Leaflet-to-annulus index and residual tricuspid regurgitation following tricuspid transcatheter edge-to-edge repair
Selected in EuroIntervention by J. Curio , A. Sticchi , G. Tang
As the relationship between leaflet length and annular dimension becomes highly relevant in TR pathophysiology, the present study aimed to evaluate the impact of tricuspid leaflet-to-annulus mismatch on outcomes after T-TEER.
References
Authors
Tetsu Tanaka, Atsushi Sugiura, Refik Kavsur, Johanna Vogelhuber, Can Öztürk, Marc Ulrich Becher, Sebastian Zimmer, Georg Nickenig, Marcel Weber
Reference
EuroIntervention. 2022 Jun 3;18(2):e169-e178
Published
June 2022
Link
Read the abstract
Reviewers
Our Comment
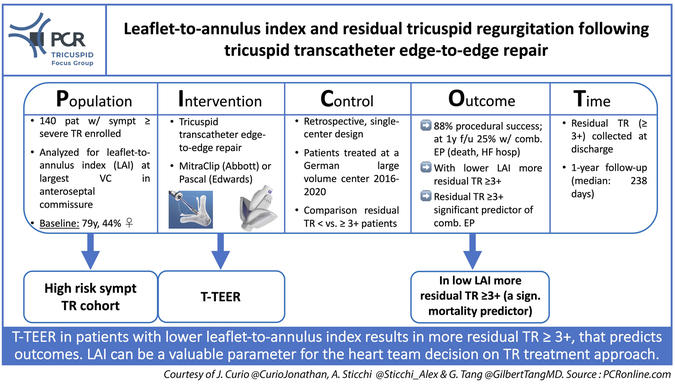
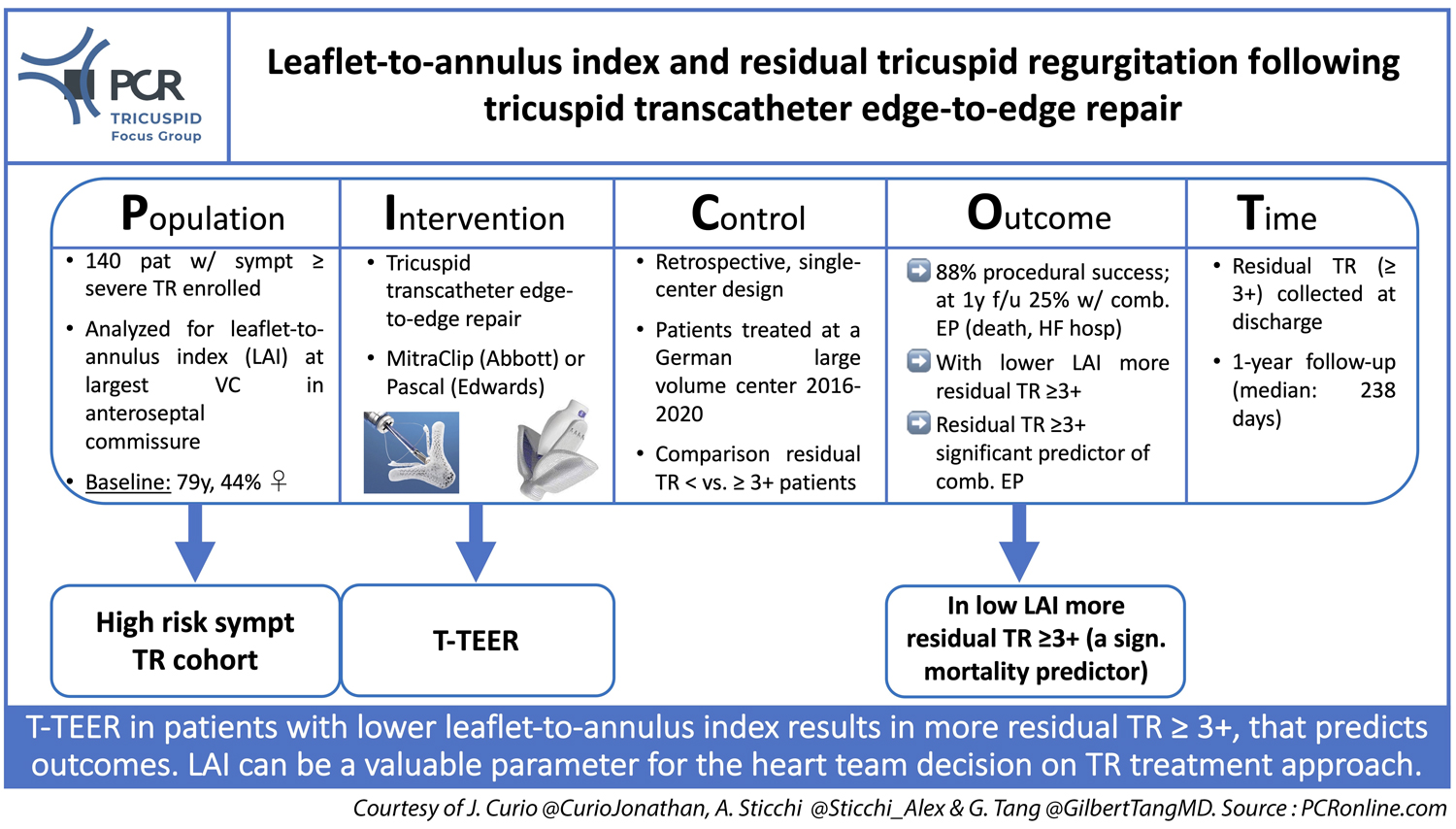
Picot scheme highlighting key aspects of the study. Courtesy of Jonathan Curio, Alessandro Sticchi, and Gilbert Tang
Why this study – the rationale/objective?
Recently, several transcatheter approaches to treat tricuspid regurgitation (TR) have gained increasing adoption given their safety and efficacy, with tricuspid transcatheter edge-to-edge repair (T-TEER) currently having the largest experience and highest number of