OCCUPI - Optical coherence tomography-guided coronary intervention in patients with complex lesions
Reported from ESC Congress 2024
Alex Sticchi provides his take on the OCCUPI trial presented by Kim Byeong-Keuk at the ESC Congress 2024 in London.
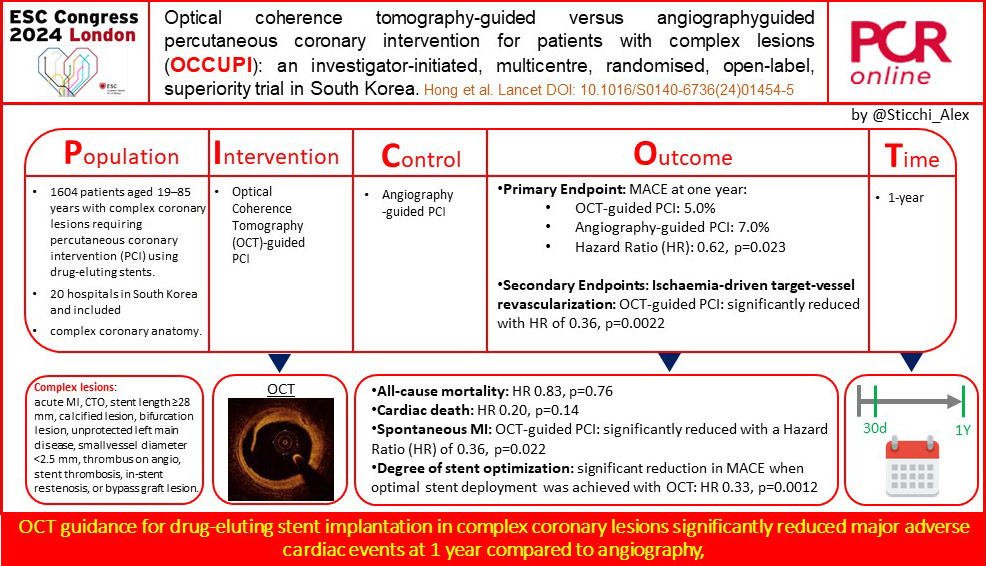
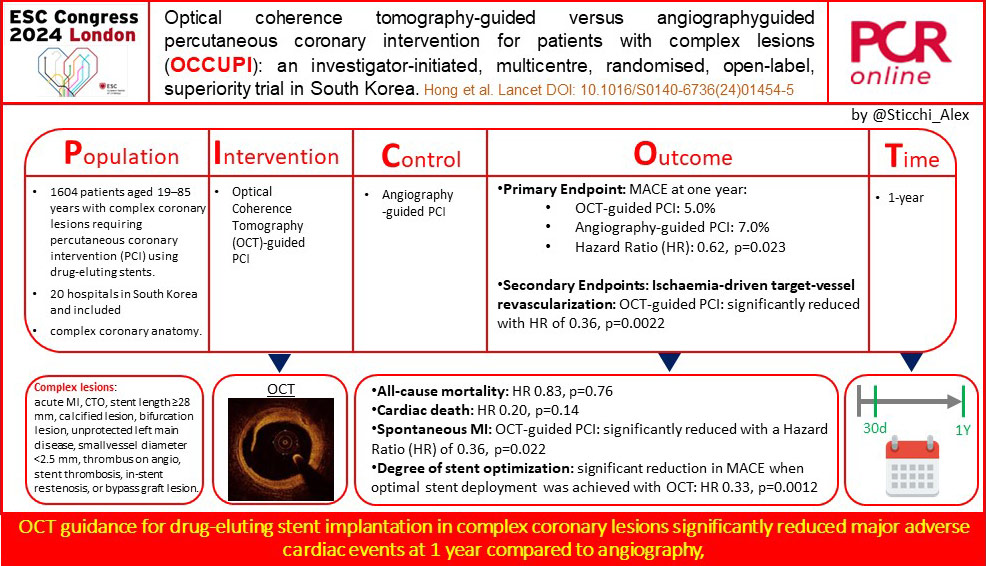
Graphic summary of key aspects of the OCCUPI trial. Courtesy of Alex Sticchi. Source: PCRonline.com
Why this study – The rationale/objectives
Complex percutaneous coronary interventions (PCI) present significant challenges due to the intricate nature of the lesions involved, which are often associated with higher risks of stent-related ischemic events. Although the last generations of drug-eluting stents have improved outcomes, the complexity of these lesions still necessitates enhanced procedural strategies. Optical coherence tomography (OCT) offers a more detailed intravascular imaging modality compared to traditional angiography, potentially allowing for better stent placement and optimization. However, despite its technological promise, the clinical superiority of OCT-guided PCI over angiography-guided PCI, particularly in complex cases, had not been definitively proven. The OCCUPI trial was designed to address this gap, aiming to determine whether OCT guidance could significantly reduce major adverse cardiac events (MACE) compared to angiography-guided PCI in patients with complex coronary lesions at 1 year.
How was it executed – The methodology
The OCCUPI trial was an investigator-initiated, multicenter, randomized, open-label, superiority trial conducted across 20 hospitals in South Korea.
It included 1604 patients aged 19–85 years who required PCI with drug-eluting stents for complex coronary lesions. Patients were randomly assigned in a 1:1 ratio to either OCT-guided PCI (803 patients) or angiography-guided PCI (801 patients).
