14 Apr 2023
ECLS: technique of implantation and/or explantation of the cannula
A problem-solving step by step tutorial
ECLS has become an important tool in the management of severe cardiogenic shock and refractory cardiac arrest, but is often complicated by bleeding ranging from nuisance to life-threatening. Therefore, deliberate management of the access site is of utmost importance.
Frequency of the problem:
Expert level:
Summary
Peripheral veno-arterial extracorporeal membrane oxygenation (vaECMO/ECLS) has become an important tool in the management of severe cardiogenic shock and refractory cardiac arrest. While different settings lead to a variety of implantation strategies, ECLS always requires large-bore vessel access to establish sufficient blood flow allowing adequate hemodynamic support. Albeit the innate hemodynamic disadvantages of the peripheral ECLS configuration (i.e. retrograde blood flow), percutaneous femoral access using Seldinger´s technique is the preferred strategy in emergency and non-surgical settings. Femoral venous plus retrograde arterial cannulation comprise the default configuration for femoro-femoral ECLS. Furthermore, the addition of an antegrade perfusion sheath is recommended.
However, ECLS therapy in cardiogenic shock and refractory arrest is often complicated by bleeding ranging from nuisance to life-threatening. Hence, deliberate access site management is of utmost importance. Starting with meticulous cannulation, acknowledging potential caveats and resulting implications regarding possible troubleshooting and explantation.
Once patients can be discharged from ECLS support, safe cannula explantation can be performed by solely applying mechanical pressure to the puncture site in most patients. Interventional approaches with per- or pre-closure and surgical explantation represent further options for individual patients. Following explantation, a vigilant follow-up is recommended to identify and prevent complications.
The problem
Once the decision to « go on pump » is made, and especially in the case of refractory cardiac arrest, time is of the essence. Urgent establishment of ECLS flow therefore competes with decisive puncture and deliberate cannula positioning. Safe placement of an antegrade perfusion sheath in cannulated limb(s) can be challenging in patients with vasculopathy and/or exposure to high doses of vasopressors.
