03 Nov 2023
Clopidogrel versus aspirin monotherapy beyond 1 year after PCI: STOPDAPT-2 five-year results
Selected in JACC by N. Ryan
The STOPDAPT-2 trial was a multicenter, open-label, adjudicator-blinded, randomised control trial comparing clopidogrel monotherapy after one-month DAPT with aspirin monotherapy following 12-months DAPT in patients undergoing PCI with a everolimus-eluting stent...
References
Authors
Hirotoshi Watanabe, Takeshi Morimoto, Masahiro Natsuaki, Ko Yamamoto, Yuki Obayashi, Ryusuke Nishikawa, Kenji Ando, Koh Ono, Kazushige Kadota, Satoru Suwa, Itsuro Morishima, Ruka Yoshida, Yoshiki Hata, Masaharu Akao, Masahiro Yagi, Nobuhiro Suematsu, Yoshihiro Morino, Takafumi Yokomatsu, Itaru Takamisawa, Toshiyuki Noda, Masayuki Doi, Hideki Okayama, Yuichi Nakamura, Kiyoshi Hibi, Hiroki Sakamoto, Teruo Noguchi, Takeshi Kimura, and on behalf of the STOPDAPT-2 investigators
Reference
J Am Coll Cardiol. Oct 23, 2023. Epublished DOI: 10.1016/j.jacc.2023.10.013
Published
October, 2023
Link
Read the abstractReviewer
Latest contributions
Balloon lithotripsy added to conventional preparation before stent implantation in severely calcified coronary lesions Impact of pullback pressure gradient on clinical outcomes after percutaneous coronary interventions Validation of intravascular ultrasound-defined optimal stent expansion criteria for favorable 1-year clinical outcomesMy Comment
Presented at TCT 2023 and simultaneously published in JACC
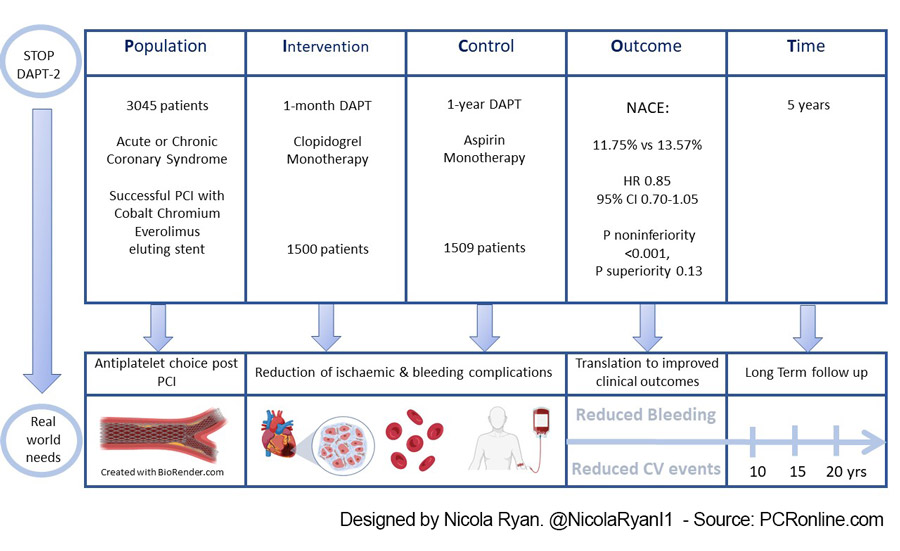
PICOT analysis of STOPDAPT-2 trial at 5 years. Designed by Nicola Ryan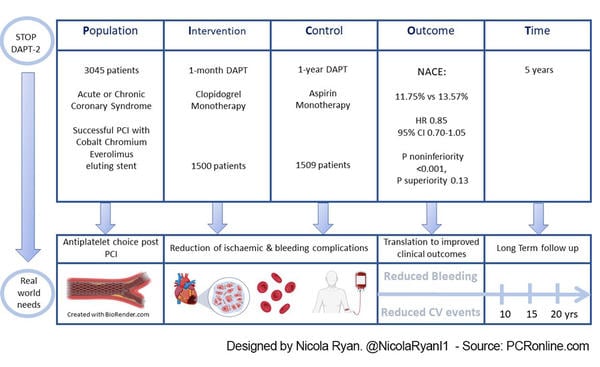
The STOPDAPT-2 trial was a multicenter, open-label, adjudicator-blinded, randomised control trial comparing clopidogrel monotherapy after one-month DAPT with aspirin monotherapy following 12-months DAPT in patients undergoing PCI with an everolimus-eluting stent. At one year clopidogrel monotherapy reduced major bleeding without an increase in ischaemic events compared to DAPT. Here the authors present the five-year follow-up comparing continued clopidogrel monotherapy in the one-month DAPT group with aspirin monotherapy in the one-year DAPT group.
Why this study – the rationale/objective?
Antiplatelet therapy post-PCI aims to reduce ischaemic events however comes with the concomitant increased risk of bleeding. Traditionally, following a period of dual antiplatelet therapy, aspirin monotherapy is prescribed lifelong to reduce the ischaemic risk.
