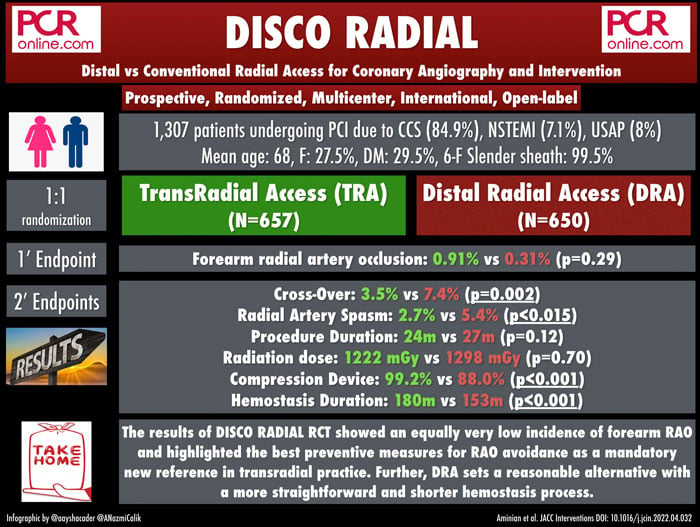
Distal versus conventional radial access for coronary angiography and intervention (DISCO RADIAL)
Selected in JACC: Cardiovascular Interventions by A. Cader , A. N. Calik
The DISCO RADIAL trial sought to assess the efficacy and safety of distal radial access (DRA) compared with conventional transradial access (TRA) with systematic implementation of best prevention methods for the reduction of radial artery occlusion (RAO).
References
Authors
Adel Aminian, Gregory A. Sgueglia, Marcus Wiemer, Joëlle Kefer, Gabriele L. Gasparini, Zoltan Ruzsa, Maarten A.H. van Leeuwen, Claudiu Ungureanu, Gregor Leibundgut, Bert Vandeloo, Sasko Kedev, Ivo Bernat, Karim Ratib, Juan F. Iglesias, Elias Al Hage, Giuseppe A. Posteraro, Dan Pascut, Frederic Maes, Damiano Regazzoli, Kornél Kakonyi, Thomas A. Meijers, Giuseppe Colletti, Lian Krivoshei, Stijn Lochy, Biljana Zafirovska, David Horák, James Nolan, Sophie Degrauwe, Kazuki Tobita, and Shigeru Saito
Reference
J Am Coll Cardiol Intv. May 17, 2022. Epublished DOI: 10.1016/j.jcin.2022.04.032
Published
17 May 2022
Link
Read the abstract
Reviewers
Our Comment
Why this study - the rationale / objective:
Transradial access (TRA) is the standard vascular access for percutaneous coronary interventions, and a #Radialfirst strategy is strongly recommended by the European and American cardiac society guidelines.
Clinical benefits of TRA, including reduced access-site bleeding and vascular complications, are offset by radial artery occlusion (RAO), which is one of the most frequent complications of TRA.
Further, an occluded radial artery will not be suitable for surgical use or re-access for future coronary or non-coronary interventions.
As the real-world RAO incidence remains high, even in the experienced centers, distal radial access (DRA) in the anatomical snuff box or the dorsum of the hand has emerged as a promising alternative access to further reduce the risk for RAO.
The DISCO RADIAL trial sought to assess the efficacy and safety of DRA compared with conventional TRA with systematic implementation of best prevention methods for the reduction of RAO1.
The primary hypothesis of the study was that DRA is superior to conventional TRA with respect to the incidence of forearm RAO at discharge.
How was it executed? - the methodology:
The DISCO RADIAL is a prospective, multicenter, international, open-label RCT, sponsored by Terumo Europe.
Only operators regularly performing transradial PCI in the whole spectrum of coronary artery disease, including acute coronary syndrome, and who performed a minimum of 100 DRA (fully independent with DRA), were qualified for the study.
