BYPASS-CTCA: The value of computed tomography cardiac angiography in improving patient satisfaction and reducing contrast load, procedural duration and complications in patients who had previous CABG undergoing invasive coronary angiography
Reported from TCT 2022
Nicola Ryan provides her take on the BYPASS-CTCA Study which was presented by Daniel A. Jones at the TCT Congress 2022.
It must be understood that the paper has yet to be published for this study therefore all assumptions are based upon the presented data.
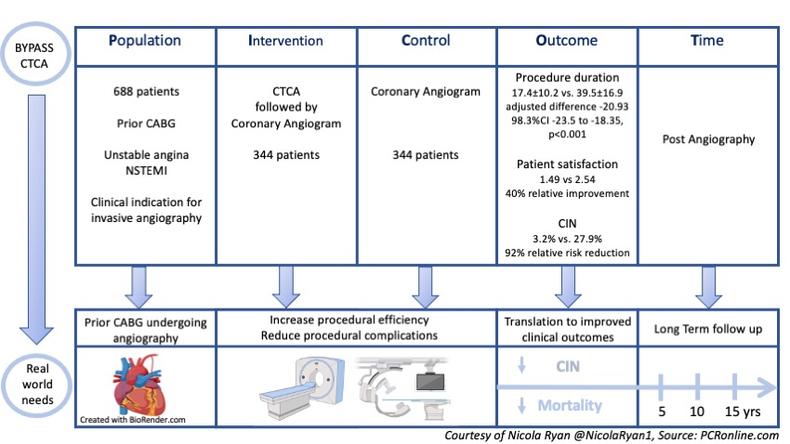
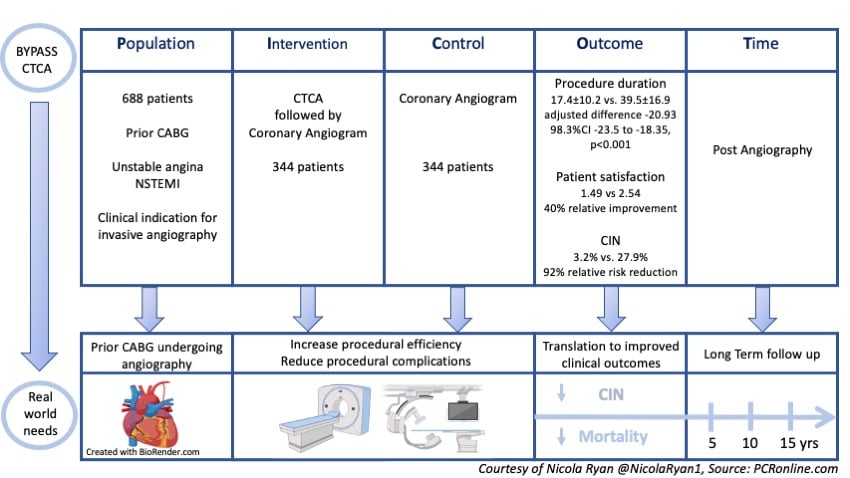
PICOT analysis of the BYPASS-CTCA study.
Courtesy of Nicola Ryan @NicolaRyan1, Source: PCRonline.com
The BYPASS-CTCA study was a randomised control trial designed to assess if adjunctive CTCA can reduce procedure time, improve patient satisfaction and prevent procedural complications in patients with prior CABG undergoing coronary angiography.
Why this study – the rationale/objective?
Coronary artery bypass grafting is frequently used to treat coronary artery disease however this leads to progression of native coronary artery disease, furthermore, surgical conduits particularly saphenous vein grafts can fail either acutely or over time. Therefore, many post-CABG patients require angiography due to either stable or unstable presentations, angiography of bypass grafts can be challenging due to unknown conduits or anatomical and technical challenges. It has been suggested that CTCA may be useful prior to angiography in patients post-CABG to reduce procedural time and contrast load (1). This trial assesses if adjunctive CTCA can reduce procedure time, improve patient satisfaction and prevent procedural complications in patients with prior CABG undergoing planned coronary angiography (ICA).
