Intravascular lithotripsy for treatment of calcified coronary lesions: patient-level pooled analysis of the Disrupt CAD studies
Selected in JACC: Cardiovascular Interventions by M. Pighi , N. Ryan
Using patient-level data from the Disrupt CAD I, II, III and IV trials, this pooled analysis assesses the efficacy and safety of intravascular lithotripsy in de novo calcified coronary lesions.
References
Authors
Dean J. Kereiakes, Carlo Di Mario, Robert F. Riley, Jean Fajadet, Richard A. Shlofmitz, Shigeru Saito, Ziad A. Ali, Andrew J. Klein, Matthew J. Price, Jonathan M. Hill, and Gregg W. Stone
Reference
10.1016/j.jcin.2021.04.015
Published
May 2021
Link
Read the abstractReviewers
Our Comment
Why this study? – the rationale/objective
Using patient-level data from the Disrupt CAD I, II, III and IV trials, this pooled analysis assesses the efficacy and safety of coronary intravascular lithotripsy (IVL) in de novo calcified coronary lesions.
Calcified coronary lesions are a challenging subset for PCI, often characterized by inadequate plaque modification, leading to an increased risk of stent under-expansion, a key predictor of restenosis, thrombosis, and repeat revascularization. In addition, adequate plaque preparation can be difficult with high-pressure non-compliant balloons and cutting balloons associated with increased risk of vessel dissection, perforation, and periprocedural MI.
Traditionally, atherectomy has been the technique of choice in heavily calcified lesions; however, adequate plaque preparation can be challenging due to wire bias, and there is an associated risk of slow flow or no flow due to distal embolization. IVL utilizes acoustic pressure waves to fracture calcium and allow adequate expansion of stents.
This study combines the patient-level data from the single-arm prospective multicentre, Disrupt CAD studies to assess the cumulative efficacy and safety of IVL in de novo calcified coronary lesions.
How was it executed? – the methodology
All patients enrolled in Disrupt CAD I, II, III and IV from December 2015 to April 2020 were included in this analysis. Inclusion criteria included operator assessed severe calcification: the presence of fluoroscopic radiopacities noted without cardiac motion before contrast injection involving both sides of the arterial wall in at least 1 location, and total length of calcium of at least 15 mm and extending partially into the target lesion, or an intravascular imaging-demonstrated calcium angle of ≥ 270° in at least 1 cross-section. All angiograms underwent corelab analysis.
- The primary efficacy endpoint was procedural success, defined as stent delivery with residual in-stent stenosis ≤ 30 %, assessed by the angiographic core lab, without in-hospital MACE.
- The primary safety endpoint was 30-day MACE, a composite of cardiac death, MI or TVR
- Procedural success with a residual stenosis threshold of < 50 %, final post-procedural percent diameter stenosis, post-IVL and final serious angiographic complications (defined as ≥ Grade D dissection, perforation, abrupt closure, slow flow/no-reflow), as well as target lesion failure (TLF) and definite or probable stent thrombosis at 30 days, were secondary endpoints.
What is the main result?
Overall, 628 patients from 72 sites in 12 countries were included in the analysis. All lesions were de novo calcified lesions in patients presenting stable or unstable angina or silent ischemia.
The majority of patients were male (77.1 %), with a mean age of 71.8 ± 8.9 years. A quarter had renal impairment (25.1 %), and over a third had diabetes (38.4 %). Thirty-day follow-up was available for 626 patients (99.7 %). Corelab analysis confirmed severe calcification in 97 % of target lesions, with a lesion length of 24.4 ± 11.5mm and a calcified segment length of 41.5 ± 20mm. IVL was successfully delivered in 98.7 % of procedures, with 74.7 ± 42.7 pulses administered.