Furthermore, ongoing resuscitation efforts (i.e. chest-compressions) or agonal/shock-related agitation might challenge operators. However, explantation starts with implantation.
Principal idea
The ideal femoral access site is located in a vessel section that can safely accommodate a 15-17(19)F arterial and 21-23F venous cannula. The arterial puncture site ought to be located ventral of the femoral-head abutment and well above the femoral bifurcation. The tip of a 15 cm long arterial cannula usually ends in the pelvic axis. However, individual anatomy might require a longer cannula (i.e. 22 cm) once in a while. The venous access site should be close to the arterial puncture, but not adjacent to it, to reduce the risk of arteriovenous fistula while allowing simultaneous compression. The entry tip of the venous cannula is preferably positioned in the superior vena cava for oxymetric reasons. The antegrade perfusion sheath is selectively positioned in the superficial femoral artery and connected to the side port of the arterial canula
Material needed
- Standard puncture needle for femoral access
- Stiff 0.035” wire
- 4F, 6F, 2 x 10F sheath
- Male-male luer adaptor
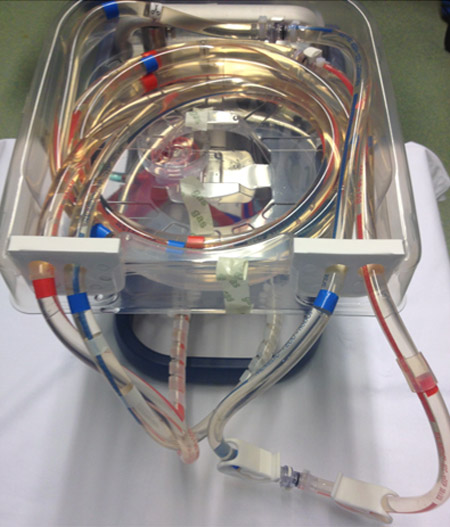
- ECLS system including circuitry and cannula
- Disposables
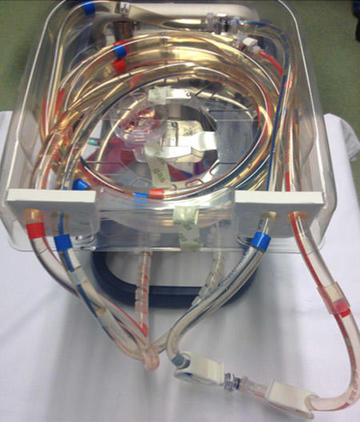
ECLS System
Method step-by-step
Step 1 - Identify suitable access site
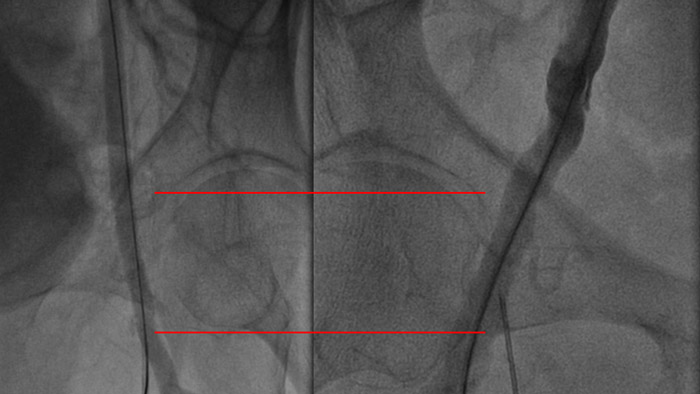
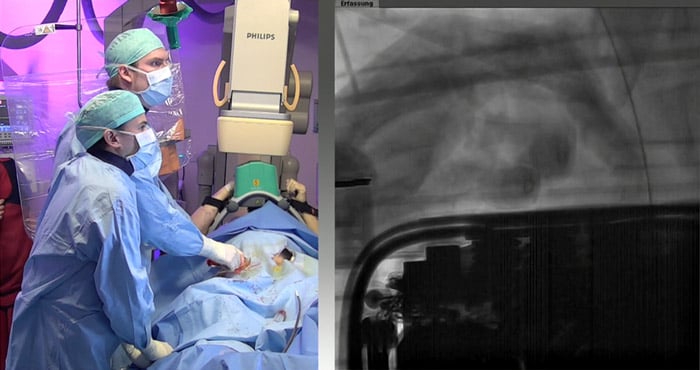
Depending on the specific setting (elective vs emergency) fluoro-anatomic landmarks and/or sonography are strongly recommended to identify a vessel section that allows safe accommodation of a 15-17(19)F arterial and 21-23F venous cannula.
The arterial puncture site should be located:
- ventral to the femoral head
- and well above the femoral bifurcation.
This enables bedside mechanical compression as a strategy for explantation/bleeding management and facilitates surgical management, use of closure devices and stenting if necessary.
Step 2 - Insert 10F sheaths
Once percutaneous femoral access is achieved, using Seldinger´s technique, a stiff wire is inserted. Although stepwise dilation is sometimes necessary, primary dilation solely with a 10F sheath prior to canula insertion is usually sufficient.