A 6-F Glidesheath Slender (Terumo) was used as the standard access sheath.
Exclusion criteria included long-term hemodialysis, ST-segment elevation myocardial infarction, and PCI for chronic total occlusion.
Eligible patients were randomly assigned in a 1:1 ratio to DRA vs TRA.
The choice of right or left radial artery was left to the operator's discretion, as was the use of ultrasound to guide arterial puncture.
After placement of the 6-F Glidesheath Slender, it was highly recommended to administer 5 mg verapamil and / or 100 to 200 mg nitroglycerin to prevent arterial spasm.
Also, all patients received an initial bolus of 5,000 IU unfractionated heparin, with an adjunctive bolus, if needed, to achieve an activated clotting time of 250 to 300 seconds according to current best practice.
If the initial attempt to obtain vascular access at the randomized access site (DRA or conventional TRA) failed, all further attempts to obtain vascular access at another site in the same limb or in another limb were considered as crossover.
Hemostasis with an air-filled closure device was recommended for the conventional TRA group with patent hemostasis implemented according to the PROPHET (Prevention of Radial Artery Occlusion— Patent Hemostasis Evaluation Trial) protocol.
For DRA, hemostasis was per hospital practice.
The primary endpoint was the incidence of forearm RAO at hospitalization discharge, which was accessed with duplex ultrasound performed between 8 and 48 hours post procedurally.
The secondary endpoints included successful sheath insertion, access-site crossover, sheath insertion time, procedure time, overall bleeding defined according to the Bleeding Academic Research Consortium (BARC) criteria, puncture site bleeding defined according to the EASY (Early Discharge After Transradial Stenting of Coronary Arteries Study) criteria, vascular access-site complications, radial artery spasm, access-related pain rated according to self-reported visual analog scale, and time to hemostasis.
What is the main result?
A total of 1,309 patients were randomized at 15 sites in Europe and 1 site in Japan.
The occurrence rate of forearm RAO, analyzed by intention-to-treat (ITT) was strikingly low, and similar between TRA and DRA groups (0.91 % vs 0.31 %; p = 0.29). A per-protocol (PP) analysis, which excluded crossovers and major protocol violations, also showed no differences in RAO between TRA and DRA (0.81 % vs 0.34 %; p = 0.45).
Distal RAO in the DRA group was 0.46 %.
As for secondary outcomes, cross-over (3.5 % vs 7.4 %; p = 0.002) and radial artery spasm (2.7 % vs 5.4 %; p < 0.015) were more frequent in DRA group.
On the other hand, selective compression device usage was more common in the TRA group (99.2 % vs 88.0 %; p < 0.001), and the median time to hemostasis was longer in patients undergoing TRA (180 min. vs 153 min.; P < 0.0001).
Patent hemostasis was achieved in 94.4 % of TRA patients.
There were no differences in bleeding (5.5 % vs 6.8 %; p = 0.33) and vascular complications (1.2 % vs 1.1 %; p = 0.81) between conventional TRA and DRA.
All analyses in the PP population revealed consistent results.
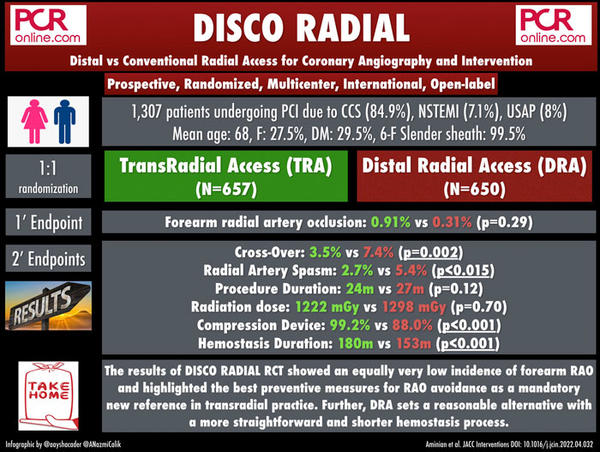
Source: courtesy of Aaysha Cader & Ali Nazmi Calik
Critical reading and the relevance for clinical practice:
The DISCO RADIAL trial found equally low forearm RAO rates with both DRA and TRA, with the implementation of a rigorous hemostasis protocol following current best practice recommendations.
