Transcatheter edge-to-edge repair in patients with severe mitral regurgitation and cardiogenic shock: Insights from the TVT Registry
Reported from TCT 2022
Mirvat Alasnag provides her take on the TEER Shock study which was presented at TCT 2022 by Mohamad A. Alkhouli.
Transcatheter mitral repair systems have largely been reserved for patients with a high or prohibitive surgical risk. The majority of the studies evaluated the role of mitral clip in the chronic heart failure setting.1-3 Given that 20% of shock patients have severe mitral regurgitation (MR), the role of transcatheter edge-to-edge repair (TEER) has grown in the last few years in the acute setting as well with a mounting body of evidence albeit mainly observational. The IREMMI trial was presented at TCT in 2020 and enrolled 93 patients with acute MR following a myocardial infarction (MI) and treated with MitraClip at 18 centres in Europe, North America, and Israel between 2016 and 2020.4 Only 50 presented with cardiogenic. MitraClip to treat acute MR was implanted 24 days after the initial presentation. After a median follow-up of 7 months, 16.3% died compared with 9.3% of those without cardiogenic shock (P = 0.377). The combined rate of death or rehospitalization due to heart failure was 28% and 25.6% in the patients with acute MR with and without cardiogenic shock (P =0.793). Overall, patients with significant MR during their index hospitalization for an MI had similar clinical outcomes whether they presented in or out of cardiogenic shock, provided initial hemodynamic stabilization was achieved prior to repair.
In 2021, Farwati et al reported a multivariable analysis of 639 patients with MR presenting with cardiogenic shock; 179 of whom had an acute MI.5 The overall in-hospital mortality rate was 23%, the rate was higher for shock patients with significant MR and acute MI (29.6%). The in-hospital mortality rate for those with both shock and MR but not acute MI was 20.4%. Predictors of included older age, use of mechanical circulatory support devices (MCS), end-stage renal disease and obesity.