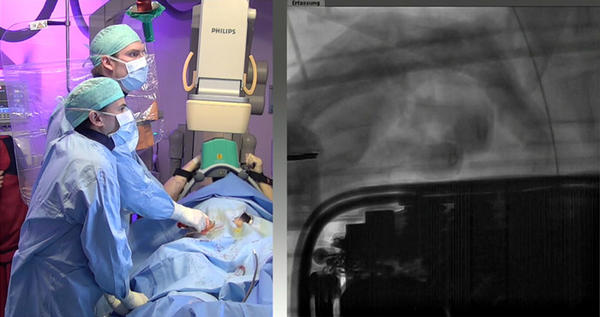
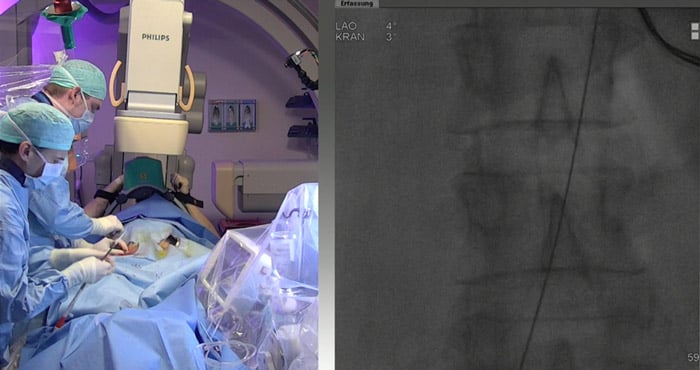
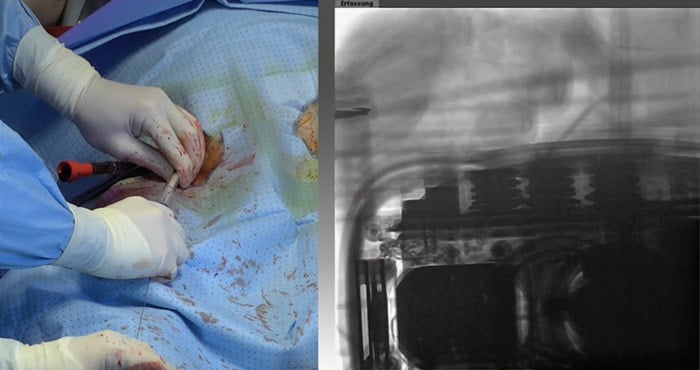
Step 3 - Confirm correct wire position
Especially in the context of extracorporeal resuscitation, fluoroscopic wire monitoring improves safety and orientation.
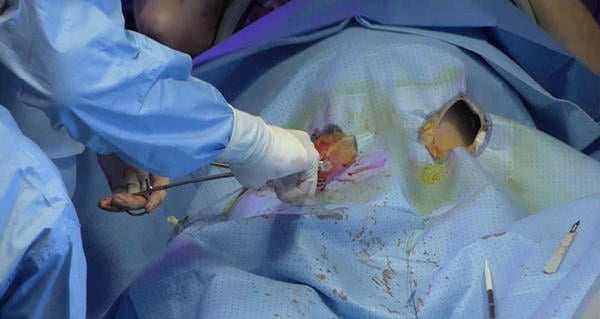
Step 4 - Use minimal incision
The skin incision prior to placement of the ECLS cannula should be kept to the minimum necessary to barely insert the cannula - excessive incisions can cause bleeding.

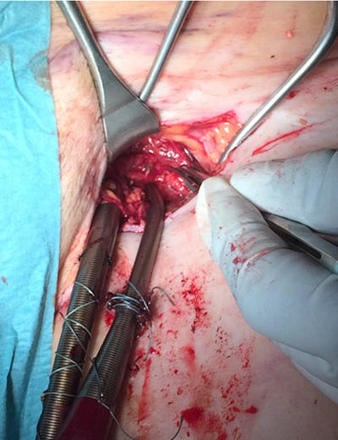
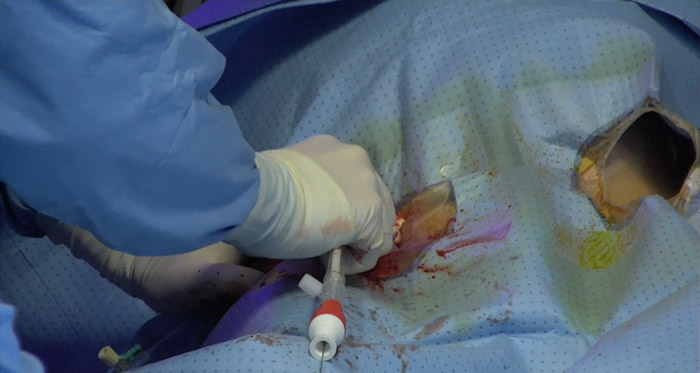
Step 5 - Insert cannula via stiff wire
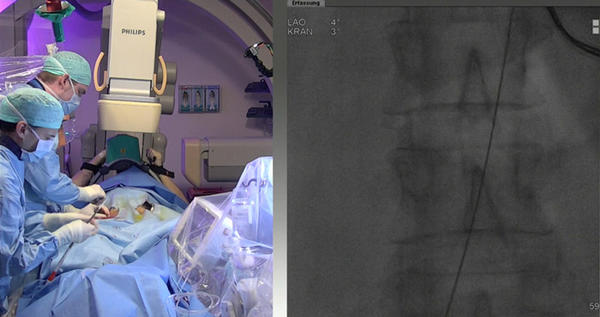
Insertion of the canula should be performed with a slight push and rotational motion under direct fluoroscopic visualisation.

