Timing and predictors of definite stent thrombosis in comatose survivors of out-of-hospital cardiac arrest undergoing percutaneous coronary intervention and therapeutic hypothermia (ST-OHCA study)
Selected in EuroIntervention by N. Ryan
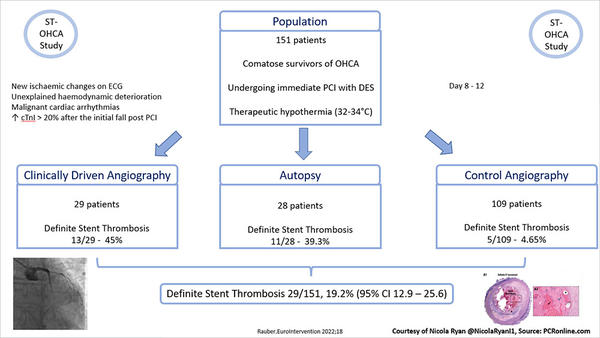
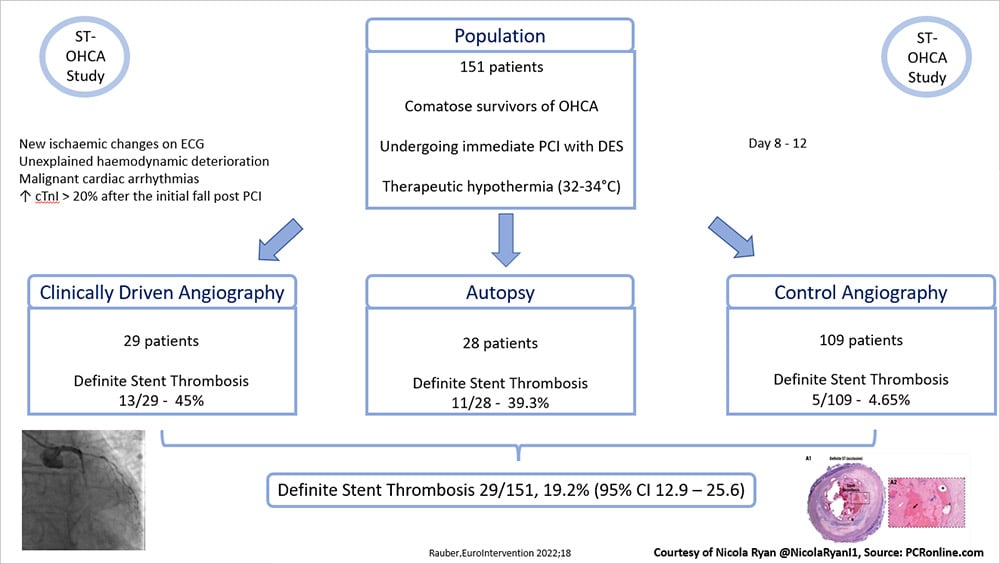
The ST-OHCA study is a single centre prospective study investigating the incidence, timing and predictors of definite stent thrombosis in comatose survivors of out-of-hospital cardiac arrest (OHCA) undergoing immediate PCI and therapeutic hypothermia.
References
Authors
Martin Rauber; Philipp Nicol; Emina Sabic; Michael Joner; Marko Noc
Reference
https://pubmed.ncbi.nlm.nih.gov/35876187/. Online ahead of print.
Published
25 July 2022
Link
Read the abstract
Reviewer
Latest contributions
Balloon lithotripsy added to conventional preparation before stent implantation in severely calcified coronary lesions Impact of pullback pressure gradient on clinical outcomes after percutaneous coronary interventions Validation of intravascular ultrasound-defined optimal stent expansion criteria for favorable 1-year clinical outcomesMy Comment
Why this study – the rationale/objective?
Stent thrombosis (ST) is a serious complication of PCI, however, in patients undergoing PCI for acute coronary syndrome or stable coronary artery disease the incidence of ST is generally low at <1%. Increasingly, comatose survivors of OHCA with a presumed cardiac aetiology, are undergoing immediate PCI. To date the reported incidence of ST in this population varies significantly, with all studies retrospective in nature. This study aimed to investigate the incidence, timing and predictors of definite stent thrombosis in comatose survivors of OHCA undergoing immediate PCI and therapeutic hypothermia (32-34°C).
Analysis of the ST-OHCA study - courtesy of Nicola Ryan
How was it executed? - the methodology
Consecutive comatose patients presenting with an OHCA with a presumed cardiac aetiology undergoing immediate angiography, PCI and therapeutic hypothermia were enrolled in the study. Patients were treated with UFH and 250-500mg IV bolus of acetylsalicylic acid prior to angiography. Cangrelor and eptifibatide were used at the discretion of the treating physician, with all patients receiving contemporary DES. A loading dose of a crushed or dissolved P2Y12 inhibitor via a naso or orogastric tube was administered post procedure and maintenance IV acetylsalicylic acid and crushed/dissolved P2Y12 inhibitor prescribed. Therapeutic hypothermia was initiated in the catheterisation laboratory or on arrival to the ICU and maintained for 24 hours (target temperature 32-34°C). A 12 lead ECG was obtained every 6 hours and cardiac troponin (cTnI) measured every 6-12 hours.