The TEER Shock study was presented at TCT 2022 by Mohamad A. Alkhouli. The investigators extracted data from the STS/ACC TVT Registry. This is the largest cohort of patients presenting with acutely decompensated heart failure and fulfilling the definition of shock to date. It included 3797 patients with cardiogenic shock loosely defined as those requiring inotropic support, mechanical circulatory support devices or identified as such on a data collection form between November 2013 and December 2021. 73% met one criterion for cardiogenic shock, 18.9% met two and 8% met all three criteria. The mitral regurgitation (MR) etiology was degenerative in 53.4%, functional in 27.5% and mixed in 13.6%. 5.4% were reported as other. The mean age was 73 years and 59.95 were men. The STS predicted risk of mortality was 14.9%. More than one clip was necessary in 47.8% of patients. Procedural success was defined as final MR grade < 2+ (occurred in 88.2%) and MR reduction > 1 grade (occurred in 91.4%). Overall success was achieved in 85.6%. Those who developed device failure were older, had more degenerative MR and a higher prevalence of diabetes and chronic obstructive lung disease. Procedural complications included VARC major bleeding (3.6%), stroke (1.6%), single-leaflet device attachment (1.3%), and conversion to surgery (0.6%).
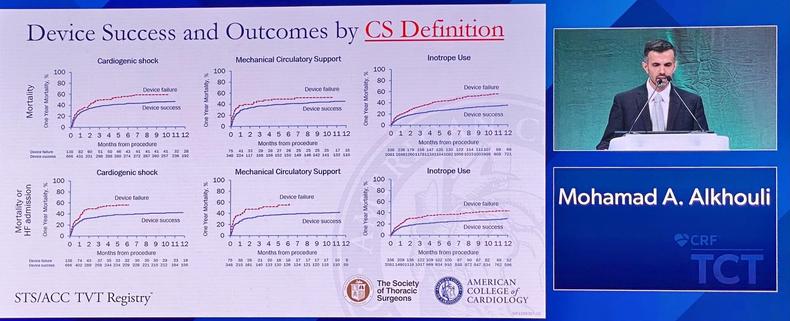
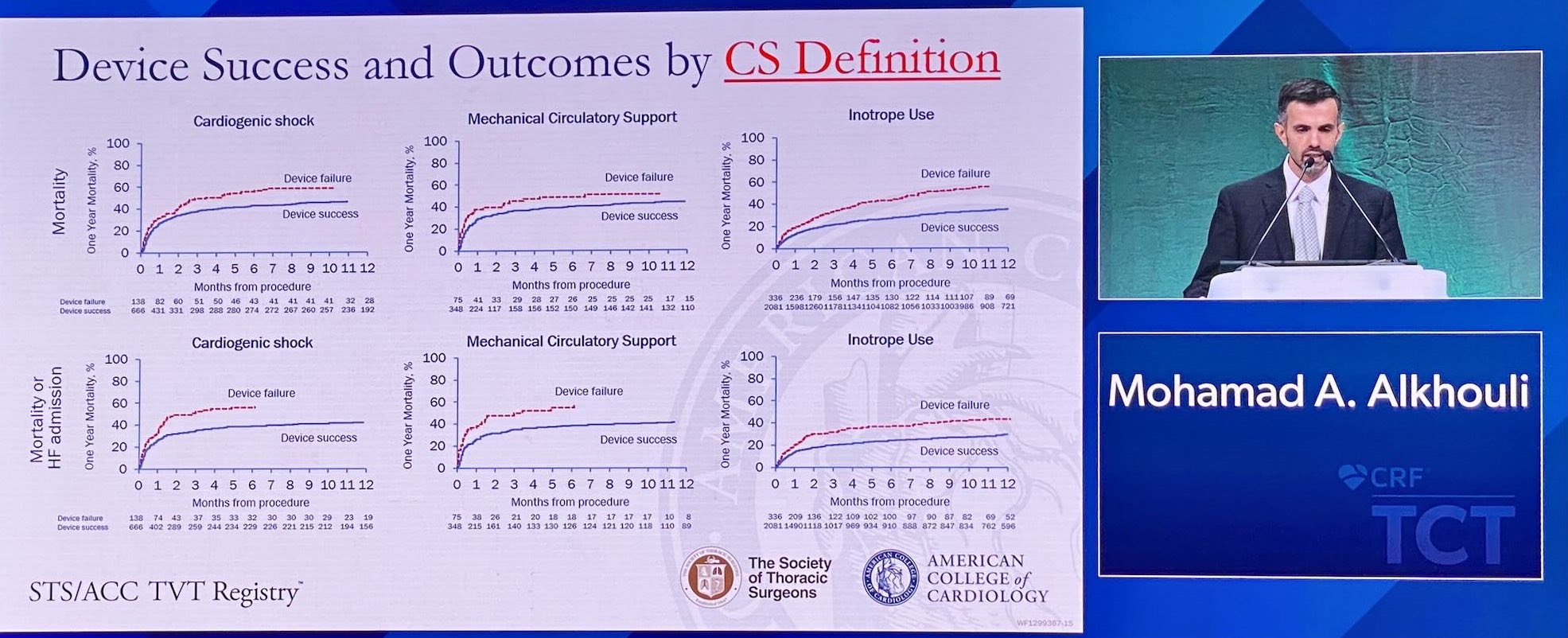
Sensitivity analysis of individual cardiogenic shock criteria and clinical outcomes at one year. Source: JACC
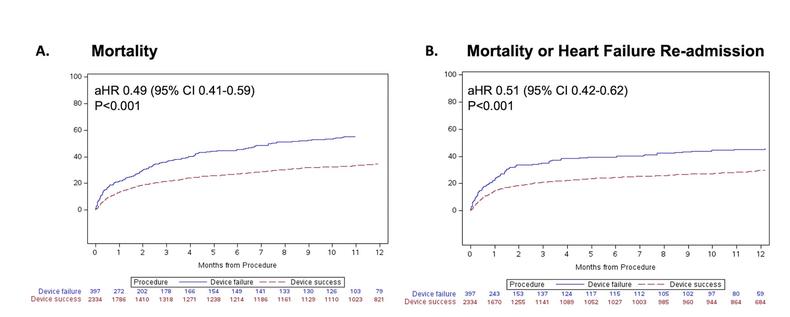
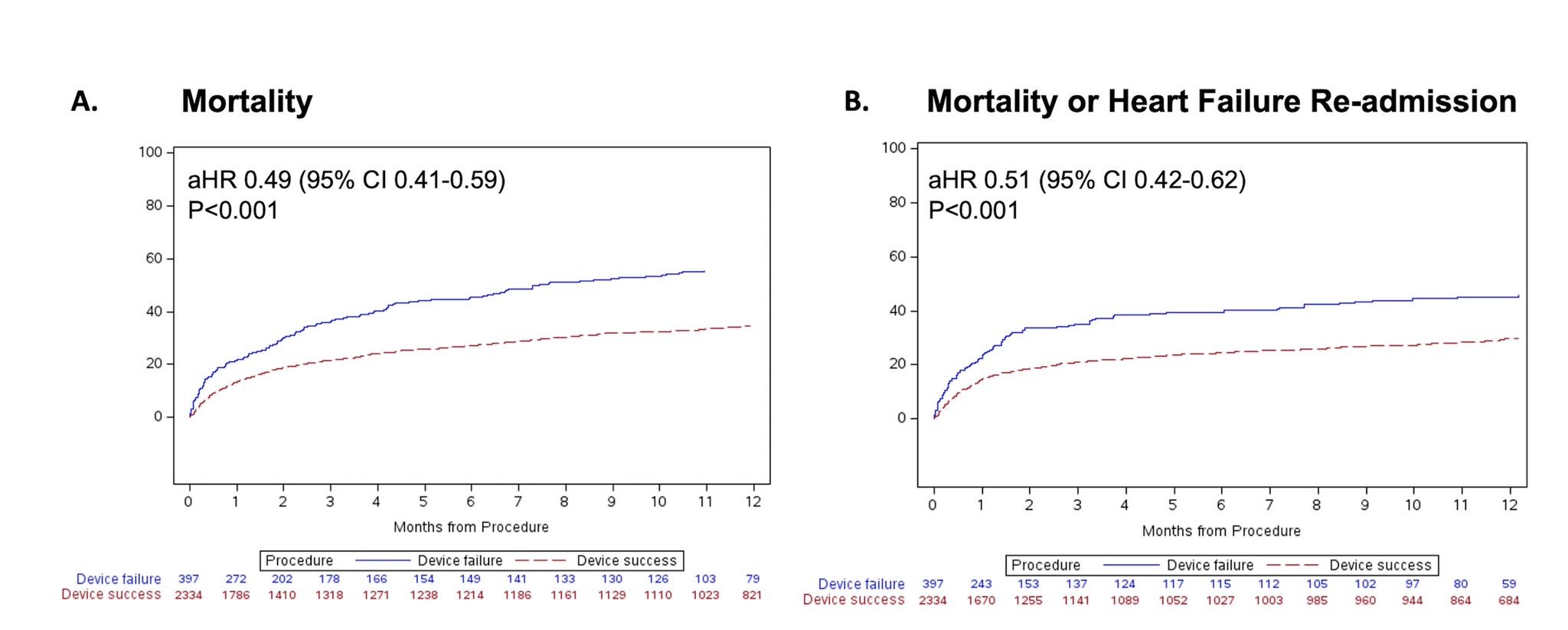