How was it executed - the methodology?
Patients with prior CABG undergoing planned angiography for stable angina and NSTEMI were eligible for inclusion. Major exclusion criteria included an eGFR <20ml/min or renal replacement therapy, inability to tolerate beta-blockers or known contrast allergy.
- There were three co-primary endpoints
- Procedural duration
- Patient satisfaction scores post angiography
- Incidence of contrast-induced nephropathy (KDIGO criteria)
- Secondary endpoints included procedural characteristics, procedural complications, MACE (all-cause mortality, MI, unplanned revascularisation) at 12 months
What is the main result?
Overall, 688 patients were included in the trial, 344 randomised to CTCA & ICA and 344 to ICA alone. In the CTCA group 329 underwent CTCA prior to ICA and 321 underwent ICA. In the ICA group 342 underwent ICA.
- The CTCA & ICA group had a significantly lower procedural duration compared to the ICA alone group. 17.4±10.2 vs. 39.5±16.9 mins (adjusted difference -20.93 98.3%CI -23.5 to -18.35, p<0.001).
- When the combined procedure time of CTCA & ICA was compared to ICA this difference persisted (21.2±20.54 vs. 39.5±16.89, OR -17.38, 95%CI -19.49 to -15.27, p<0.001).
- Patient satisfaction was higher in the CTCA & ICA group 1.49 vs 2.54, 40% relative improvement.
- Contrast-induced nephropathy was significantly lower in the CTCA & ICA group 3.2% vs. 27.9%, 92% relative risk reduction.
- Of the secondary endpoints, procedural complications were higher in the ICA alone group 10.8% vs. 2.4%.
- MACE rates were lower in the CTCA & ICA group 16.28% vs. 29.36%, (OR 0.46, 95%CI 0.32-0.66, p<0.001).
Critical reading and the relevance for clinical practice
The results of this study show that in patients with prior CABG with a clinical indication for invasive angiogram adjuvant CTCA reduces procedural time, improves patient satisfaction and reduces contrast-induced nephropathy (CIN).
Of note, it is not clear in what percentage but the presenter suggested in patients who had undergone a prior CTCA not all grafts were selectively engaged at angiography due to known patency or occlusion which likely influenced the shorter procedural times and increased use of radial access in the CTCA & ICA group. Furthermore, in patients who required PCI at the time of their angiography PCI procedural time was shorter in those who had undergone prior angiography 70.4±34.67 vs. 81.21±36.35 (OR -10.81 95%CI -19.16 to -2.45, p=0.011) suggesting that CTCA may have aided in PCI planning pre-procedure.
The difference in CIN between groups was striking despite the baseline renal function of both groups being well balanced. Further details, particularly with regard to the timing of CTCA and ICA as well as the contrast load used for PCI procedures will be of interest to further understand this difference.
Whilst the study was not powered for MACE there was a significant difference between the groups (CTCA & ICA 16.28% vs. ICA 29.36% OR 0.46, 95%CI 0.32-0.66, p<0.001) which appears to be mainly driven by non-fatal MI 9.59% vs. 18.6%, OR 0.45 95%CI 0.45, 95%CI 0.28-0.71, p<0.001). The definition and timing of the non-fatal MI will be of interest to further interpret this result as well as understanding in the case of peri-procedural MI if the vessel intervened upon was a native coronary artery or a bypass graft.
Overall, this trial suggests that CTCA prior to coronary angiography is beneficial in terms of reducing procedural time and contrast use as well as improving patient satisfaction. Further data with regard to overall radiation exposure, duration of hospitalisation and cost effectiveness will aid in understanding the generalisability of this trial.
References
- Jones D, Castle E, Beirne AM, Rathod K, Treibel T, Guttmann O, et al. Computed tomography cardiac angiography for planning invasive angiographic procedures in patients with previous coronary artery bypass grafting [Internet]. EuroIntervention. [cited 2022 Sep 19].





No comments yet!