3-year outcomes after a 2-stent with provision stenting for complex bifurcation lesions defined by DEFINITION criteria
Selected in JACC: Cardiovascular Interventions by N. Ryan
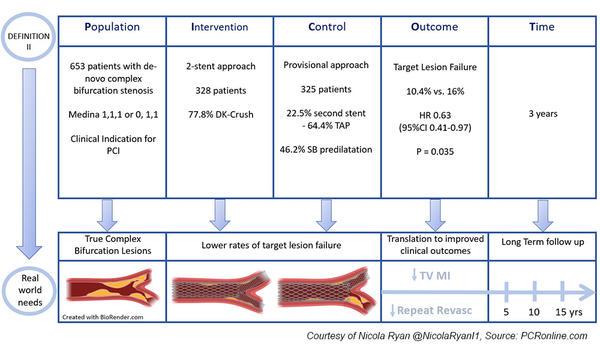
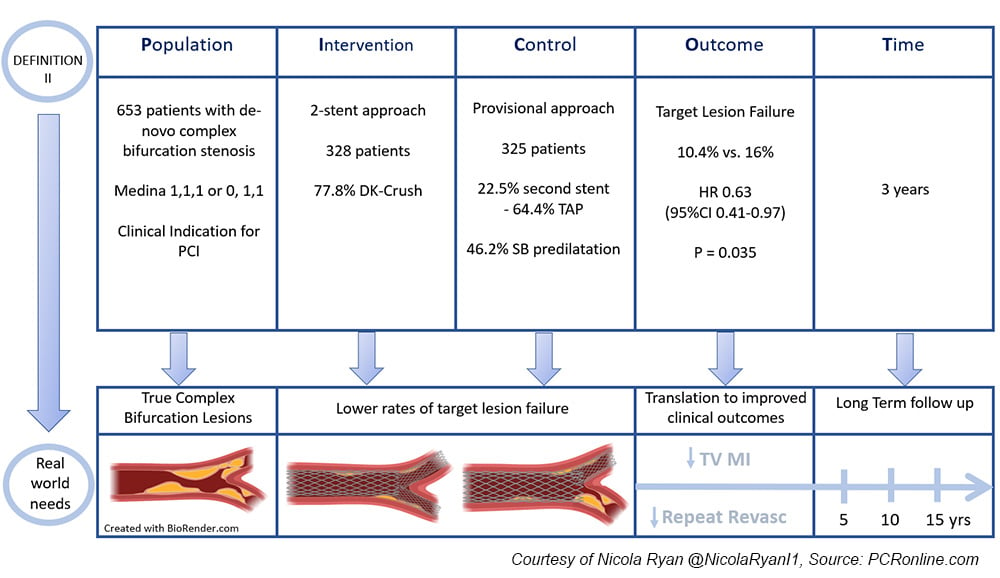
DEFINITION II was a randomised control trial comparing PCI in complex bifurcation lesions using a two-stent technique versus a provisional stenting strategy. At one year follow-up, a two-stent technique was superior to a provisional approach in true complex bifurcations. Here, the authors present the 3-year clinical outcomes of the DEFINITION II trial.
References
Authors
Jing Kan, Jun-Jie Zhang, Imad Sheiban, Teguh Santoso, Muhammad Munawar, Damras Tresukosol, Kai Xu, Gregg W. Stone, Shao-Liang Chen, and on behalf of the DEFINITION II Investigators.
Reference
J Am Coll Cardiol Intv. 2022 Jul, 15 (13) 1310–1320
Published
July 2022
Link
Read the abstract
Reviewer
Latest contributions
Balloon lithotripsy added to conventional preparation before stent implantation in severely calcified coronary lesions Impact of pullback pressure gradient on clinical outcomes after percutaneous coronary interventions Validation of intravascular ultrasound-defined optimal stent expansion criteria for favorable 1-year clinical outcomesMy Comment
Why this study – the rationale/objective?
The optimal PCI strategy in bifurcation lesions is a topic of debate with a provisional strategy (PS) considered the standard approach in the majority of cases. DKCRUSH-V however, showed lower rates of target lesion failure (TLF) at one and three years in true LM bifurcations using a double-kissing crush technique compared to provisional stenting.
The DEFINITION Criteria were developed to identify complex bifurcations; however, prior to the DEFINITION II trial, they had not been assessed in a prospective fashion. At one-year follow up, TLF was significantly higher in the PS group compared to the two-stent group (11.4 % vs. 6.1 %, HR 0.52; 95 % CI 0.30-0.90, p = 0.019), mainly driven by TLR (5.5 % vs. 2.4 %, HR 0.43,95 % CI 0.19-1.0, p = 0.049) and TVMI (7.1 % vs. 3.0 %, HR 0.43, 95 % CI 0.2-0.9, p = 0.025).
