NOTION-3 - Percutaneous coronary intervention in patients undergoing transcatheter aortic valve implantation
Reported from ESC Congress 2024
Make the most of the insights from Jacob Thomsen Loenborg’s interview with Chiara De Biase and Ali Nazmi Calik’s article to capture the key takeaways from this trial, simultaneously published in the NEJM, presented at the ESC Congress 2024 in London.
Key take-away messages: PCI with TAVI reduced death, MI, or urgent revascularization compared to TAVI alone but increased minor bleeding.
PCI should be standard in TAVI, with decisions tailored to individual patient risk.
Read the review by Ali Nazmi Calik!
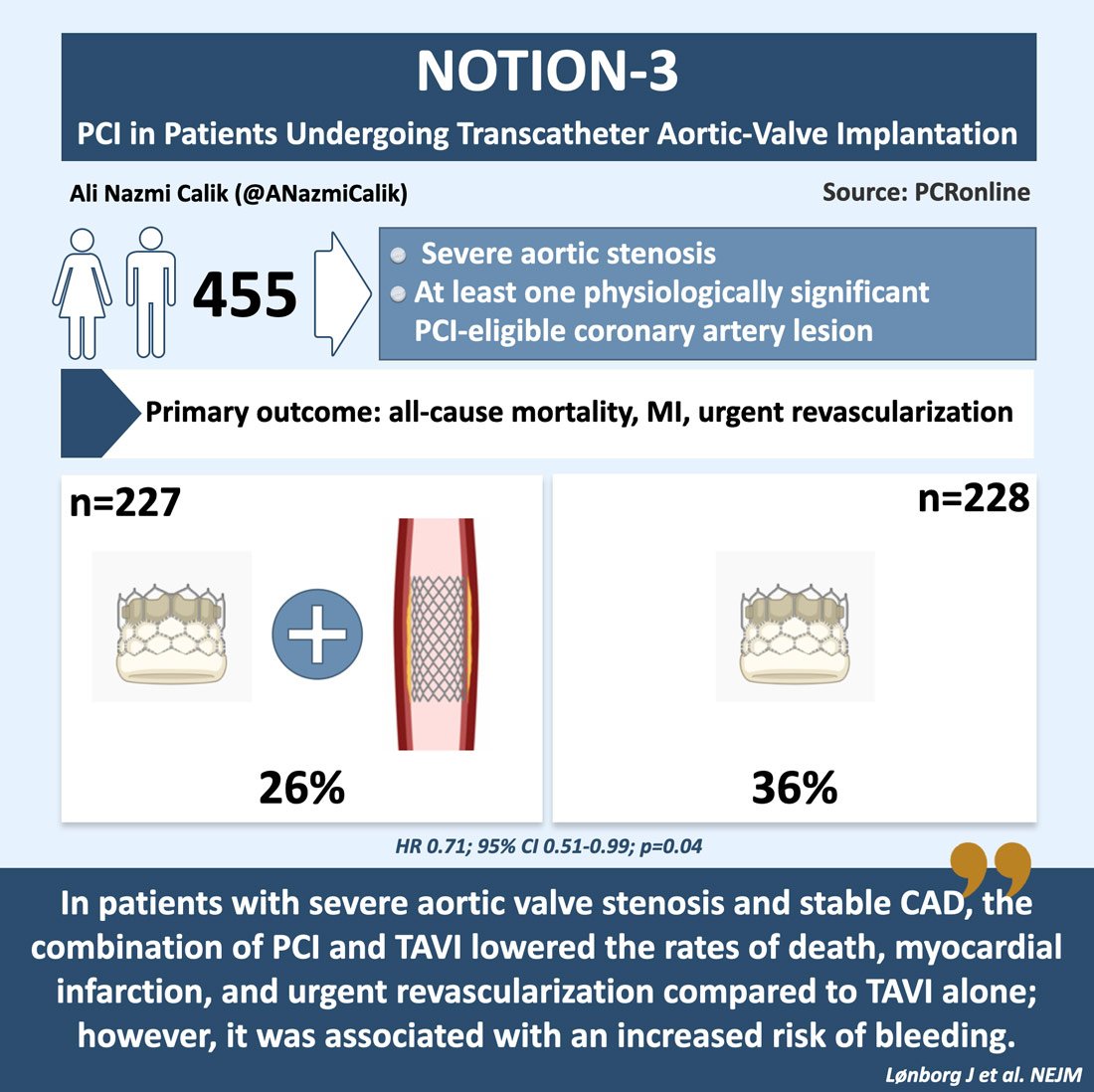
NOTION-3 is a multicenter, international, open-label, randomized superiority trial involving patients with coronary artery disease and severe aortic stenosis undergoing transcatheter aortic valve implantation (TAVI). The trial aims to compare clinical outcomes in patients who underwent revascularization with percutaneous coronary intervention (PCI) to those who were treated conservatively.
