MIRACLE 2 score and SCAI grade to identify patients with out-of-hospital cardiac arrest for immediate coronary angiography
Selected in JACC: Cardiovascular Interventions by E. Asher
The purpose of the current study was to evaluate the impact of performing immediate CAG post-OHCA with stratification of predicted neurologic injury and cardiogenic shock on arrival to a center.
References
Authors
Nilesh Pareek, Nicholas Beckley-Hoelscher, Ritesh Kanyal, Antonio Cannata, Peter Kordis, Nicholas Sunderland, Ali Kirresh, Joanne Nevett, Rachael Fothergill, Ian Webb, Rafal Dworakowski, Narbeh Melikian, Sundeep Kalra, Thomas W. Johnson, Gianfranco Sinagra, Serena Rakar, Marko Noc, Ajay M. Shah, Jonathan Byrne, and Philip MacCarthy
Reference
J Am Coll Cardiol Intv. 2022 May, 15 (10) 1074–1084
Published
15 May 2022
Link
Read the abstract
Reviewer
My Comment
Why this study – the rationale/objective?
The role of immediate coronary angiography (CAG) for patients with out-of-hospital cardiac arrest (OHCA) is unclear, which may be explained, in part, by the majority of patients dying of hypoxic brain injury.
The purpose of the current study was to evaluate the impact of performing immediate CAG post-OHCA with stratification of predicted neurologic injury and cardiogenic shock on arrival to a center.
How was it executed? - the methodology
Between May 2012 and July 2020, patients from 5 European centers were included in the European Cardiac Arrest Registry.
Inclusion criteria:
Patients older than 18 years who presented with OHCA and return of spontaneous circulation (ROSC) in the field.
Exclusion criteria:
Patients who died before or on arrival to a center, with any evidence of an obvious noncardiac cause of arrest (suicide, trauma, drowning, substance overdose), and those with suspected or imaging confirmed intracerebral bleeding, known neurologic disability.
Standardized systematic protocols:
Patients with OHCA with ROSC
- If ST-Segment elevation on ECG - taken directly to a catheterization laboratory
- All other patients - emergency department and then referred to a specialist center within a 2-hour time frame. On arrival, a decision to perform immediate CAG is made by the admitting interventional cardiologist.
- Immediate CAG was classified as receiving invasive CAG and revascularization if required within a 2-hour time frame.
- Patients not receiving this treatment were classified as receiving an initial conservative approach.
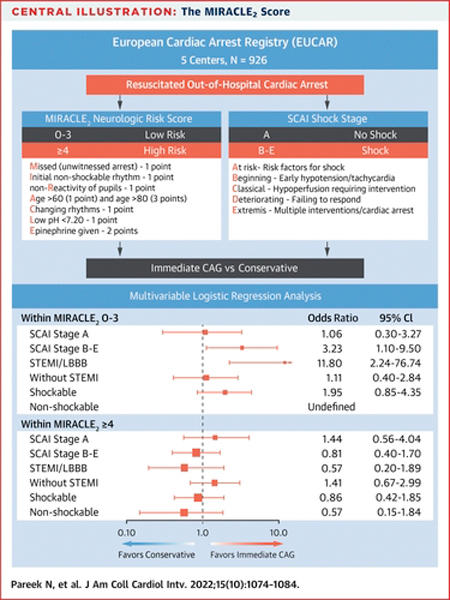
MIRACLE2 SCORE AND SCAI SHOCK CLASSIFICATION
The MIRACLE2 score is a bedside risk score that was designed in accordance with the Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis guidelines, and includes 7 variables to predict poor long-term neurologic outcomes after OHCA:
- Missed (Unwitnessed arrest) – 1 point
- Initial non-shockable rhythm – 1 point
- non-Reactivity of pupils – 1 point
- Age > 60 (1 point) and > 80 (3 points)
- Changing rhythms – 1 point
- Low pH < 7.20 – 1 point
- Epinephrin given – 2 points
Patients were retrospectively classified into low vs high neurologic risk (MIRACLE2 score 0-3 which correlates with a risk of < 50 % for a poor outcome vs. ≤ 4) and degree of cardiogenic shock on arrival (Society for Cardiovascular Angiography and Interventions [SCAI] grade A vs B-E) at risk, beginning shock, classic shock, deteriorating shock, and extremis.
A multivariable logistic regression analysis including immediate CAG was performed for the primary outcome of survival with good neurologic outcome (Cerebral Performance Category 1 or 2) at hospital discharge.
Outcomes:
The primary endpoint was survival with good neurologic outcome, classified as cerebral performance category (CPC) 1 or 2 (none to mild disability) at hospital discharge.