These rates of RAO were much lower than the estimates of 3.5 % and 1.0 % used for TRA vs DRA respectively, and thus a type II error rate inflation might be attributed to these non-significant differences between the two groups.
The fact that RAO rates after DRA remain low even when compared to the best practice TRA protocols is noteworthy.
These best practices include the use of 6 French Glidesheath slender (with the reduced outer diameter and known to reduce RAO as per the RAP and BEAT trial)2, the use of patent hemostasis (demonstrated to reduce RAO by PROPHET trial)3, and adequate procedural anticoagulation.
The Glidesheath slender use is of particular value in DRA, which has a narrower diameter than the proximal radial artery.
Also, the significantly shorter hemostasis time following DRA is also a determinant of the very low forearm RAO rates.
Two prior randomized controlled trials have evaluated forearm RAO as the primary endpoint between DRA and conventional TRA4,5.
In the DAPRAO (Distal Radial Approach to Prevent Radial Artery Occlusion) trial, RAO was 1.2 % vs 8.8 % in the DRA and TRA arms respectively4.
In the ANGIE (Anatomical Snuffbox for Coronary Angiography and Interventions) trial, 60-day RAO rates were 3.7 % vs 7.9 % for DRA and TRA respectively5.
These trials were limited by their single-center nature and lack of implementation of best practices.
Also, a 7.4 % crossover rate from DRA to conventional TRA in DISCO RADIAL despite considerable operator expertise speaks to one of the limitations of uptake of DRA in regular clinical practice, and its associated learning curve in comparison to TRA.
However, crossover rates were still much lower than in DAPRAO, where crossover to TRA was 13.3 %, and ANGIE, where it was as high as 22.3 %.
Perhaps the biggest limitation of this trial is its conservative estimation of RAO rates during sample size calculation.
It’s possible that the lower than anticipated incidence of RAO in both groups may have led to the difference between groups being nonsignificant when it actually is significant.
Despite higher crossover and spasm, the fact that bleeding and procedural variables were similar between arms, on the background of similar RAO rates renders DRA as a valid alternative access for transradial interventions.
What do you see as issues leading to low uptake of DRA in your practice?
References
- Aminian A, Sgueglia GA, Wiemer M, et al. Distal Versus Conventional Radial Access for Coronary Angiography and Intervention (DISCO RADIAL). JACC Cardiovasc Interv. 2022 May 10:S1936-8798(22)00897-4.
- Aminian A, Saito S, Takahashi A, et al. Comparison of a new slender 6 Fr sheath with a standard 5 Fr sheath for transradial coronary angiography and intervention: RAP and BEAT (Radial Artery Patency and Bleeding, Efficacy, Adverse Event), a randomized multicentre trial. EuroIntervention. 2017;13:e549–e556.
- Pancholy S, Coppola J, Patel T, Roke-Thomas M. Prevention of radial artery occlusion patient hemostasis evaluation trial (PROPHET study): a randomized comparison of traditional versus patency documented hemostasis after transradial catheterization. Catheter Cardiovasc Interv. 2008;72:335–340
- Eid-Lidt G, Rivera Rodriguez A, Jimenez Castellanos J, et al. Distal Radial Artery Approach to Prevent Radial Artery Occlusion trial. J Am Coll Cardiol Intv.2021;14:378–385.
- Tsigkas G, Papageorgiou A, Moulias A, et al. Distal or traditional transradial access site for coronary procedures: a single-center, randomized study. J Am Coll Cardiol Intv. 2022;15:22–32.





No comments yet!