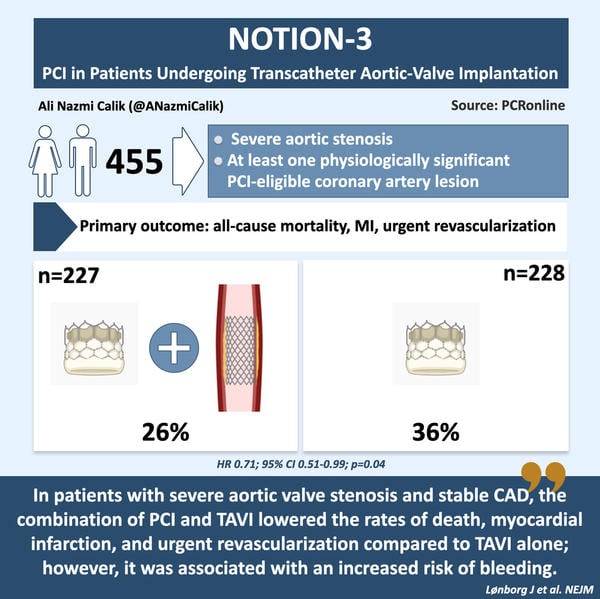
Infographic highlighting key insights from the NOTION-3 trial, designed by Ali Nazmi Calik for PCRonline
Why this study – the rationale/objective?
Coronary artery disease is present in approximately half of the patients undergoing transcatheter aortic valve implantation (TAVI), making the assessment and management of this condition a reasonable strategy. Furthermore, up to 20 % of these patients also undergo treatment with percutaneous coronary intervention (PCI)1-7. Whereas severe aortic stenosis is linked to higher morbidity and mortality, coronary artery disease that is incidentally discovered during the evaluation for TAVI may be a benign finding. In such cases, the potential benefits of PCI may not justify the associated risks6-8.
Given the absence of clear recommendations in U.S. and European guidelines regarding the performance of PCI alongside TAVI, and the lack of relevant data, the NOTION-3 trial was designed to investigate the hypothesis that routine revascularization of coronary artery stenoses — defined as having a fractional flow reserve (FFR) of 0.80 or lower or a coronary artery diameter stenosis of at least 90 %, as determined by angiography — would enhance clinical outcomes in patients with stable coronary artery disease and severe symptomatic aortic stenosis when performed in conjunction with TAVI. This would be compared to TAVI alone without revascularization.
How was it executed - the methodology
Patients were eligible for randomization if they had severe aortic stenosis and were selected for TAVI by the local heart team. Additionally, they needed to have at least one physiologically significant stenosis in a coronary artery with a diameter of at least 2.5 mm. Physiological significance was defined as having a fractional flow reserve (FFR) of 0.80 or lower, or a coronary artery diameter stenosis of at least 90 %, as determined by visual assessment.
The primary exclusion criteria included a life expectancy of less than one year, severe renal failure (defined as an estimated glomerular filtration rate of less than 20 ml per minute per 1.73 m² of body surface area), an acute coronary syndrome occurring within 14 days prior to the heart team's decision to proceed with TAVI, and left main coronary artery stenosis.
Patients assigned to the PCI group were intended to receive complete revascularization of all PCI-eligible lesions in coronary arteries with a diameter of at least 2.5 mm that met either the FFR or angiographic criteria. The protocol strongly advised that PCI be completed prior to TAVI as part of a staged approach; however, PCI performed concurrently with TAVI or within two days following the procedure was also permitted.