Interestingly, those with device failure had a higher LVEF (42.9% vs 40.7%) and less frequent moderate-severe or severe MR (84.9% vs 96.1%). Yet, their in-hospital mortality remained higher (16.4% vs 9.1%; P < 0.001) and length of stay was longer (14.3 vs 12.2 days; P < 0.001). The 30-day mortality in those with a successful procedure was lower than the STS expected rate (14.9% vs 13.1%). All-cause mortality was significantly lower at one year in those with a successful compared with the failed arm (34.6% vs 55.5%; 95% CI 0.41-0.59). The number needed to treat (NNT) was 4.8 to prevent death at one year. Of note, the NNT to prevent one death or heart failure hospitalization is 6.4. Heart failure readmission rates and mortality were also significantly lower in those with a successful procedure (29.6% vs 45.2%; 95% CI 0.42-0.62). Both ejection fraction and acute coronary syndrome did not impact outcomes in this study.
The results of TEER Shock are encouraging. There’s a signal towards a mortality benefit which warrants further examination. A randomized trial is important to define the shock stage, discriminate acute MI and provide a prespecified analysis by degree of MR, degree of left ventricular dysfunction (ejection fraction) and presence of critical care algorithms. With regards to the latter, Papolos et al noted in their multicenter observational study, that centers employing shock teams were more likely to obtain invasive hemodynamics, use advanced types of MCS, and had a lower risk-adjusted mortality.6 As such, critical care teams and pathways can impact survival beyond TEER.
The CAPITAL MINOS trial is a much anticipated open-label, multi-center randomized clinical trial comparing TEER on top of medical therapy to medical therapy alone in those presenting with cardiogenic shock and severe MR.7 Society for Cardiovascular Angiography and Interventions (SCAI) stage C or D shock and at least 3+ MR are used to define the enrolled population.