More recent trials (1,2) have suggested that P2Y12 monotherapy may be preferable in terms of reducing bleeding risk without increasing ischaemic risk. Several trials including STOPDAPT-2 demonstrated a reduction in bleeding events without an ischaemic penalty in patients treated with short-duration DAPT followed by P2Y12 monotherapy at one-year (3).
Some studies have suggested a benefit of clopidogrel monotherapy after one year (4) however, aspirin remains the recommended long-term anti-platelet agent in current guidelines (5). Given that antiplatelet therapy is typically prescribed lifelong understanding the optimal anti-platelet strategy after one year is of interest.
How was it executed – the methodology?
Patients having undergone successful PCI with cobalt-chromium everolimus-eluting stents were eligible for inclusion in the study. Patients were randomised 1:1 to one month of DAPT followed by clopidogrel monotherapy or 12 months of DAPT. At 12 months patients in the clopidogrel monotherapy group were to continue clopidogrel and those in the one-year DAPT group were to continue aspirin monotherapy.
- The primary endpoint was net adverse clinical events (NACE); a composite of cardiovascular outcomes (cardiovascular death, myocardial infarction, stroke or definite stent thrombosis) and TIMI major or minor bleeding.
- Secondary endpoints were the major cardiovascular and bleeding components of the primary endpoint.
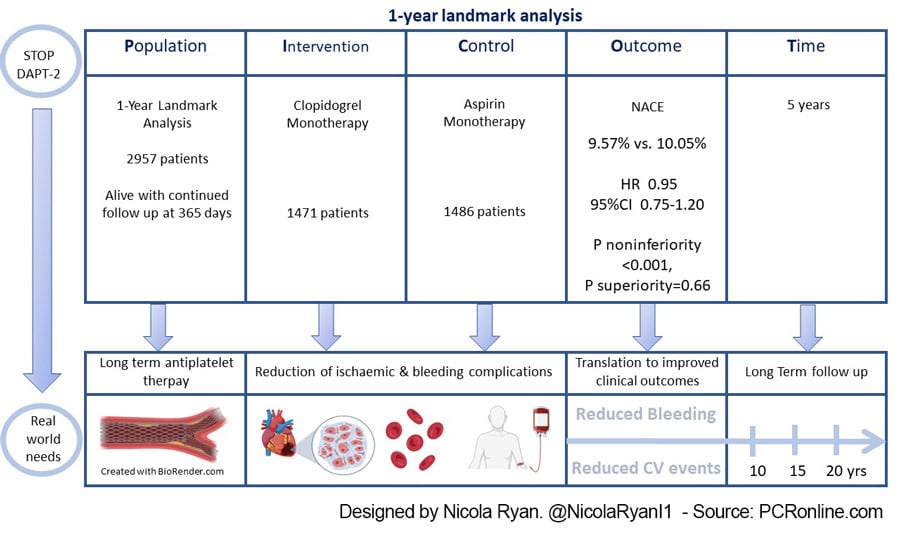
- A 1-year landmark analysis was carried out to compare the effects of long-term clopidogrel and aspirin monotherapy.
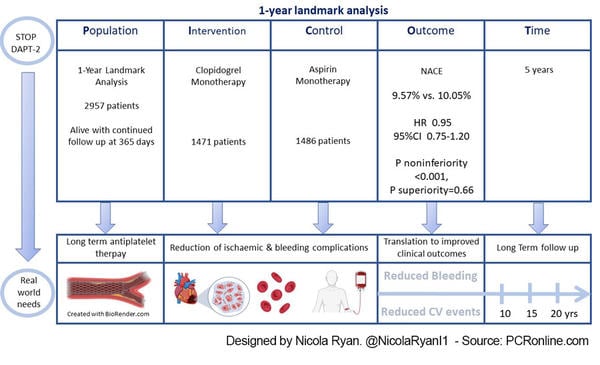
STOPDAPT-2 trial at 5 years / 1-year landmark analysis. Designed by Nicola Ryan
What is the main result?
Recruitment occurred between December 2015 and December 2017 in Japan. Overall, 3045 patients were randomised; 1500 were assigned to 1-month DAPT (long-term clopidogrel monotherapy) and 1509 assigned to 1-year DAPT (long-term aspirin monotherapy). At 5 years 40 patients had withdrawn consent and 3005 were included in the intention to treat (ITT) analysis: 1498 in the clopidogrel group and 1507 in the aspirin group. The majority of patients were men in their 60’s with typical CVRF, 60% of the population presented with chronic coronary syndrome. The use of intracoronary imaging was high within the trial with IVUS used in 85% of cases and a radial approach in 80%, the target lesion was the LAD in 60% of cases with the majority of patients having ≤2 target vessels treated. The landmark analysis included those patients alive and continued follow-up at 365 days (1471 in the clopidogrel group and 1486 in the aspirin group).