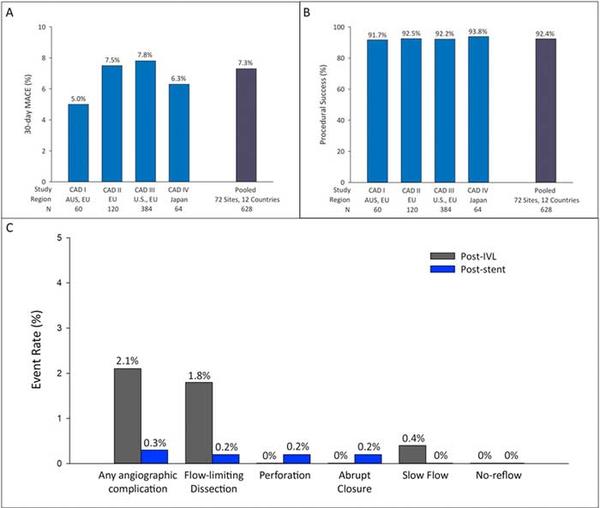
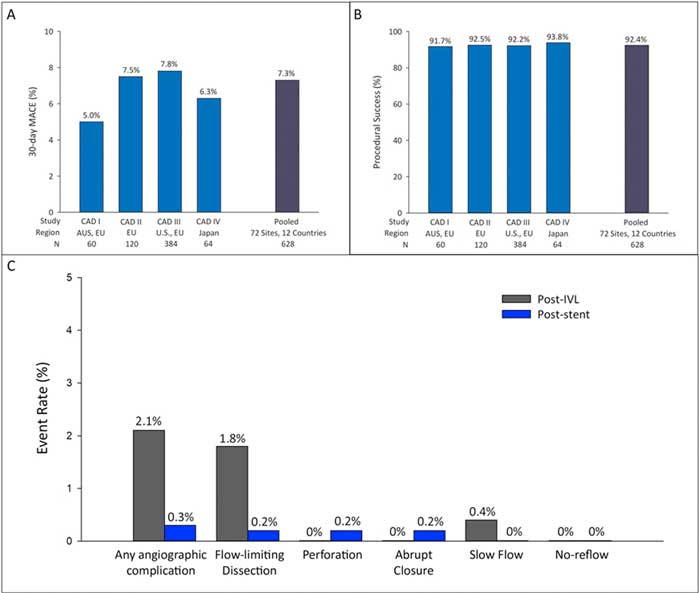
- The primary efficacy endpoint was achieved in 92.4 % of patients (95 % CI 90.0 - 94.3 %) with no significant differences across the four studies.
- The 30-day MACE rate was 7.3 % (95 % CI 5.4 - 9.7 %), mainly driven by non Q wave MI (6.9 % 95% CI 5.0 - 9.1 %). TLF at 30 days was 7.2 % (95 % CI 5.3 - 9.5 %) with low rates of probable stent thrombosis (0.8 % 95 % CI 0.3 - 1.9 %)
- Overall serious complications were low at 2.1 % post IVL (flow-limiting dissection 1.8 %, slow flow 0.4 %) and 0.3 % at end of procedure.
- At subgroup analysis both lesions > 25 mm and bifurcation lesions had lower procedural success rates (90.7 % vs. 94.9 % p = 0.05 and 89.5 % vs. 94.8 % p = 0.02) and lower rates of freedom from MACE at 30 days (90.0 % vs. 94.6 % p = 0.03 and 88.9 % vs. 94.3 % p = 0.03).
Source = JACC: Cardiovascular Interventions
Critical reading and the relevance for clinical practice:
The results of this patient-level pooled analysis show that IVL is both safe and efficacious in de-novo calcified coronary lesions. Corelab analysis confirmed that 97 % of included lesions were truly severely calcified, those most expected to provide challenges for adequate plaque preparation. At subgroup analysis, anatomical complexity, lesions > 25mm and bifurcation lesions were predictors of poorer outcomes however, overall both MACE and serious complication rates were low.
A note of caution when interpreting the results, one must bear in mind that there are some limitations to the data, i.e. these were single-arm prospective trials with no comparator. Further data supporting the use of IVL in more complex patient and anatomic subgroups, e.g. LMS disease, in-stent restenosis, and its use in combination with other plaque modifying techniques such as “rota shock” are required. Acute coronary syndromes and very long lesions (> 40mm) were also excluded from this study, in such settings, IVL may have required adjuvant therapy to achieve adequate stent delivery and optimization. This paper does not provide data on intravascular imaging following IVL and stenting. The authors report that this analysis is ongoing and will be the focus of a future manuscript. Intravascular imaging is an extremely useful tool in confirming circumferential and longitudinal multi-plane calcium fracture. Adequate calcium fracture is key in allowing optimal stent implantations and impacts clinical outcomes, particularly in complex settings (i.e. long lesions, bifurcations, and chronic total occlusions).
Given the good outcomes from the initial Disrupt CAD studies, IVL is now used in real-world clinical practice. Further data, including that from the post-marketing registry, will provide insights into the long-term durability of the IVL as an adjunct to PCI and the generalisability of the findings from the Disrupt trials. Ongoing clinical experience, as well as study data, will determine the role of IVL in the plaque modification algorithm.








No comments yet!