patients treated1. However, given the availability of several different approaches (TEER, annuloplasty, replacement) and anatomic heterogeneity, to better the selection of the most appropriate device, it is important to understand different clinical and anatomic TR features. As the relationship between leaflet length and annular dimension becomes highly relevant in TR pathophysiology, the present study aimed to evaluate the impact of tricuspid leaflet-to-annulus mismatch on outcomes after T-TEER.
How was it executed? - the methodology
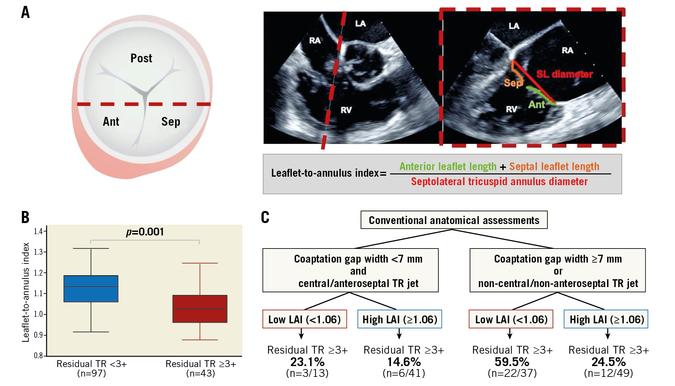
140 patients underwent T-TEER (MitraClip, Abbott Vascular; Pascal system, Edwards Lifesciences) between 2015 and 2020 at a single high-volume center. In these patients, a leaflet-to-annulus index (LAI) was calculated by dividing length of anterior and septal tricuspid leaflets by septolateral length of the tricuspid annulus at the position of the widest vena contracta in midsystole.
- Primary endpoint was significant residual TR, defined as discharge TR ≥ 3+
- Secondary endpoint was a composite of all-cause mortality and HF hospitalizations within 1-year follow-up
Source: EuroIntervention
What is the main result?