The study’s primary endpoint was the occurrence of MACE—comprising cardiac death, myocardial infarction, stent thrombosis, or ischaemia-driven target-vessel revascularization—within one year post-PCI. Secondary endpoints included individual components of the primary endpoint, overall revascularization rates, periprocedural myocardial infarction, and the degree of stent optimization achieved through OCT.
What is the main result?
The primary endpoint occurred in 5% of the OCT-guided group compared to 7% in the angiography-guided group, indicating a statistically significant reduction in MACE with OCT guidance (HR 0.62, p=0.023). This reduction was largely driven by significant decreases in ischaemia-driven target-vessel revascularization (HR 0.36, p=0.0022) and spontaneous myocardial infarction (HR 0.36, p=0.022) in the OCT group. However, no significant differences were observed in all-cause death (HR 0.83, p=0.76) or cardiac death (HR 0.20, p=0.14) between the groups. Notably, PCI optimization based on OCT findings was associated with a substantial reduction in MACE compared to patients who did not achieve optimal results (HR 0.33, p=0.0012). Despite these positive outcomes, 30% of patients in the OCT group did not meet optimal imaging criteria, reflecting challenges in achieving procedural perfection even with advanced imaging tools.
Critical reading and the relevance for clinical practice
The OCCUPI trial stands as a cornerstone study in the ongoing evaluation of intravascular imaging’s role in percutaneous coronary interventions (PCI), particularly in complex coronary lesions. The trial’s findings emphasize the importance of OCT in improving procedural outcomes by reducing major adverse cardiac events (MACE) compared to conventional angiography-guided PCI. However, the study also highlights certain limitations and areas where further research and refinement are needed to fully realize the potential benefits of OCT.
Comparative effectiveness and safety
The OCCUPI trial’s results demonstrate that OCT-guided PCI significantly reduces MACE at one year compared to angiography-guided PCI, particularly through a reduction in ischaemia-driven target-vessel revascularization and spontaneous myocardial infarction. These findings are consistent with the growing body of evidence that supports the use of intravascular imaging to optimize stent deployment and procedural outcomes resulting the best class of recommendation in the ESC 2024 guidelines for Chronic Coronary Syndromes.
However, it is important to note that the trial did not find significant differences in all-cause mortality or cardiac death between the two groups. This suggests that while OCT improves immediate and mid-term procedural outcomes, its impact on long-term survival remains uncertain.
Additionally, the trial revealed that 30% of patients in the OCT-guided group did not achieve optimal procedural results, despite the advanced imaging provided by OCT. This highlights a critical challenge in the clinical application of OCT: achieving consistent procedural optimization across diverse patient populations and lesion complexities. The variability in achieving optimal outcomes with OCT underscores the need for operator expertise, standardized protocols, and potentially adjunctive technologies to ensure that the full benefits of OCT are realized in clinical practice.
Integration of OCT into clinical practice
The OCCUPI trial’s findings advocate for the broader adoption of OCT in PCI, particularly in cases involving complex coronary lesions. The significant reduction in MACE observed with OCT guidance suggests that OCT should be considered a valuable tool for improving procedural success and patient outcomes. However, the lack of significant mortality benefits also calls for a nuanced approach to its use, balancing the advantages of enhanced imaging with the associated costs, increased contrast use, and procedural time.
Due to these considerations, we should emphasize the need for personalized approaches in using OCT, suggesting that its greatest benefits may be seen in specific patient subgroups, such as those with high-risk anatomical features or complex lesion morphologies.
Moreover, we have to continue with a growing education about OCT use because the learning curve associated with this intracoronary imaging tool indicates that operator experience plays a significant role in the effectiveness of OCT-guided PCI. This highlights the importance of targeted training programs and the potential development of automated OCT analysis tools to assist operators in achieving optimal outcomes.
Future directions and final considerations
Looking forward, the OCCUPI trial suggests several avenues for future research and clinical development. One key area is the exploration of adjunctive technologies that could complement OCT, such as artificial intelligence (AI) algorithms designed to assist in real-time image analysis and decision-making. These technologies could help bridge the gap between OCT’s potential and the variability in achieving optimal outcomes observed in the trial.
Another important consideration is the need for longer-term follow-up studies to assess the durability of OCT-guided PCI benefits. While the OCCUPI trial provides compelling evidence of short- to mid-term improvements, the impact of OCT on long-term clinical outcomes, including mortality and the need for repeat interventions, remains an open question.
Finally, the trial underscores the importance of integrating OCT into broader clinical guidelines for PCI, particularly in complex cases where traditional angiography may fall short. As OCT technology continues to evolve, it will be crucial to refine its use within clinical practice, ensuring that its application is both effective and efficient.
The OCCUPI trial confirms that OCT-guided PCI is a safe and effective approach that significantly reduces MACE compared to angiography-guided PCI, particularly through a reduction in target-vessel revascularization and myocardial infarction. However, the trial also highlights the challenges associated with achieving consistent procedural optimization and the need for further research to fully understand the long-term benefits of OCT. As OCT becomes more integrated into clinical practice, its role in improving outcomes for patients with complex coronary lesions will likely continue to grow, supported by ongoing advancements in technology and operator training.
Related publications
- Five-year follow-up of OCT-guided percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction
- Impact of morphofunctional assessment with quantitative flow ratio and optical coherence tomography in patients with acute coronary syndromes
- Intracoronary optical coherence tomography: state of the art and future directions




No comments yet!