09 Feb 2022
Frequency and outcomes of periprocedural MI in patients with chronic coronary syndromes undergoing PCI
Selected in Journal of the American College of Cardiology by S. Brugaletta
This study evaluated the frequency and impact of periprocedural MI by using various MI definitions among patients with chronic coronary syndrome (CCS) undergoing percutaneous coronary intervention (PCI).
References
Authors
Yasushi Ueki, Tatsuhiko Otsuka, Sarah Bär, Kostantinos C. Koskinas, Dik Heg, Jonas Häner, George C.M. Siontis, Fabien Praz, Lukas Hunziker, Jonas Lanz, Stefan Stortecky, Thomas Pilgrim, Sylvain Losdat, Stephan Windecker, and Lorenz Räber
Reference
J Am Coll Cardiol. 2022 Feb, 79 (6) 513–526
Published
February 2022
Link
Read the abstract
Reviewer
My Comment
Why this study – the rationale/objective?
Definitions of periprocedural myocardial infarction (MI) differ with respect to biomarker threshold as well as ancillary criteria for myocardial ischemia and are limited in terms of validation.
This study evaluated the frequency and impact of periprocedural MI by using various MI definitions among patients with chronic coronary syndrome (CCS) undergoing percutaneous coronary intervention (PCI).
How was it executed? - the methodology
Between 2010 and 2018, periprocedural MIs were assessed according to the third and fourth Universal Definition of Myocardial Infarction (UDMI), Academic Research Consortium-2 (ARC-2), and Society for Cardiovascular Angiography and Interventions (SCAI) criteria based on high-sensitivity troponin in patients with CCS undergoing PCI enrolled into the Bern PCI registry.
The primary endpoint was cardiac death at 1 year.
What is the main result?
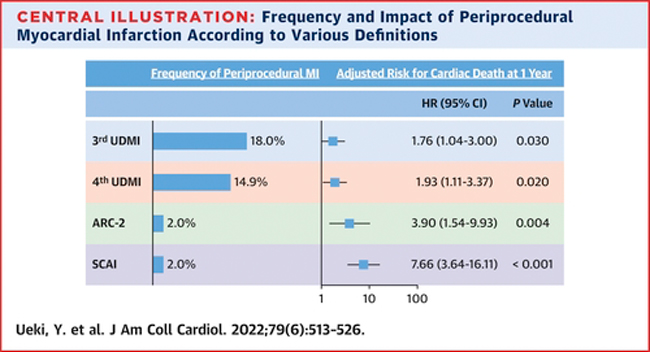
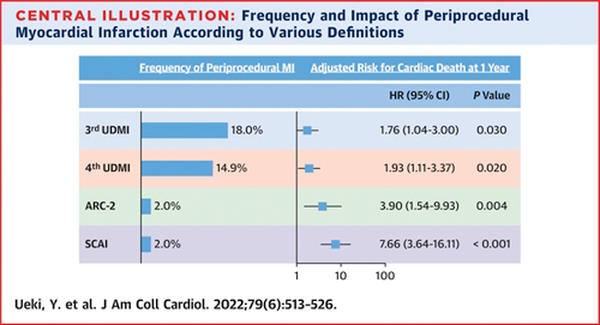
Among 4,404 patients with CCS, periprocedural MI defined by the third UDMI, fourth UDMI, ARC-2, and SCAI were observed in 18.0 %, 14.9 %, 2.0 %, and 2.0 % of patients, respectively.
Among patients with periprocedural MI defined by the third UDMI, fourth UDMI, ARC-2, and SCAI, cardiac mortality at 1 year was 2.9 %, 3.0 %, 5.8 %, and 10.0 %. The ARC-2 (HR: 3.90; 9 5% CI: 1.54-9.93) and SCAI (HR: 7.66; 95 % CI: 3.64-16.11) were more relevant compared with the third UDMI (HR: 1.76; 95 % CI: 1.04-3.00) and fourth UDMI (HR: 1.93; 95 % CI: 1.11-3.37) for cardiac death at 1 year.
Source: JACC
Critical reading and the relevance for clinical practice
This is a very interesting study for understanding the weight of each periprocedural MI definition in determining cardiac death at 1-year follow-up.
There is always a debate within the interventional cardiology community on how to define a periprocedural MI and there are indeed many definitions that are differently used in various studies.
This study shows that the incidence of periprocedural MI may vary much according to the definition used and that its relationship with cardiac death at 1-year is very wide. Periprocedural MI defined according to the 3rd UDMI definition is for example very frequent (up to 18 %), but contributes a little to the risk of cardiac death at 1-year. On the contrary, periprocedural MI defined according to SCAI criteria has an incidence of 2 %, but contributes a lot to the risk of developing a cardiac death at 1-year.
These considerations are important to take in mind either in trial design or in daily clinical practice. In the latter periprocedural MIs are rarely diagnosed, but given the result of the present study, it may be of renewed interest to look at them, given their close relationship with 1-year cardiac death.