Step 6 - Prepare the cannula
The cannula inlet is removed with the wire and the cannula is clamped. A syringe connected to the cannula is used to check for adequate backflow, then the cannula is deaerated and clamped again.
Step 7 - Confirm correct wire position
For correct venous-cannula positioning, the wire should be placed into the superior caval vein/axillary vein, or jugular vein.
Step 8 - Insert venous cannula
The inflow tip of the venous drainage cannula is placed in the superior caval vein. This ensures adequate drainage and allows highly deoxygenated blood from the cerebral circulation to enter the ECLS system bypassing the right ventricle.
Step 9 - Prepare the cannula
The cannula inlet is removed with the wire and the cannula is clamped. A syringe connected to the cannula is used to check for adequate backflow, then the cannula is deaerated and clamped again.
Step 10 - Establish ECLS-flow
Once ECLS circuit is connected to the cannulas, in a stepwise fashion, release the clamp on the venous line, ensure sweep-gas flow is established, start ECLS and open the arterial clamp.

Step 11 - Establish antegrade perfusion
In order to prevent critical limb ischemia, placement of an antegrade perfusion canula/sheath concludes the process of femoro-femoral ECLS implantation. In an emergency setting (“life before limb”), this can be postponed until revascularization/reperfusion is performed.
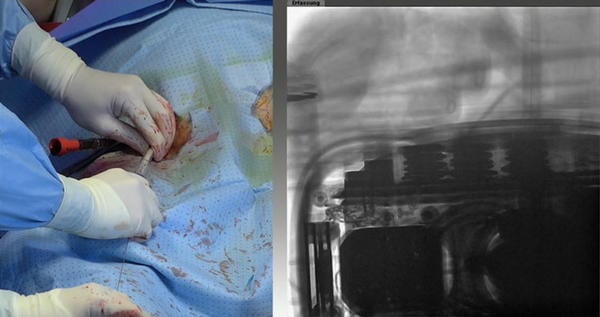
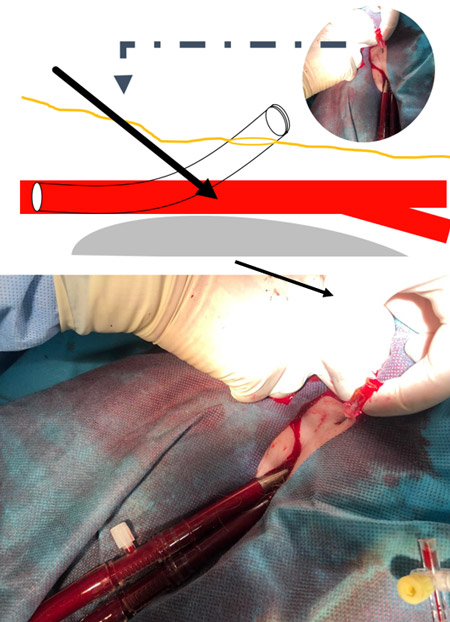
Step 11-a – Puncture site
Puncture the skin cranial to the arterial cannula insertion site and aim towards the arterial cannula to penetrate the vessel a little distal to the ECLS-cannula puncture site in the vessel.