- Stent thrombosis was suspected with new ischaemic changes on ECG
- Unexplained haemodynamic deterioration
- Malignant cardiac arrhythmias
- If cTnI valves increased by > 20% after the initial fall post PCI
- Immediate coronary angiogram was performed with any features of suspected ST
- Control angiogram was performed between day 8 and 12 in patients without features of suspected ST
- All deceased patients underwent an autopsy.
What is the main result?
Overall, between August 2016 and July 2021, 362 comatose survivors of OHCA presented to the centre of whom 169 underwent immediate PCI. Follow up clinically driven or control angiography was available in 151 participants who comprise the study population. The majority of the population were men (89%) in their 60’s who had experienced a witnessed OHCA (93%) with three quarters receiving by-stander CPR. The majority of patients presented with a shockable rhythm (87%) and three quarters had an STEMI on their post resuscitation ECG.
- Definite stent thrombosis occurred in 19.2% of patients (95% CI 12.9%-25.6%)
- Angiographically confirmed definite stent thrombosis was seen in 13.1% (18/137)
- 29 patients underwent a clinically driven angiogram with definite stent thrombosis confirmed in 13 patients (45%).
- 108 patients underwent a control angiogram with definite stent thrombosis seen in 5 (4.6%).
- Autopsy revealed ST in 39.3% of patients (11/28)
- 62% of stent thrombosis occurred within the first three days post presentation.
- Following logistic regression predictors of ST were longer duration of pre-hospital resuscitation (OR 1.05, 95%CI 1.01-1.09, p=0.018), lower arterial pH (OR 0.002, 95%CI 0-0.51, p=0.027) and increased creatinine (OR 1.02, 95% CI 1.00-1.04, p=0.018) on admission.
- Patients with ST had a significantly lower survival with good neurological recovery than those without (17% vs 60%, p<0.001)
Critical reading and the relevance for clinical practice
The results of this study show that the incidence of stent thrombosis in comatose survivors of OHCA undergoing immediate PCI and therapeutic hypothermia is high at 19.2%. The majority of stent thrombosis occurred early in the hospitalisation with clinical signs of definite stent thrombosis in 80%. Haemodynamic deterioration was seen in 34% and new ECG changes in 17%. Malignant arrhythmias (14%) and a significant rise in cTnI (14%) were also observed. Interestingly, a fifth of patients did not demonstrate any obvious clinical signs of ST with 2 detected at autopsy and 4 on control angiography.
Crushed or dissolved P2Y12 inhibitors were not administered until after PCI with relatively low rates of use of both the IV P2Y12 inhibitor cangrelor (5%) and GP IIb/IIIa inhibitor eptifibatide (9%) potentially leading to delayed platelet inhibition. Platelet inhibition may have also been delayed by the use of hypothermia, both of these factors may lead to platelet aggregation and stent thrombosis. Systematic use of a GP IIb/IIIa inhibitor or IV P2Y12 inhibitor in this population may be beneficial to reduce the risk of ST.
Longer resuscitation and the resultant haemodynamic and metabolic compromise appear to be predictors of ST, whilst these are not be modifiable on admission they should be borne in mind when carrying out PCI and scrupulous attention to detail should be paid to minimise technical factors which may also contribute to the risk of ST. Finally recent trials have suggested that hypothermia may produce a prothrombic environment increasing the risk of ST (1–3) therefore maintenance of normothermia may be more beneficial in this population.
It must be borne in mind that there are a number of limitations to this trial including the fact that it was a single centre study without systematic use of intracoronary imaging. Given that patients with ST had a significantly lower survival with good neurological recovery than those without modification of any potential risks for ST is key. Further research determining the optimal management of comatose survivors of OHCA patients undergoing PCI is required. Undoubtably reduction of the risk of stent thrombosis requires a multi-pronged approach including selection of patients who will benefit most from an immediate invasive strategy, imaging optimal PCI, optimisation of platelet inhibition and consideration to maintenance of normothermia rather than hypothermia.
References
- Noc M, Erlinge D, Neskovic AN, Kafedzic S, Merkely B, Zima E, et al. EuroIntervention. 2017 Aug 4;13(5):e531–9.
- Noc M, Laanmets P, Neskovic A, Petrović M, Stanetic B, Aradi D, et al. A multicentre, prospective, randomised controlled trial to assess the safety and effectiveness of cooling as an adjunctive therapy to percutaneous intervention in patients with acute myocardial infarction: the COOL AMI EU Pivotal Trial [Internet]. EuroIntervention. [cited 2022 Aug 9]. Available from: https://eurointervention.pcronline.com/article/a-multicentre-prospective-randomised-controlled-trial-to-assess-the-safety-and-effectiveness-ofcooling-as-an-adjunctive-therapy-to-percutaneous-intervention-in-patients-with-acute-myocardial-infarction-thecoolamieu-pivotal-trial
- Nichol G, Strickland W, Shavelle D, Maehara A, Ben-Yehuda O, Genereux P, et al. Prospective, multicenter, randomized, controlled pilot trial of peritoneal hypothermia in patients with ST-segment- elevation myocardial infarction. Circ Cardiovasc Interv. 2015 Mar;8(3):e001965.




No comments yet!