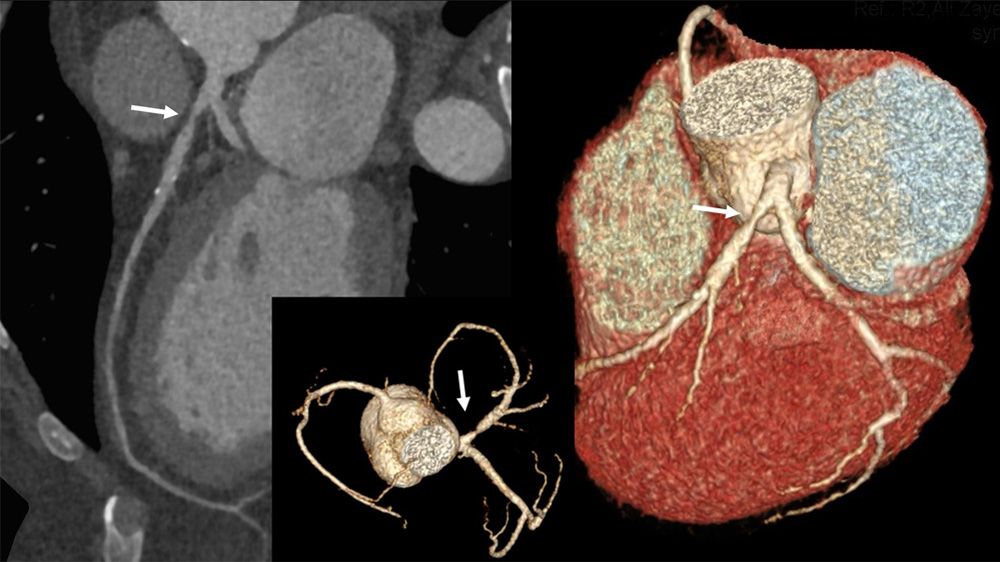
Coronary CT angiogram revealed severe proximal LAD discrete lesion, but an ambiguous proximal zone at the ostium of LAD, with regards to involvement of the LMCA involvement (Figure 1).
The challenge is to locate a healthy landing zone at the ostium of LAD with no disease extension to LM. Furthermore, as to proceed with the strategy to position the stent at the ostium with no strut protrusion into the LMCA.
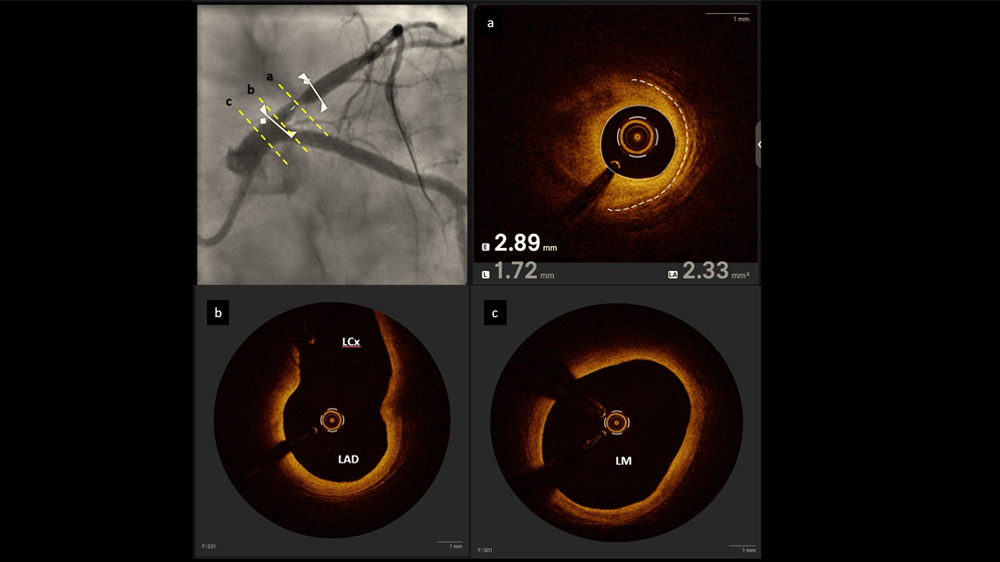
Utilising the data from the CTCA, the best angulation to visualize the ostium of LAD was selected. Subsequently, both LAD and LCX were wired, and the OCT run into LAD done showed significant lipid rich atheroma in the proximal LAD (Figure 2) with healthy ostial segment of LAD without involvement of the distal LMCA or OS of LCx.
