04 Jan 2022
Defining percutaneous coronary intervention complexity and risk: an analysis of the UK BCIS Database 2006-2016
Selected in JACC: Cardiovascular Interventions by S. Brugaletta
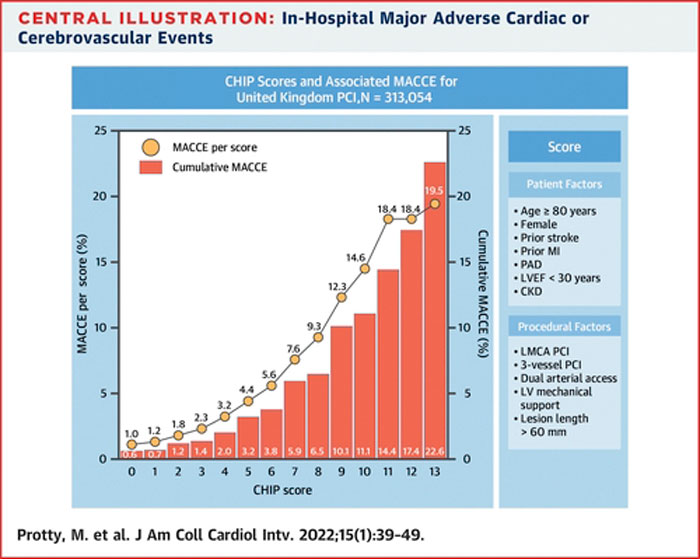
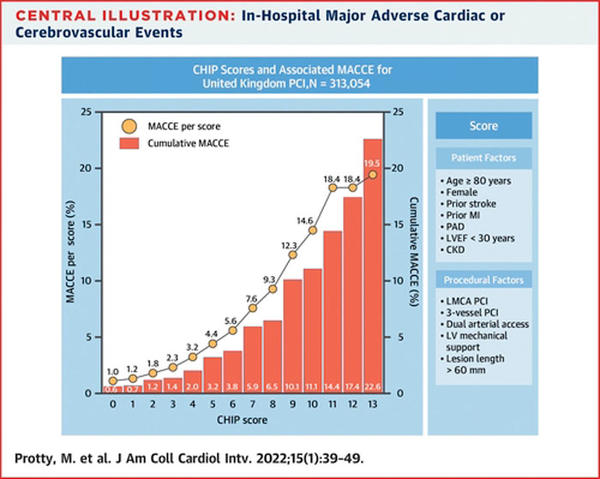
A multiple logistic regression model was developed to identify variables associated with in-hospital MACCE and to construct a CHIP score. The cumulative effect of this score on patient outcomes was examined.
References
Authors
Majd Protty, Andrew S.P. Sharp, Sean Gallagher, Vasim Farooq, James C. Spratt, Peter Ludman, Richard Anderson, Margaret M. McEntegart, Colm Hanratty, Simon Walsh, Nick Curzen, Elliot Smith, Mamas Mamas, and Tim Kinnaird
Reference
J Am Coll Cardiol Intv. 2022 Jan, 15 (1) 39–49
Published
January 2022
Link
Read the abstract
Reviewer
My Comment
Why this study – the rationale/objective?
Complex high-risk indicated percutaneous coronary intervention (CHIP-PCI) is an emerging concept that is poorly defined.
In particular, it is difficult to define difficulties of such procedure and how they may be related to events.
The authors used the BCIS (British Cardiovascular Intervention Society) database to define the factors associated with percutaneous coronary intervention (PCI) procedural complexity.
How was it executed? - the methodology
The BCIS (British Cardiovascular Intervention Society) database was used to study all PCI procedures in the United Kingdom 2006-2016.
A multiple logistic regression model was developed to identify variables associated with in-hospital major adverse cardiac or cerebrovascular events (MACCE) and to construct a CHIP score. The cumulative effect of this score on patient outcomes was examined.
What is the main result?
A total of 313,054 patients were included.
Seven patient factors (age ≥ 80 years, female sex, previous stroke, previous myocardial infarction, peripheral vascular disease, ejection fraction < 30 %, and chronic renal disease) and 6 procedural factors (rotational atherectomy, left main PCI, 3-vessel PCI, dual arterial access, left ventricular mechanical support, and total lesion length > 60 mm) were associated with increased in-hospital MACCE and defined as CHIP factors.
The mean CHIP score/case for all PCIs increased significantly from 1.06 ± 1.32 in 2006 to 1.49 ± 1.58 in 2016 (P < 0.001 for trend).
A CHIP score of 5 or more was present in 2.5 % of procedures in 2006, increasing to 5.3 % in 2016 (P < 0.001 for trend).
Overall in-hospital MACCE was 0.6 % when the CHIP score was 0 compared with 1.2 % with any CHIP factor present (P < 0.001).
As the CHIP score increased, an exponential increase in-hospital MACCE was observed.
The cumulative MACCE for procedures associated with a CHIP score 4+ or above was 3.2 %, and for a CHIP score 5+ was 4.4 %.
All other adverse clinical outcomes were more likely as the CHIP score increased.
Source: JACC - Cardiovascular Interventions
Critical reading and the relevance for clinical practice
The attention of the interventional cardiology community has increased during the last years on the so-called CHIP procedures, which are complex and high-risk PCI procedures.
Although there are been many attempts to define such procedures, it is still difficult to identify which factors are related to them and how they may influence the prognosis.
This paper is indeed a good way to start defining them beyond a simple definition, by identifying clinical and procedural factors associated either with procedural complexity or with in-hospital events.
A couple of points should be made:
- First it would have been interesting to know how this score may be related to events beyond in-hospital time frame.
- Second, although we cannot modify patient factors, it may be interesting to understand how we may reduce the risk related to procedural factors, making these procedures safer and less risky: operator experience, one-access Impella, high use of radial approach may be useful?