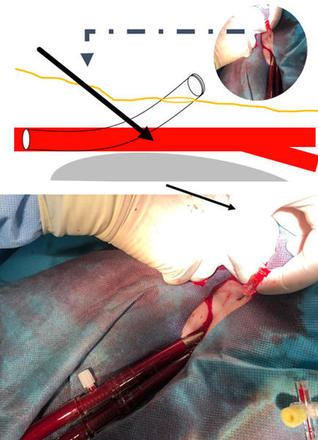
Step 11-b – Confirm position
In case of challenging puncture and/or questionable position, contrast-visualisation, using a 4F dilator, can clarify correct position in superficial femoral artery.

Step 11-c - Connect to arterial cannula side port
The antegrade perfusion cannula is connected to the arterial ECLS-cannula using a double-male luer lock adapter.

Step 11-d - Eventually repeat process...
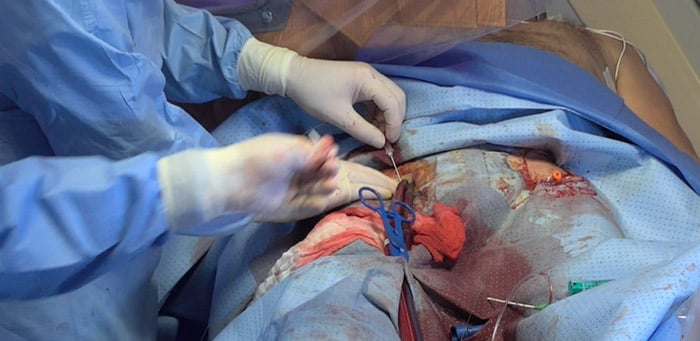
Repeat process in case of contralateral large-bore access, and, if deemed necessary, connect with 3-way stopcock and secure all cannulas and lines with sutures and robust fixation.

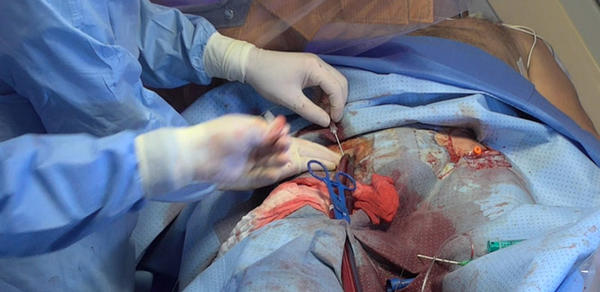
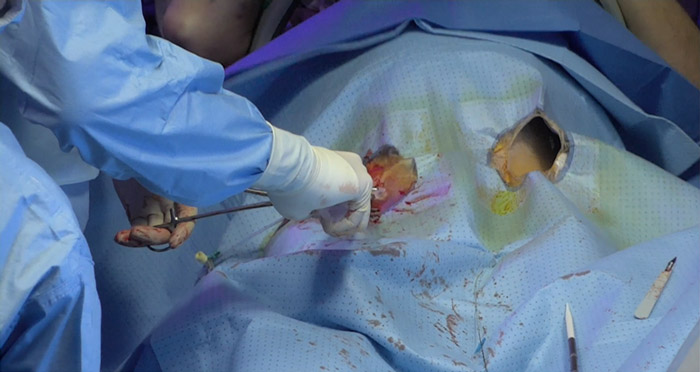
Step 12 - Explantation
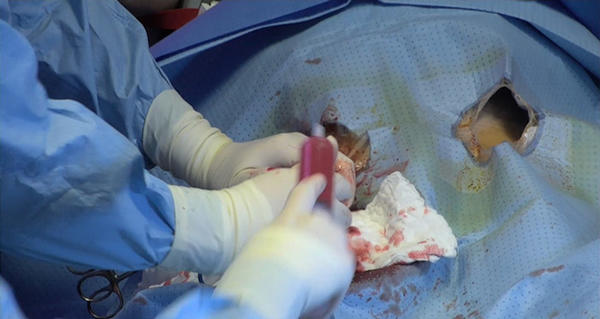
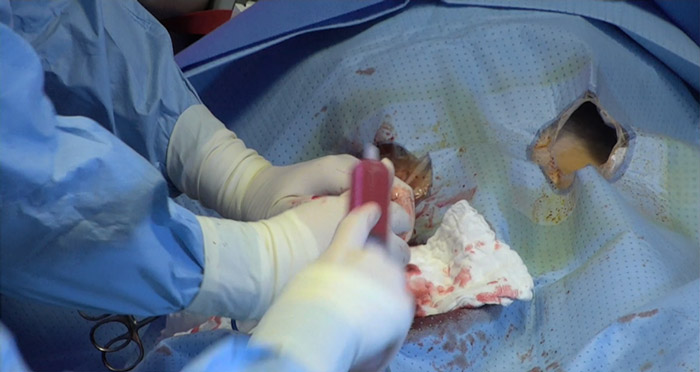
Step 12-a - Mechanical pressure
In most cases, the femoral head abutment allows safe removal using mechanical pressure devices.

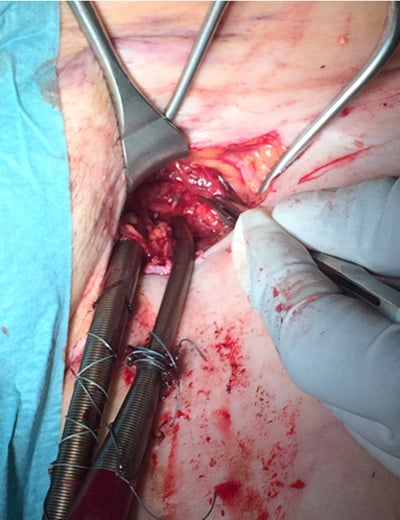
Step 12-b - Surgical and interventional management of the access site is an additional option in some cases.
Step 13 - Follow-up
After successful explantation of the ECLS, exclude complications by careful follow-up examination of the access site with sonography and/or CT.

Figure: Cannula-associated thrombosis (white arrow)
Points of specific attention
Implantation and explantation of ECLS requires specific attention to every component of the treatment concept to ensure optimal outcomes. Percutaneous femoral access using the Seldinger technique guided by fluoroscopy and/or sonography is the preferred strategy in non-surgical emergency situations.