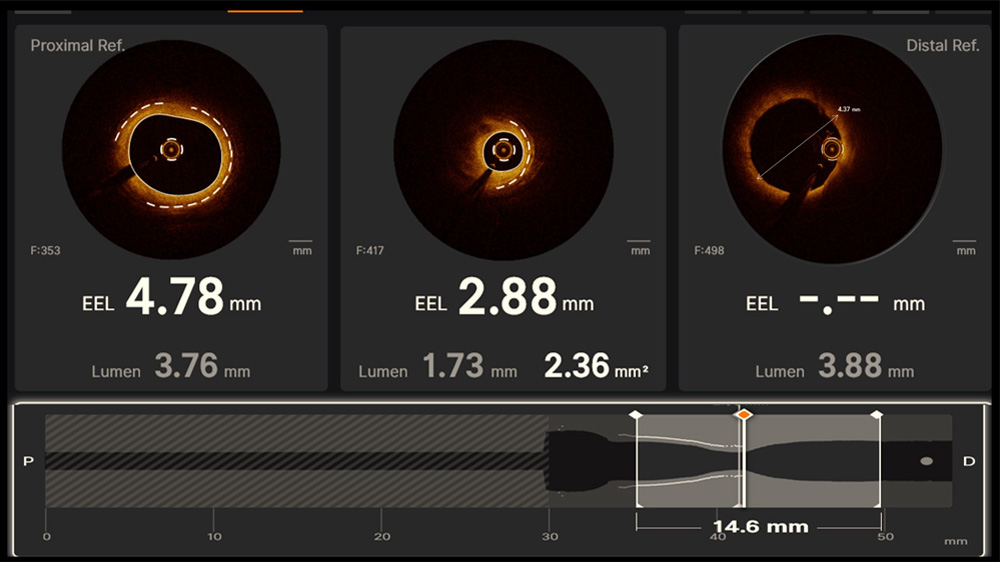
The lesion was 15 mm in length, with a vessel diameter of 4 mm in distal and 4.74 mm at proximal segment (Figure 3).
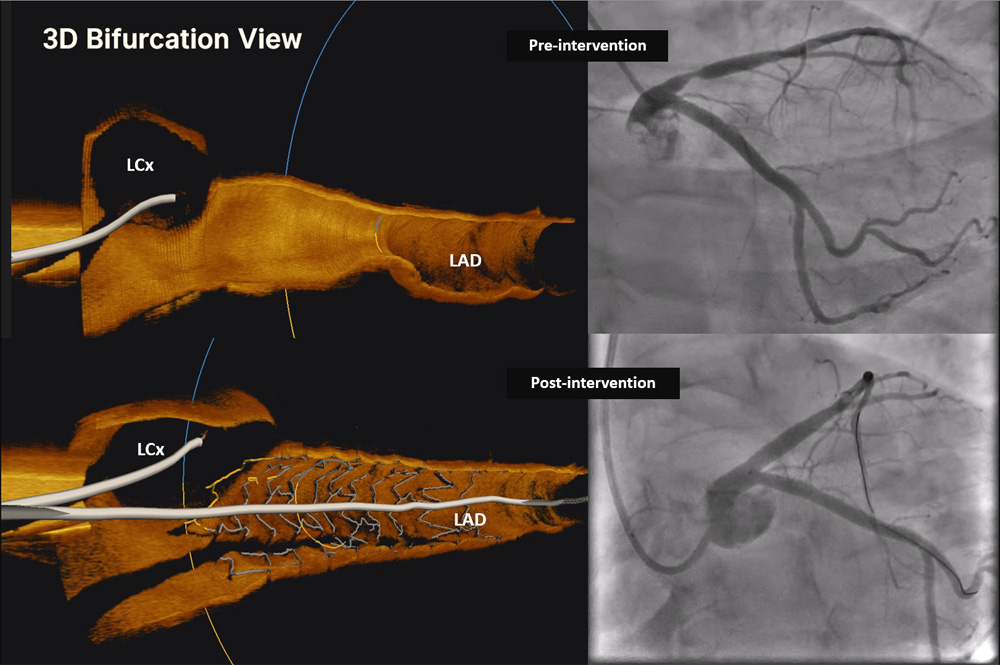
Utilising AI & co-registration in OCT, a 4.0 x 15 mm stent was placed in position (Video 1) & subsequently post dilated with a non-compliant 4.5 x 12 mm balloon.
