16 Jun 2023
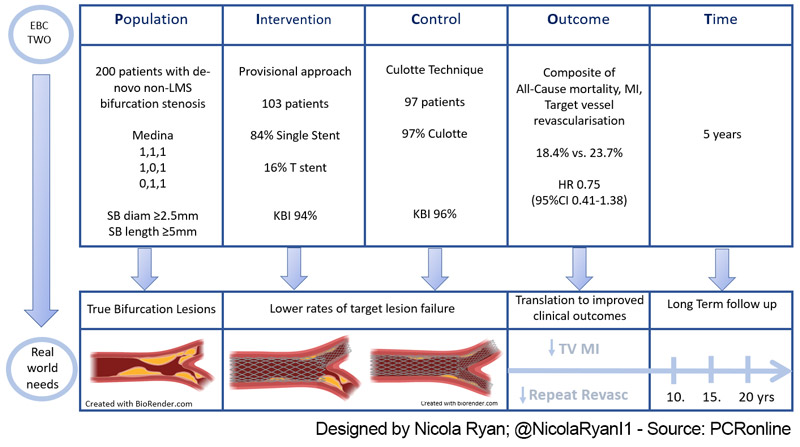
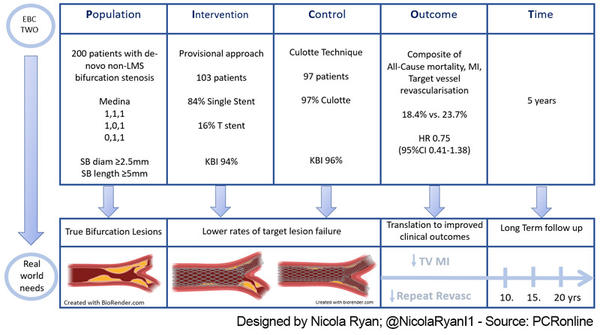
Stepwise provisional versus systematic culotte for stenting of true coronary bifurcation lesions: five-year follow-up of the multicentre randomised EBC TWO Trial
Selected in EuroIntervention Journal by N. Ryan
The investigator initiated, multicentre, randomised, EBC TWO trial compared a provisional strategy with a systematic culotte technique in patients with true non-LMS bifurcation disease. At one year, there was no difference between the groups in terms of the composite endpoint of all-cause mortality, MI or TVR. Here, the authors report the extended follow-up through five years.
References
Authors
Sandeep Arunothayaraj, Miles Behan, Thierry Lefèvre, Jens Flensted Lassen, Alaide Chieffo, Goran Stankovic, Francesco Burzotta, Manuel Pan, Miroslaw Ferenc, Thomas Hovasse, Mark Spence, Philippe Brunel, James Cotton, James Cockburn, Didier Carrié, Andreas Baumbach, Michael Maeng, Yves Louvard, David Hildick-Smith
Reference
10.4244/EIJ-D-23-00211 - DOI: 10.4244/EIJ-D-23-00211
Published
May 16, 2023
Link
Read the abstract
Reviewer
My Comment
Designed by Nicola Ryan
Why this study – the rationale/objective?
The optimal treatment for true non-LM bifurcation disease remains a topic of debate. The DKCRUSH-II1 trial showed a trend towards reduced MACE at 5 years with a DK-Crush technique, however this was mainly driven by TVR which clustered around the time of compulsory angiography follow-up.
Furthermore, concerns exist with regard to trials using first generation stents or those in which the side branches (SB) were small and unlikely to be of functional significance. Therefore, the EBC-TWO trial included exclusively bifurcations with disease in both branches with a SB diameter ≥ 2.5 mm and length ≥ 5 mm, with no difference in composite endpoint of all-cause mortality, MI or TVR at one year. The longer term outcomes of such strategy is of interest, therefore the authors report the extended follow-up to five years.
How was it executed - the methodology?
From April 2011 to January 2014, patients requiring PCI for true bifurcation disease (main vessel (MV) & SB > 50 stenosis with both MV & SB reference diameter ≥ 2.5 mm and SB ostial disease ≥ 5mm in length were eligible for inclusion. Follow-up was continued to five years in-person or telephonically. There was no routine angiographic follow-up.
- The primary endpoint was the composite of all cause death, MI and target vessel revascularisation (TVR) at five years.
- The secondary endpoints were the components of the primary endpoints and stent thrombosis.
What is the main result?
Overall, 200 patients from 6 European countries were enrolled in the trial. 103 were randomised to provisional approach, with 16 % undergoing a provisional-T, and 97 randomised to the systematic culotte group. The majority of bifurcations involved the LAD (78 %), with a mean SB length of 10 mm, and approximately a third of patients presented with ACS.