(CPC 1 – normal function; CPC 2 – moderate impairment but with independent living; CPC 3 – consciousness with severe impairment; CPC 4 – persistent coma, and CPC 5 – death).
What is the main result?
- One thousand two hundred and forty-six patients had OHCA with sustained ROSC. Of these, 237 had incomplete data to perform MIRACLE2 scoring, and 83 had Glasgow Coma Scale scores of 15, hence 926 were included in the final analysis.
- Approximately one half of the patients had cardiac arrest at home (n = 496 of 921 [53.9 %]), and 705 patients (76.1 %) had initial shockable rhythms.
- A total of 568 patients (61.3 %) had SCAI grade B to E cardiogenic shock on admission.
- There were 480 of 918 patients (52.3 %) with STEMI or left bundle branch block on admission ECG.
- A total of 686 of 926 patients (74.1 %) had immediate CAG, and of these, 450 (65.6 %) had culprit coronary lesions.
- Percutaneous coronary intervention (PCI) was performed in 420 of 686 patients (61.2 %).
- The primary endpoint of survival with good neurologic outcome on hospital discharge occurred in 391 of 926 patients (42.2 %).
- Four hundred five patients (44.0 %) were in the low MIRACLE2 risk group and 521 (56.0 %) in the high-risk group.
- There was a substantial and highly significant difference in the primary endpoint between low- and high-risk MIRACLE2 groups (76.5 % vs 15.5 %; P < 0.0001).
- In the entire cohort, immediate CAG was not significantly associated with survival with good neurologic outcome (P = 0.437); was not significantly associated with good outcome in the low (P = 0.121) or high (P = 0.948) MIRACLE2 group. Was also not associated with improved outcome in the multivariable logistic regression in a sensitivity analysis of the prespecified subgroups. Moreover, it was not associated with better outcomes in STEMI patients (p = 0.371); patients without STEMI (p = 0.337); or in those with cardiogenic shock (p = 0.5).
- In the 405 patients in the low MIRACLE2 risk group, immediate CAG was significantly associated with survival with good outcome in those presenting with cardiogenic shock (OR: 3.23; 95 % CI: 1.10-9.50; P = 0.031) and in those with STEMI (OR: 11.80; 95 % CI: 2.24-76.74; P = 0.048).
- In contrast, stratification based on the high-risk MIRACLE2 group showed that none of these prespecified subgroups appeared to achieve any benefit from immediate CAG.
Immediate CAG vs. conservative
Source = JACC: Cardiovascular Interventions
Critical reading and the relevance for clinical practice
The major finding of the current study is that Immediate CAG was associated with survival with improved neurologic outcome at hospital discharge in selected patients with OHCA with favorable prediction of neurologic recovery (MIRACLE2 score 0-3), cardiogenic shock (SCAI grades B-E) and/or STEMI on arrival.
Although RCT evidence supports coronary revascularization in patients with cardiogenic shock, these studies did not specifically include patients with OHCA. Hence, early classification of patients at low risk for neurologic injury but with cardiogenic shock might identify subgroups of patients who might benefit most from an immediate invasive approach.
In this study, the findings indicate that an immediate invasive approach is most warranted in a cohort of patients at low risk for neurologic injury but also with STEMI on admission and significant hemodynamic instability.
The lack of any association of immediate CAG with improved neurologic outcome in the high-risk group (or in any of the sensitivity analyses based on admission characteristics within this group - including STEMI), might be explained by a higher inherent risk for neurologic injury in this patient group, rendering them potentially futile to the benefits of coronary revascularization.
This might also suggest that one can identify subgroups of patients who might benefit most from an immediate invasive approach after OHCA, an effect that was not observed in the COACT, PEARL, and TOMAHAWK studies.
Should common practice and guidelines be changed?
The study had several limitations:
- It was an observational registry,
- There was an inherent risk for selection bias. In particular, because of a lack of high-level evidence for benefit for immediate CAG, patients were selected for this approach at the admitting interventional cardiologist’s discretion,
- The registry recruited patients with a primary cardiac etiology OHCA, which is reflected in the high rates of an initial shockable rhythm, so the findings may not be generalizable to all patients with OHCA.
Finally, the authors suggest that the findings should be viewed only as hypothesis-generating and suggest they require detailed validation in larger prospective studies and RCTs before incorporation into clinical practice.
They concluded that Combined classification of patients with OHCA with STEMI, a MIRACLE2 score of 0 to 3, and an SCAI grade of B to E identifies a potential cohort at low risk for neurologic injury that benefits most from immediate CAG.
What is your approach regarding CAG in patients with OHCA?





No comments yet!