Post PCI OCT run showed good expansion > 90 % of the stent, no edge dissection and, importantly, a good coverage of the ostial LAD (including the atheromatous plaque) with no major protrusion in the LM (Figure 4).
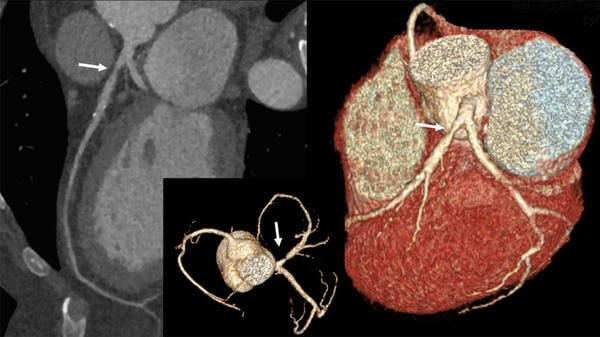
Figure 1 - Utility of the CT coronary angiogram to delineates the lesion severity and location (white arrow)
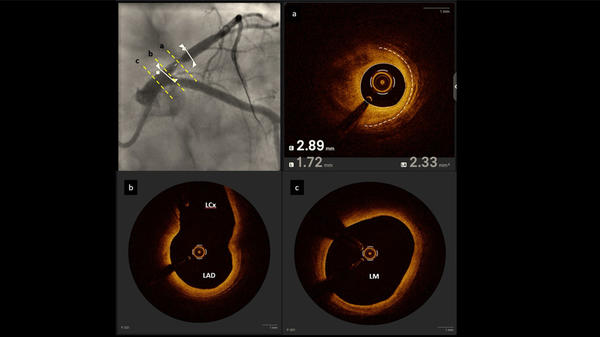
Figure 2 - Multiple cross sections at different points.
(A) showing the tightest point with area of 2.3 mm2.
(B) showing the LM carina bifurcation with Healthy ostial LCx and distal LM.
(C) showing the distal LM free from significant atheroma.
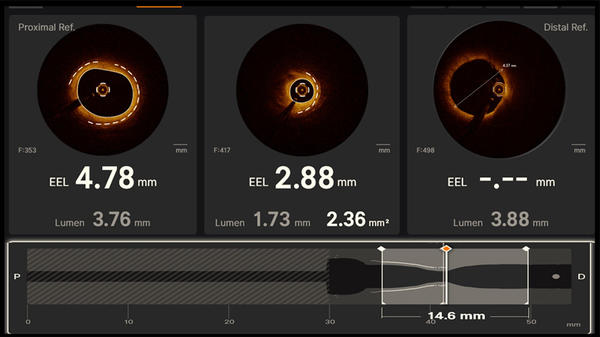
Figure 3 - Automated calculation of the EEL (external elastic lamina), Lumen diameter and length of disease segment with OCT.
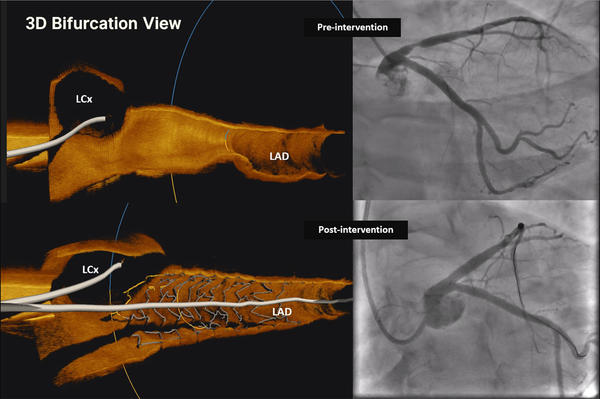
Figure 4 - Precision PCI comparing pre and post Angioplasty with 3D dimension
Final remarks
Nailing ostial lesions can be performed if indicated! Imaging modalities predict pre- and post-intervention outcomes.
Original tweet and Twitter discussion
Thanks for the votes
— Fawaz Bardooli, MD (@FBardooli) July 16, 2024
We need to clarify if Os LAD/LM are involved or not (most of the time yes)
Having multi modality imaging including CTCA and OCT helps.
Decided to nail Os but with AI using the co-registration feature pic.twitter.com/QrZ4t5Dd8R
Authors








1 comment
nice case. thanks for sharing