- The primary endpoint occurred in 18.4 % of the Provisional group, compared to 23.7 % of the Culotte group (HR 0.75, 95 % CI 0.41-1.38, p = 0.36)
- There was no difference in all cause (7.8 % vs 7.2 %, HR 1.11, 95 % CI 0.40 = 3.05, p = 0.85) or cardiac (2.9 % vs 3.1 %, HR 0.93, 95 % CI 0.19-4.59, p = 0.92) mortality between groups
- MI (8.7 % vs 13.4 %, HR 0.64, 95 % CI 0.27-1.5, p = 0.30), TVR (6.8 % vs 9.3 % HR 1.12, 95 % CI 0.37-3.34, p = 0.84) and stent thrombosis (1.9 % vs 3.1 %, HR 0.63, HR 0.11 = 3.75, p = 0.61) were similar between groups.
Critical reading and the relevance for clinical practice:
The long-term follow-up of investigator initiated multicentre randomised EBC TWO showed that there were no significant differences between a provisional strategy and a systematic culotte in terms of MACE, composite endpoint of all-cause mortality, myocardial infarction, or target vessel revascularisation at five years.
Overall, MACE was 21 % with low rates of bifurcation-related adverse events (6.5 %), a composite of acute vessel closure, stent thrombosis, target lesion MI, and target lesion revascularisation, with no significant differences between strategies (5.8 % provisional vs. 7.2 % culotte, HR 0.80, 95 % CI0.27-2.39 p = 0.69). There was no significant interaction between SB length (≥ 10 mm), and the primary endpoint (p for interaction 0.34). Importantly, when SB stenting was required in the provisional strategy group, there was no significant difference in MACE compared to those with MV stenting alone (12.5 % vs 19.5 %, HR 0.72, 95 % CI 0.17-3.09).
The EBC TWO trial enrolled patients with significant SB disease (mean length 10 mm diameter ≥ 2.5 mm), with a high proportion of patients presenting with acute coronary syndrome and LAD disease, therefore representative of patients who potentially were more likely to benefit from a two-stent strategy.
Of note, there is a number of limitations inherent to the time of enrolment in the trial, notably the modifications in the Culotte technique to a DK Culotte which in bench testing has advantages over traditional Culotte2.
Futhermore, the use of intracoronary imaging, which may improve outcomes in bifurcation PCI3, was neither mandated nor recorded in the trial.
Finally, the second anti-platelet agent was clopidogrel, more potent P2Y12 inhibitors may improve clinical outcomes, though rates of stent thrombosis were low overall.
To date, all data supporting a two-stent technique in non-LM bifurcations above a provisional approach has been driven by DK-CRUSH II, with the inherent limitation of control angiography at 8 months. Given the clustering of TVR around the control angiogram, it is more difficult to translate this real-world practice where TVR is typically ischaemia driven.
Given the long-term results from this trial, a step-wise provisional approach appears to be the most favourable option when treating non-LM bifurcation lesions. This stepwise approach allows assessment of lesion at each stage of the intervention with conversion to a two-stent technique if required without significant jeopardy.
To go further...
Fresh from the #EuroPCR 2023 session presenting the Late-Breaking clinical EBC TWO Trial , we asked Mirvat Alasnag and Sandeep Arunothayaraj to summarize the key takeaways from the five-year results of this multicenter randomised study comparing stepwise provisional versus systematic culotte for stenting of true coronary bifurcation lesions.
References
- Crush Versus Provisional Stenting of Coronary Artery Bifurcation Lesions: The 5-Year Follow-Up Results From a Randomized and Multicenter DKCRUSH-II Study (Randomized Study on Double Kissing Crush Technique Versus Provisional Stenting Technique for Coronary Artery Bifurcation Lesions). Circ Cardiovasc Interv. 2017 Feb;10(2):e004497.
- Toth G, Sasi V, Franco D, Prassl A, Diserafino L, Ng J, et al. Double-kissing culotte technique for coronary bifurcation stenting [Internet]. EuroIntervention. [cited 2023 May 31]. Available from: https://eurointervention.pcronline.com/article/double-kissing-culotte-technique-for-coronary-bifurcation-stenting-technical-evaluation-and-comparison-with-conventional-double-stenting-techniques
- Kim JS, Hong MK, Ko YG, Choi D, Yoon JH, Choi SH, et al. Impact of intravascular ultrasound guidance on long-term clinical outcomes in patients treated with drug-eluting stent for bifurcation lesions: Data from a Korean multicenter bifurcation registry. American Heart Journal. 2011 Jan;161(1):180–7.