44% of patients were women, mean age was 79 years. TR was 3+ (severe) in 59%, 4+ (massive) in 36% and 5+ (torrential) in 8%. 89% presented with NYHA functional class III/IV.
79% of cases were performed with MitraClip/TriClip, and 21% were treated using PASCAL. Acute procedural success was achieved in 88%, while discharge TR ≥ 3+ was found in 31%.
During 1 year after the procedure (median follow-up: 238 days) 18 patients died and 25 patients were hospitalized for heart failure (25% experiencing composite secondary endpoint). TR ≥ 3+ was a significant predictor of the composite outcome.
Key findings regarding the impact of LAI were:
- Patients with residual TR ≥ 3+ had lower LAI (1.0 vs. 1.13 in discharge TR < 3+), based on numerically greater annuli
- In multivariable models with geometric variables and cardiac parameters, LAI remained a significant predictor of residual TR ≥ 3+ and was associated with procedural success in the univariate model
- ROC curve analysis was used to identify an LAI cut-off of 1.06 predicting residual TR ≥ 3+; this cut-off was able to further increase the predictive value of conventional risk markers (coaptation gap width < 7mm, and central/anteroseptal TR jet present or not, respectively)
- Also, posteroseptal and anteroposterior commissure LAIs were evaluated but were not associated with residual TR ≥ 3+
Critical reading and the relevance for clinical practice
Several relevant factors to consider in device selection for transcatheter TR treatment have been identified and were recently summarized in a concise guiding flowchart by the PCR Tricuspid Focus Group, where a coaptation gap ≤ 8.5mm, a commissural jet location, and only mild/moderate tethering were reported as factors favoring T-TEER treatment2.
The authors of the present study provide a valuable additional tool to stratify the probability of procedural success, via residual TR impacting hard treatment outcomes. LAI adds a further perspective to the anatomical evaluation of TR patients as it integrates the pathophysiological interconnection between annular dilation and missing leaflet reserve to further support successful coaptation. That said, it is important to note that LAI in the present study did not directly impact outcomes, but only influenced residual TR, which is an established predictor of worse clinical outcomes3.
Interestingly, while right ventricular diameters were without significant difference, right atrial area was significantly larger in patients with residual TR ≥ 3+ (namely, the group showing smaller LAI). This may be caused by continuous volume load to the RA or this may also represent a profile of atrial functional TR, as previously described4.
However, several additional parameters would be of interest:
- Achievable leaflet grasping and leaflet insertion might differ between patients with high or low LAI.
- As in T-TEER an annuloplasty-like effect can be observed, it would be interesting to know if any/which group of patients, when stratified per LAI, shows more of this effect
- LAI measurements are taken at only one position of regurgitation (largest coaptation gap in anteroseptal commissure), however, as TR pathologies can be very complex with multiple jets and large areas of lacking coaptation, an approach correlating leaflet area of all leaflets and annular area might stratify patients even more precisely
In conclusion, for heart teams evaluating TR patients and deciding on the most promising treatment approach, the present study adds the importance of LAI assessment, allowing a more quantitative prediction of achievable treatment response following T-TEER, especially in terms of TR reduction.
References
- Lurz P, Stephan von Bardeleben R, Weber M et al. Transcatheter Edge-to-Edge Repair for Treatment of Tricuspid Regurgitation. J Am Coll Cardiol 2021;77:229-239.
- Praz F, Muraru D, Kreidel F et al. Transcatheter treatment for tricuspid valve disease. EuroIntervention 2021;17:791-808.
- Mehr M, Taramasso M, Besler C et al. 1-Year Outcomes After Edge-to-Edge Valve Repair for Symptomatic Tricuspid Regurgitation: Results From the TriValve Registry. JACC Cardiovasc Interv 2019;12:1451-1461.
- Muraru D, Addetia K, Guta AC et al. Right atrial volume is a major determinant of tricuspid annulus area in functional tricuspid regurgitation: a three-dimensional echocardiographic study. Eur Heart J Cardiovasc Imaging 2021;22:660-669.









No comments yet!