One crucial point is the precise puncture at the level of the middle/upper third and ventral of the femoral head. This allows for emergency management in case of bleeding and removal with bedside mechanical compression.
Additionally, it simplifies surgery and use of closure devices. It also facilitates safe implementation of antegrade perfusion cannula. Proper positioning of the drainage cannula with its inflow-tip in the superior caval vein is crucial to ensure adequate venous drainage, especially of desaturated blood returning from cerebral circulation. Additionally, vigilant follow-up after ECLS liberation is strongly suggested to detect and/or handle potential complications.
A word from the reviewer - Julien Adjedj
- ECLS implantation occurs in every cathlab with or without cardiac surgery; in other words, cardiogenic shock happens to all of us.
- Therefore, the need to implant ECLS in the cathlab increased and the need to implant cannula percutaneously in the cathlab by interventional cardiologist became crucial to save the situation in short period of time.
- This toolkit summarizes how to implant ECLS in the cathlab using echo and angiography is the best way, but it should not take extra time
- It provides helpful insights for reperfusion cannula, which is the most novel part for interventional cardiologist













3 comments
Excellent step by step explanation of this too much complicated procedure...
Dear Julien, Excellent description of the work. For removal pre but also after emergency procedures post closure with proglides similar to TAVR cases works excellent both arterial and venous and reduces compression time significant.
Excellent