The primary outcome is a composite of in-hospital all-cause mortality, cardiac transplantation, implantation of durable left ventricular assist device, or discharge on palliative inotropic therapy. Secondary outcomes is mortality at 6 months. This trial, along with the aforementioned studies, will likely change the guideline recommendation. These will, of course, need to be interpreted in conjunction with results of other trials evaluating inotropic regimens such as the Capital DOREMI 2 trial; after all, shock management is a more comprehensive care plan that should integrate revascularization, hemodynamic support and TEER. Finally, a randomized trial may help define futility more specifically.
References
- Stone GW, Lindenfeld J, Abraham WT, Kar S, Lim DS, Mishell JM, Whisenant B, Grayburn PA, Rinaldi M, Kapadia SR, Rajagopal V, Sarembock IJ, Brieke A, Marx SO, Cohen DJ, Weissman NJ, Mack MJ; COAPT Investigators. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N Engl J Med. 2018 Dec 13;379(24):2307-2318. doi: 10.1056/NEJMoa1806640. Epub 2018 Sep 23.
- Kar S, Feldman T, Qasim A, Trento A, Kapadia S, Pedersen W, Lim DS, Kipperman R, Smalling RW, Bajwa T, Hermann HC, Hermiller JB, Lasala JM, Reisman M, Glower D, Mauri L, Whitlow P; EVEREST II Investigators. Five-year outcomes of transcatheter reduction of significant mitral regurgitation in high-surgical-risk patients. Heart. 2019 Nov;105(21):1622-1628. doi: 10.1136/heartjnl-2017-312605. Epub 2018 Aug 4.
- Sodhi N, Asch FM, Ruf T, Petrescu A, von Bardeleben S, Lim DS, Maisano F, Kar S, Price MJ. Clinical Outcomes With Transcatheter Edge-to-Edge Repair in Atrial Functional MR From the EXPAND Study. JACC Cardiovasc Interv. 2022 Sep 12;15(17):1723-1730. doi: 10.1016/j.jcin.2022.07.023.
- Estévez-Loureiro R, Shuvy M, Taramasso M, Benito-Gonzalez T, Denti P, Arzamendi D, Adamo M, Freixa X, Villablanca P, Krivoshei L, Fam N, Spargias K, Czarnecki A, Haberman D, Agmon Y, Sudarsky D, Pascual I, Ninios V, Scianna S, Moaraf I, Schiavi D, Chrissoheris M, Beeri R, Kerner A, Fernández-Peregrina E, Di Pasquale M, Regueiro A, Poles L, Iñiguez-Romo A, Fernández-Vázquez F, Maisano F. Use of MitraClip for mitral valve repair in patients with acute mitral regurgitation following acute myocardial infarction: Effect of cardiogenic shock on outcomes (IREMMI Registry). Catheter Cardiovasc Interv. 2021 May 1;97(6):1259-1267. doi: 10.1002/ccd.29552. Epub 2021 Feb 18.
- Farwati M, Saad AM, Abushouk AI, Bansal A, Gad MM, Krishnaswamy A, Yun J, Kapadia S. Short-Term Outcomes Following Urgent Transcatheter Edge-to-Edge Repair With MitraClip in Cardiogenic Shock: A Population-Based Analysis. JACC Cardiovasc Interv. 2021 Sep 27;14(18):2077-2078. doi: 10.1016/j.jcin.2021.04.052. Epub 2021 Jul 28.
- Papolos AI, Kenigsberg BB, Berg DD, Alviar CL, Bohula E, Burke JA, Carnicelli AP, Chaudhry SP, Drakos S, Gerber DA, Guo J, Horowitz JM, Katz JN, Keeley EC, Metkus TS, Nativi-Nicolau J, Snell JR, Sinha SS, Tymchak WJ, Van Diepen S, Morrow DA, Barnett CF; Critical Care Cardiology Trials Network Investigators. Management and Outcomes of Cardiogenic Shock in Cardiac ICUs With Versus Without Shock Teams. J Am Coll Cardiol. 2021 Sep 28;78(13):1309-1317. doi: 10.1016/j.jacc.2021.07.044.
- Parlow S, Di Santo P, Jung RG, Fam N, Czarnecki A, Horlick E, Abdel-Razek O, Chan V, Hynes M, Nicholson D, Dryden A, Fernando SM, Wells GA, Bernick J, Labinaz M, Mathew R, Simard T, Hibbert B. Transcatheter mitral valve repair for inotrope dependent cardiogenic shock - Design and rationale of the CAPITAL MINOS trial. Am Heart J. 2022 Aug 21;254:81-87. doi: 10.1016/j.ahj.2022.08.008. Epub ahead of print.





No comments yet!