How was it executed? - the methodology
DEFINITION II was a randomised control trial in patients undergoing PCI for symptoms or proven ischaemia with a de-novo complex bifurcation stenosis (Medina 1,1,1 or 0,1,1) as defined by the DEFINITION criteria.
The DEFINITION criteria require one major and two minor criteria to assess a bifurcation lesion as complex. (Major: SB lesion length ≥ 10 mm with ≥ 70 % stenosis for LM or ≥ 90 % stenosis for non-LM, Minor: moderate-severe calcification, multiple lesions, bifurcation angle < 45° or > 70°, MVRD < 2.5 mm, thrombus containing lesion, MV lesion length ≥ 25 mm.)
- The primary endpoint was TLF (a composite of cardiac death, target vessel MI, or clinically driven TLR) at 3 years, with a safety endpoint of stent thrombosis.
- DK Crush or Culotte was strongly recommended for the two-stent group, with the second stent strategy left to the operators discretion in the provisional group if required.
- POT was recommended in both groups.
What is the main result?
DEFINITION-II randomised 653 patients, 328 to the two-stent technique and 325 to the PS with 3-year follow-up available for 321 and 322 respectively.
In both the two-stent and PS groups, the majority of bifurcations were LAD/Diagonal followed by distal LMS (62.5 % vs. 60.6 % and 28.7 % vs. 28.9 % p = 0.552, respectively). IVUS was used in slightly over a quarter of cases (27.7 %) with final POT performed in almost all cases (2-stent 98.2 % vs PS 99.0 %).
- TLF was significantly higher in the PS group compared to the two-stent group (16 % vs. 10.4 %, HR 0.63; 95 % CI 0.41-0.97, p = 0.034), mainly driven by TLR (8.3 % vs. 4.3 %, HR 0.50, 95 % CI 0.26-0.96, p = 0.038) and TVMI (8 % vs. 3.7 %, HR 0.45, 95 % CI 0.23-0.89, p = 0.022).
- There were no differences between groups in TLF from 1 year to 3 years follow-up (2-stent 4.3 % vs. PS 4.6 %, HR 0.87, 95 % CI 0.41-1.82, p = 0.703).
Critical reading and the relevance for clinical practice
The results of this study demonstrate that the one-year results of DEFINITION II showing that a two-stent technique is superior to a provisional approach in true complex bifurcations are maintained at three-year follow-up.
Interestingly, landmark analysis shows that the TLF rates differ significantly at 30-day follow-up (3.0 % vs. 7.4 %, HR 0.41, 95% CI 0.20-0.85, p = 0.017) and whilst the cumulative difference persists to 3-year follow-up, there are no significant differences between the rates of TLF or its components from 31 days to 1 year or 1 to 3 years between the groups.
In the provisional strategy group, those treated with a second stent had higher rates of TLF from 1-3 years compared to those treated with 1 stent (2 stents 9.6 % vs 1-stent 33.2 %, HR 3.13, 95 % CI 1.14-8.64 p = 0.027). This was due to increased rates of clinically driven TLR in the 2-stent group (6.8 % vs. 1.6 %, HR 4.45, 95 % CI 1.19-16.52, p = 0.026), whilst small numbers, it raises questions with regard to the durability of the results. Patients with intraprocedural complications had a higher rate of TLF at one year compared to those without however there were no differences from 1 to 3 years.
A note of caution when interpreting the results, one must bear in mind that all bifurcations were complex with significant stenoses in important side branches; therefore, not generalisable to all bifurcations. DK Crush was the most commonly used two-stent technique, however, the study was not powered to demonstrate differences between two-stent techniques.
The increased rates of TLR from 1-3 years in the PS group who were treated with a second stent draws attention to the importance of meticulous attention to detail in all procedural steps to ensure durability of the procedure. Overall, rates of IVUS were low and its use for pre-procedural planning as well as stent optimisation may improve outcomes.
In summary, DEFINITION-II adds to the evidence that an upfront 2-stent strategy may be most appropriate in true complex bifurcation lesions. Given that there was no increased benefit from the 2-stent approach from one to three years, attention needs to be paid to the initial assessment of the lesion, appropriate plaque preparation, and meticulous attention to detail at each stage of the procedure to ensure an optimal result at initial stent implantation.






No comments yet!