Patients in the PCI group received lifelong aspirin at a daily dose of 75 mg and clopidogrel at the same dose for 6 months following the PCI. For those requiring oral anticoagulation, aspirin was continued for 1 month and clopidogrel for 6 months, while oral anticoagulation was maintained indefinitely. However, following the publication of the AUGUSTUS trial in 2019, the duration of aspirin therapy for these patients was shortened to 7 days9. Patients in the conservative-treatment group were prescribed lifelong aspirin at a daily dose of 75 mg and clopidogrel at the same dose for 3 months, following standard practice after TAVI. However, after the publication of the POPular TAVI trial in 2020, these patients received lifelong aspirin monotherapy at 75 mg daily, without clopidogrel10.
The primary endpoint was a major adverse cardiac event, defined as a composite of death from any cause, myocardial infarction, or urgent revascularization, assessed until more than one year after TAVI for the last enrolled patient. Urgent revascularization included any procedure performed during an unplanned hospital admission for acute coronary syndrome.
Secondary end points included the individual components of the primary end point; death from cardiovascular causes; periprocedural or spontaneous myocardial infarction; any revascularization; stent thrombosis; hospital admission for heart failure; stroke; bleeding, assessed according to the Valve Academic Research Consortium–2 definitions; acute kidney failure; New York Heart Association functional class (I, II, III, or IV) after TAVI; and the Canadian Cardiovascular Society (CCS) class indicating the severity of angina after TAVI.
What is the main result?
Between September 2017 and October 2022, a total of 455 patients were enrolled across 12 hospitals and included in the primary analysis. Of these, 227 patients were assigned to the PCI group, while 228 were assigned to the conservative treatment group.
The median age of the patients was 82 years, and 67 % of the patients were men. The median STS-PROM score was 3 % and the median SYNTAX score was 9. Patients in the PCI group had a higher number of lesions characterized by an FFR of 0.80 or lower, or a coronary artery diameter stenosis of at least 90 %, compared to those in the conservative treatment group.
Complete revascularization was achieved in 89 % of patients in the PCI group. PCI was performed before TAVI in 74 % of the patients, while 26 % underwent PCI either simultaneously (17 %) with or shortly after (9 %) TAVI. None of the patients in the conservative treatment group had a planned PCI prior to TAVI.
At a median follow-up of 2 years, the primary endpoint (defined as a composite of death from any cause, myocardial infarction, or urgent revascularization) occurred in 60 patients (26 %) in the PCI group, compared to 81 patients (36 %) in the conservative treatment group (HR,0.71; 95 % CI, 0.51 to 0.99, p = 0.04). The difference was primarily driven by higher rates of myocardial infarction and the need for urgent revascularization in the conservative treatment group. Any minor, major, life-threatening, or disabling bleeding occurred in 64 patients (28 %) in the PCI group, compared to 45 patients (20 %) in the conservative treatment group (HR, 1.51; 95 % CI, 1.03 to 2.22).
Critical reading and the relevance for clinical practice
In patients with stable coronary artery disease and severe symptomatic aortic stenosis, characterized by an FFR of 0.80 or lower or a coronary artery diameter stenosis of at least 90 % as determined by angiography, undergoing TAVI, revascularization with PCI was linked to a reduced risk of a composite outcome of death from any cause, myocardial infarction, or urgent revascularization compared to conservative treatment. However, the PCI group experienced a higher risk of bleeding than the conservative treatment group.
The NOTION-3 trial differs in several key aspects from the ACTIVATION trial11, which was halted early due to futility and failed to achieve non-inferiority at one year. NOTION-3 included nearly twice as many patients and had a longer follow-up period compared to ACTIVATION. Additionally, NOTION-3 did not specify the Canadian Cardiovascular Society (CCS) class as an inclusion or exclusion criterion. In ACTIVATION trial, coronary artery disease was defined anatomically as a diameter stenosis of at least 70 %, which is considered less reliable than physiological testing in patients without aortic stenosis. In patients with severe aortic stenosis, FFR may underestimate the physiological significance of coronary artery stenosis. However, this underestimation may have limited clinical impact, as about 10 % of patients with untreated coronary artery disease show FFR values crossing the 0.80 cutoff when comparing pre-TAVI and 6-month post-TAVI measurements.
Nonetheless, it remains to be determined whether coronary artery disease assessment in patients undergoing TAVI should rely on physiological measures like FFR or on visual evaluations of the coronary arteries.
