Multivessel PCI Guided by FFR or Angiography for Myocardial Infarction - FLOWER-MI
Selected in New England Journal of Medicine by N. Ryan , M. Pighi
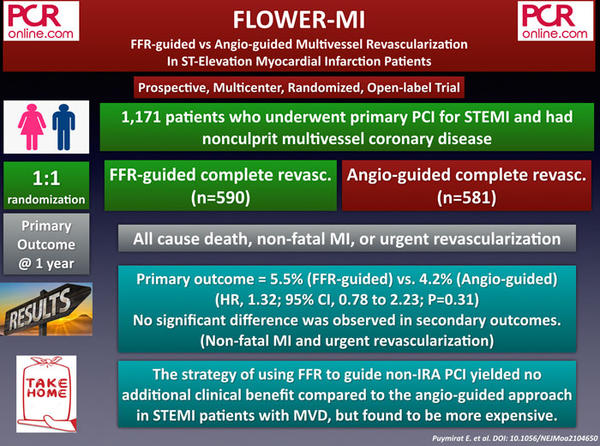
This investigator-initiated randomised, open-label, multicentre trial compares FFR versus angiography guided strategies for treating non-culprit lesions in patients presenting with STEMI and multivessel coronary artery disease. The results of this study were released during ACC.21.
References
Authors
Etienne Puymirat, M.D., Ph.D., Guillaume Cayla, M.D., Ph.D., Tabassome Simon, M.D., Ph.D., Philippe G. Steg, M.D., Gilles Montalescot, M.D., Ph.D., Isabelle Durand-Zaleski, M.D., Ph.D., Alicia le Bras, M.D., Romain Gallet, M.D., Ph.D., Khalife Khalife, M.D., Jean-François Morelle, M.D., Pascal Motreff, M.D., Ph.D., Gilles Lemesle, M.D., Ph.D., Jean-Guillaume Dillinger, M.D., Ph.D., Thibault Lhermusier, M.D., Ph.D., Johanne Silvain, M.D., Ph.D., Vincent Roule, M.D., Ph.D., Jean-Noel Labèque, M.D., Grégoire Rangé, M.D., Grégory Ducrocq, M.D., Ph.D., Yves Cottin, M.D., Didier Blanchard, M.D., Anaïs Charles Nelson, N.D., Bernard De Bruyne, M.D., Ph.D., Gilles Chatellier, M.D., and Nicolas Danchin, M.D. et al
Reference
May 16, 2021 DOI: 10.1056/NEJMoa2104650
Published
16 May 2021
Link
Read the abstractReviewers
Our Comment
Why this study- the rationale/objective?
In stable patients, FFR guided revascularisation is superior to angiography alone, the data for patients presenting with STEMI is less clear. In patients with STEMI complete revascularisation, either angiography- or FFR-guided, is superior to culprit-only revascularisation in reducing repeated revascularisation; however, whether an FFR-guided strategy improves clinical outcomes over angiography alone is unknown.
How was it executed – the methodology?
From December 2016 to December 2018, 1171 patients presenting with a STEMI having undergone successful culprit vessel PCI were randomised to FFR guided versus angiography guided non-culprit revascularisation. Multivessel disease was defined as >50% stenosis in at least one non-culprit artery >2.0mm in diameter amenable to PCI. Complete revascularisation during the index procedure was encouraged, and if this was not possible, it was achieved as soon as possible and within five days of the initial procedure.
- The primary outcome was a composite of all-cause death, non-fatal MI and unplanned hospitalisation leading to urgent revascularisation at one year.
- The secondary outcomes included procedural time, contrast volume, the individual components of the primary outcome, any revascularisation, urgent revascularisation of any target lesion in a non-culprit artery, rehospitalisation for angina/heart failure, rehospitalisation within the cardiology department, CCS angina class, quality of life as assessed with EQ-5D, number of anti-anginal medications, cost-effectiveness, cost-utility.
What is the main result?
Overall, 1171 patients from 41 sites in France were enrolled in the trial. After exclusion criteria, 586 patients underwent FFR-guided non-culprit revascularisation and 577 angiography-guided non-culprit revascularisation and were included in the ITT analysis. The majority of participants were men (83%) in their 60’s with no significant differences in cardiovascular risk factors between groups. Approximately 60% presented with an infarction in the inferior leads on ECG. A quarter of patients had three-vessel CAD, with the majority presenting with two-vessel disease (culprit and one other artery).
- The primary outcome occurred in 5.5% (32/586) of patients in the FFR group compared to 4.2% (24/577) in the angiography group (HR 1.32, 95% CI 0.78-2.23, p=0.31)
- In the FFR group, the mean FFR was 0.79±0.11 with 44.3% of lesions having an FFR ≥0.80
- Over half of non-culprit lesions were angiographically severe (>70%) by visual estimation in both arms (FFR 52.9% vs Angio 67.2%)
- PCI was carried out in 55.7% of lesions in the FFR group compared to 90.5% in the angiography group.
Critical reading and the relevance for clinical practice
The results of this investigator-initiated randomised, open-label, multicentre trial showed that an FFR-guided strategy for non-culprit lesions in patients presenting with STEMI and multivessel coronary artery disease did not provide a significant benefit above an angiography-guided strategy. Of note, all patients included in the trial were treated with optimal medical therapy.
Several studies have shown that physiologically guided deferral of PCI in the setting of ACS leads to higher rates of MACE than in stable patients. This phenomenon may be due to the microvascular dysfunction and adenosine resistance post STEMI leading to higher FFR values (i.e. negative), than those that may be obtained once the microvascular bed has recovered. In this trial the non-culprit evaluation was carried out at a mean time of 2.6 days post STEMI, implying some negative FFRs may have been positive if assessed at a later timepoint.
Once again this study raises the question of plaque vulnerability and inflammation in the context of STEMI. Patients presenting with STEMI may have vulnerable plaque through their coronary tree, potentially explaining the improved outcomes with complete versus culprit-only revascularisation. In the PROSPECT II trial, non-IRA plaque burden more than 70% and LCBI >324 by IVUS/NIRS were independent predictors of MACE. High-risk plaque characteristics (i.e. TCFA) on OCT in non-culprit lesions were the strongest predictor of MACE despite negative FFR in the COMBINE-FFR study.
A note of caution when interpreting the results, the MACCE rates in both arms were significantly lower (<5%) than those used in the power analysis (9.5% FFR, 15% angiography). Consequently, the trial would have required the enrolment of almost 8000 patients to demonstrate meaningful differences among the two strategies. Furthermore one could argue vessels <2.5mm should not be included given the limitations of current DES.
Given the outcome from this trial, complete revascularisation guided by angiography appears to be a reasonable option based on the operator's preference and healthcare economy. In addition, the recently commenced OCT-CONTACT trial will help determine if patients with STEMI benefit from imaging guided revascularisation of non-culprit lesions.







No comments yet!