- Clopidogrel monotherapy was non-inferior but not superior to Aspirin monotherapy for the primary endpoint of NACE at 5 years ( 11.75% vs 13.57%, HR 0.85, 95% CI 0.70-1.05, P noninferiority <0.001, P superiority 0.13)
- Clopidogrel was superior to aspirin for major cardiovascular endpoint (8.61% vs. 11.05%, HR 0.77, 95%CI 0.61-0.97, P noninferiority <0.001, P Superiority 0.03)
- There was no difference in bleeding between the two groups at 5-years (4.44% vs. 4.92%, HR 0.89, 95%CI 0.64-1.25, p=0.51)
- In the landmark analysis
- Clopidogrel monotherapy was non-inferior, but not superior to aspirin monotherapy for the primary endpoint of NACE (9.57% vs. 10.05%; HR 0.95, 95%CI 0.75-1.20, P noninferiority <0.001, P superiority=0.66)
- There was no difference in the major cardiovascular endpoint (6.79% vs. 8.68%; HR 0.77, 95%CI 0.59-1.0], P=0.06)
- Bleeding rates were similar between treatment arms (3.99% vs. 3.32%; HR 1.23, 95%CI 0.83-1.81, P=0.31)
Critical reading and the relevance for clinical practice
The results of this study show that at 5 years clopidogrel monotherapy after one month of DAPT was non-inferior but not superior to aspirin monotherapy following one year of DAPT in terms of NACE. Clopidogrel remained superior in terms of major cardiovascular events mainly driven by reduced MI with no differences in bleeding events between the groups. Beyond one-year the landmark analysis included only patients who had survived to 365 days and continued follow-up, i.e. a comparison between clopidogrel versus aspirin monotherapy beyond 1-year post-PCI showed that clopidogrel was non-inferior but not superior to aspirin at 5-years in terms of NACE with no differences in the major cardiovascular or bleeding endpoints.
This trial is at odds with the recent HOST-EXAM extended study (4) where the benefit of clopidogrel monotherapy persisted at a median of 5.8 years follow-up. Overall compliance to assigned treatment was approximately 80% at 5 years, in a sensitivity analysis including only patients compliant to assigned therapy there appeared to be a trend towards benefit with clopidogrel; excluding patients with an event at one-year HR 0..72 955 CI 0.51-0.99, p=0.047, including patients with an event at one-year HR 0.68, 95% CI 0..49-0.93, p=0.01.
As with any analysis, there are a number of limitations which must be borne in mind most importantly the randomisation to anti-platelet therapy occurred immediately post PCI with no risk stratification for patients who had events in the initial period. Furthermore, bleeding or ischaemic events in the follow-up period often lead to a change in anti-platelet strategy. Current guidelines recommend continual assessment and re-assessment of bleeding and ischaemic risk when prescribing and continuing anti-platelet therapy. The study was carried out in exclusively Japanese centres with rates of intravascular imaging use that are not typically seen in European countries, therefore the results may not be generalisable. Finally, the majority of patients enrolled in this study were low or intermediate bleeding risk therefore must be interpreted in this context.
This study adds to the data with regard to long-term anti-platelet strategy in the non-high bleeding risk population. To date, the optimal long-term antiplatelet strategy in all populations remains undetermined and clinicians must carefully assess individual patients bleeding and ischaemic risks when prescribing and reviewing antiplatelet therapy.
References
- Koo BK, Kang J, Park KW, Rhee TM, Yang HM, Won KB, et al. Aspirin versus clopidogrel for chronic maintenance monotherapy after percutaneous coronary intervention (HOST-EXAM): an investigator-initiated, prospective, randomised, open-label, multicentre trial. Lancet. 2021 May 14;
- Baber U, Dangas G, Angiolillo DJ, Cohen DJ, Sharma SK, Nicolas J, et al. Ticagrelor alone vs. ticagrelor plus aspirin following percutaneous coronary intervention in patients with non-ST-segment elevation acute coronary syndromes: TWILIGHT-ACS. Eur Heart J. 2020 Oct 1;41(37):3533–45.
- Watanabe H, Domei T, Morimoto T, Natsuaki M, Shiomi H, Toyota T, et al. Effect of 1-Month Dual Antiplatelet Therapy Followed by Clopidogrel vs 12-Month Dual Antiplatelet Therapy on Cardiovascular and Bleeding Events in Patients Receiving PCI: The STOPDAPT-2 Randomized Clinical Trial. JAMA. 2019 Jun 25;321(24):2414.
- Kang J, Park KW, Lee H, Hwang D, Yang HM, Rha SW, et al. Aspirin vs. Clopidogrel for Chronic Maintenance Monotherapy after Percutaneous Coronary Intervention: the HOST-EXAM Extended Study. Circulation [Internet]. 2022 Oct 24 [cited 2022 Nov 8]; Available from: https://www.ahajournals.org/doi/abs/10.1161/CIRCULATIONAHA.122.062770
- Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC Guidelines for the management of acute coronary syndromes: Developed by the task force on the management of acute coronary syndromes of the European Society of Cardiology (ESC). European Heart Journal. 2023 Oct 7;44(38):3720–826.