In the NOTION-3 trial, patients assigned to PCI showed a reduced incidence of myocardial infarction, urgent revascularization, and any form of revascularization compared to those assigned to conservative treatment and benefits of PCI were most pronounced in lesions with a diameter stenosis of at least 90 %, aligning with prior observations12,13. Increased patient activity following TAVI and changes in coronary wall shear stress after the procedure may serve as plausible explanations for these findings.
When interpreting the results of this trial, it is important to consider the median number of physiologically significant lesions per patient (n = 1), the low SYNTAX score, and the small proportion of patients with multivessel disease. Additionally, changes in the antiplatelet therapy regimen during the trial should be taken into account. Finally, the current trial does not address the timing of PCI, as 74 % of patients underwent the procedure prior to TAVI, while 26 % had it performed during or after the procedure.
In conclusion, the results of the NOTION-3 trial suggest that PCI should be considered for lesions with an FFR of 0.80 or lower or an angiographic coronary artery diameter stenosis of at least 90 % in all patients with severe aortic stenosis undergoing TAVI. However, the decision to proceed with PCI should be individualized, taking into account the patient's age, overall health, comorbidities, life expectancy, the complexity and severity of coronary artery disease, and the associated bleeding risk.
References
- Faroux L, Guimaraes L, Wintzer-Wehe- kind J, et al. Coronary artery disease and transcatheter aortic valve replacement: JACC state-of-the-art review. J Am Coll Cardiol 2019;74:362-72.
- Sabbah M, Engstrøm T, De Backer O, Søndergaard L, Lønborg J. Coronary assessment and revascularization before transcutaneous aortic valve implantation: an update on current knowledge. Front Cardiovasc Med 2021;8:654892.
- Massussi M, Adamo M, Rosati F, Chizzola G, Metra M, Tarantini G. Coronary artery disease and TAVI: current evidence on a recurrent issue. Catheter Cardiovasc Interv 2023;101:1154-60.
- Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J 2022;43:561-632.
- Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/ American Heart Association Joint Com- mittee on Clinical Practice Guidelines. J Am Coll Cardiol 2021;77:450-500.
- Snow TM, Ludman P, Banya W, et al. Management of concomitant coronary artery disease in patients undergoing trans- catheter aortic valve implantation: the United Kingdom TAVI Registry. Int J Cardiol 2015;199:253-60.
- Søndergaard L, Popma JJ, Reardon MJ, et al. Comparison of a complete percutaneous versus surgical approach to aortic valve replacement and revascularization in patients at intermediate surgical risk: results from the randomized SURTAVI trial. Circulation 2019;140:1296-305
- Généreux P, Sharma RP, Cubeddu RJ, et al. The mortality burden of untreated aortic stenosis. J Am Coll Cardiol 2023;82: 2101-9.
- Lopes RD, Heizer G, Aronson R, et al. Antithrombotic therapy after acute coronary syndrome or PCI in atrial fibrillation. N Engl J Med 2019;380:1509-24.
- Brouwer J, Nijenhuis VJ, Delewi R, et al. Aspirin with or without clopidogrel after transcatheter aortic-valve implantation. N Engl J Med 2020;383:1447-57.
- Patterson T, Clayton T, Dodd M, et al. ACTIVATION (PercutAneous Coronary inTervention prIor to transcatheter aortic VAlve implantaTION): a randomized clinical trial. JACC Cardiovasc Interv 2021;14: 1965-74.
- Johnson NP, Tóth GG, Lai D, et al. Prognostic value of fractional flow reserve: linking physiologic severity to clinical outcomes. J Am Coll Cardiol 2014;64: 1641-54.
- Persits I, Layoun H, Kondoleon NP, et al. Impact of untreated chronic obstructive coronary artery disease on outcomes after transcatheter aortic valve replacement. Eur Heart J 2024;45:1890-900.
Related publications
- Management of coronary artery disease in patients undergoing transcatheter aortic valve implantation. A clinical consensus statement from the European Association of Percutaneous Cardiovascular Interventions in collaboration with the ESC Working Group on Cardiovascular Surgery
- Comparison of different percutaneous revascularisation timing strategies in patients undergoing transcatheter aortic valve implantation
- A randomised multicentre study of angiography- versus physiology-guided percutaneous coronary intervention in patients with coronary artery disease undergoing TAVI: design and rationale of the FAITAVI trial
Latest news from ESC Congress 2024
Authors






No comments yet!