EROSION III: a multicenter RCT of OCT-guided reperfusion in STEMI with early infarct artery patency
Selected in JACC: Cardiovascular Interventions by S. Brugaletta
This is an interesting study showing that in patients with STEMI with early infarct artery patency, OCT guidance compared with angiographic guidance of reperfusion was associated with less stent implantation during primary PCI.
References
Authors
Haibo Jia, Jiannan Dai, Luping He, Yishuo Xu, Yongfeng Shi, Lei Zhao, Zhiqi Sun, Yin Liu, Ziqian Weng, Xue Feng, Dirui Zhang, Tao Chen, Xiling Zhang, Lulu Li, Yousheng Xu, Yanqing Wu, Yining Yang, Chunmei Wang, Lang Li, Jianping Li, Jingbo Hou, Bin Liu, Gary S. Mintz, and Bo Yu
Reference
J Am Coll Cardiol Intv. 2022 Apr, 15 (8) 846–856
Published
15 April 2022
Link
Read the abstract
Reviewer
My Comment
Why this study – the rationale/objective?
Angiography is limited in assessing the underlying pathophysiological mechanisms of the culprit lesion.
The aim of this study was to test whether optical coherence tomographic (OCT) guidance would provide additional useful information beyond that obtained by angiography and lead to a shift in reperfusion strategy and improved clinical outcomes in patients with ST-segment elevation myocardial infarction (STEMI) with early infarct artery patency.
How was it executed? - the methodology
EROSION III (Optical Coherence Tomography–Guided Reperfusion in ST-Segment Elevation Myocardial Infarction With Early Infarct Artery Patency) is an open-label, prospective, multicenter, randomized, controlled study approved by the ethics committees of participating centers.
Patients with STEMI who had angiographic diameter stenosis > 70 % and TIMI (Thrombolysis In Myocardial Infarction) flow grade 3 at presentation or after antegrade blood flow restoration were recruited and randomized to either OCT guidance or angiographic guidance.
The primary efficacy endpoint was the rate of stent implantation.
What is the main result?
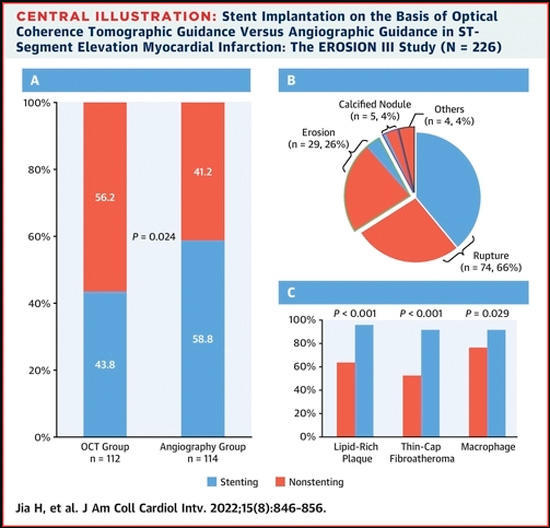
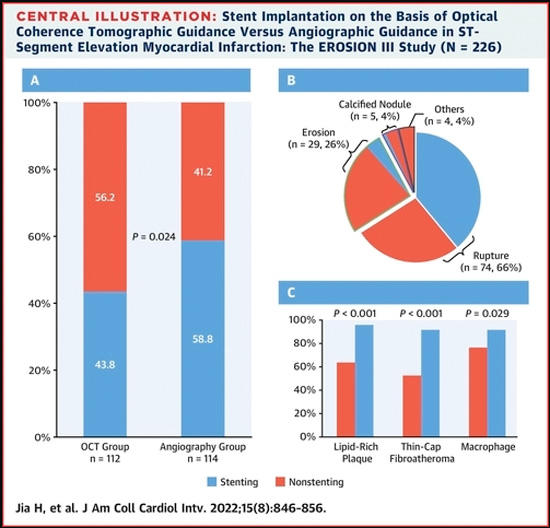
Among 246 randomized patients, 226 (91.9 %) constituted the per-protocol set (112 with OCT guidance and 114 with angiographic guidance).
The median diameter stenosis was 54.0 % (IQR: 48.0 %-61.0 %) in the OCT guidance group, and 53.5 % (IQR: 43.8 %-64.0 %) in the angiographic guidance group (P = 0.57) before randomization.
Stent implantation was performed in 49 of 112 patients (43.8 %) in the OCT group, and 67 of 114 patients (58.8 %) in the angiographic group (P = 0.024), demonstrating a 15 % reduction in stent implantation with OCT guidance.
In patients treated with stent implantation, OCT guidance was associated with a favorable result with lower residual angiographic diameter stenosis (8.7 % 3.7 % vs 11.8 % 4.6 % in the angiographic guidance group; P < 0.001).
Two patients (1 cardiac death, 1 stable angina) met the primary safety endpoint in the OCT guidance group, as did 3 patients (3 cardiac deaths) in the angiographic guidance group (1.8 % vs 2.6 %; P = 0.67).
Reinfarction was not observed in either group.
At 1 year, the rates of predefined cardiocerebrovascular events were comparable between the groups (11.6 % after OCT guidance vs 9.6 % after angiographic guidance; P = 0.66).
Source: JACC - Cardiovascular Interventions
Critical reading and the relevance for clinical practice?
This is an interesting study showing that in patients with STEMI with early infarct artery patency, OCT guidance compared with angiographic guidance of reperfusion was associated with less stent implantation during primary percutaneous coronary intervention.
This result was possible because of the identification by OCT of larger minimal luminal areas, less severe area stenosis, and smaller lipid arcs.
This is one of the first times OCT is shown to be able to guide treatment in an acute setting, by identifying those culprit lesions which require stent implantation and those which can be left with medical treatment.
Importantly, there were no differences in clinical events at 1-year follow-up, although the small number of patients included does not allow to draw definite conclusions.
To translate this study into clinical practice, we would need an OCT expert in every site in order to analyze pullbacks of ACS patients. Unfortunately not every center has OCT or a 24h/7days OCT expert available.
-> Are we ready for customizing stenting in ACS based on OCT?




No comments yet!