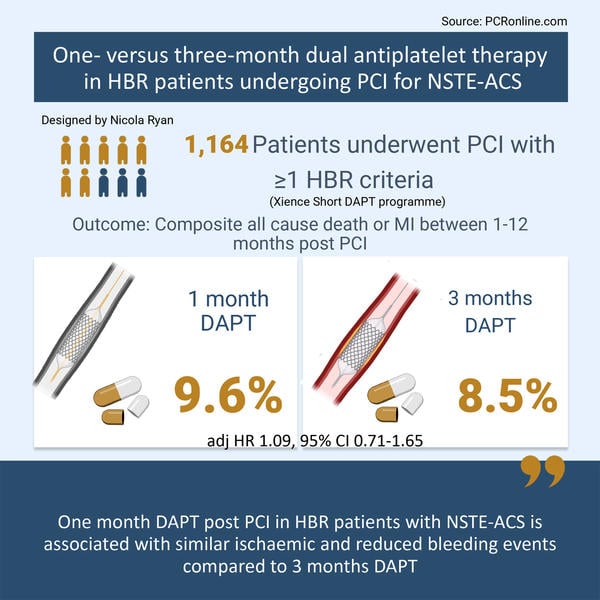
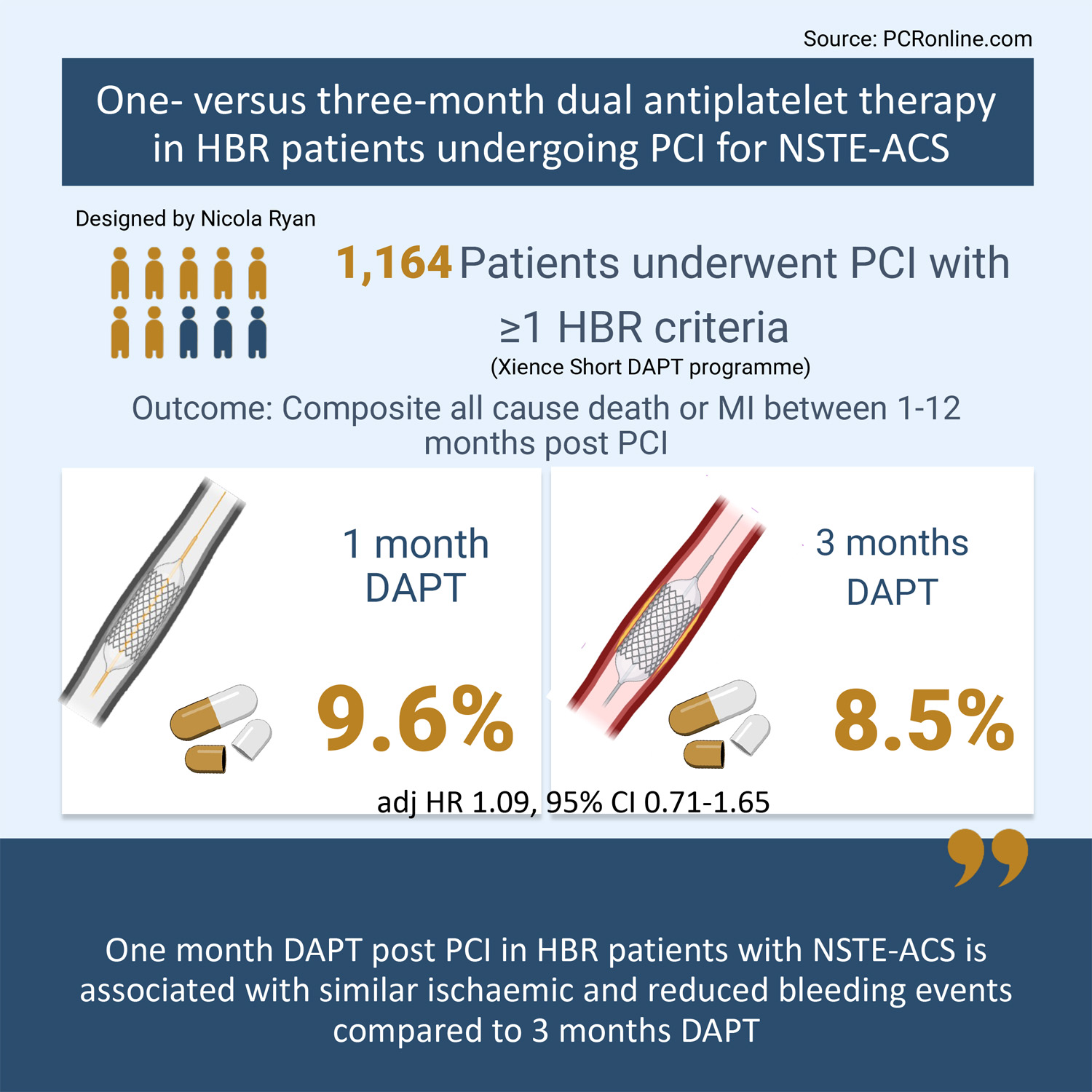
One- versus three-month dual antiplatelet therapy in high bleeding risk patients undergoing percutaneous coronary intervention for non-ST-segment elevation acute coronary syndromes
Selected in EuroIntervention Journal by N. Ryan
The optimal duration of short DAPT in ACS patients is unknown, therefore this analysis of the XIENCE Short DAPT programme compared the clinical outcomes of one versus three months DAPT in HBR patients with and without ACS.
References
Authors
Davide Cao; Pascal Vranck; Marco Valgimigli; Samantha Sartori; Dominick J. Angiolillo; Sripal Bangalore; Deepak L. Bhatt; Yihan Feng; Junbo Ge; James Hermiller; Raj R. Makkar; Franz-Josef Neumann; Shigeru Saito; Hector Picon; Ralph Toelg; Aziz Maksoud; Bassem M. Chehab; James W. Choi; Gianluca Campo; José M. De la Torre Hernandez; Mitchell W. Krucoff; Vijay Kunadian; Gennaro Sardella; Alessandro Spirito; Holger Thiele; Olivier Varenne; Birgit Vogel; Yujie Zhou; Stephan Windecker; Roxana Mehran
Reference
DOI: 10.4244/EIJ-D-23-00658 • MAY 20, 2024
Published
20 May 2024
Link
Read the abstractReviewer
Latest contributions
Balloon lithotripsy added to conventional preparation before stent implantation in severely calcified coronary lesions Impact of pullback pressure gradient on clinical outcomes after percutaneous coronary interventions Validation of intravascular ultrasound-defined optimal stent expansion criteria for favorable 1-year clinical outcomesMy Comment
This prespecified analysis from the Xience Short DAPT programme compared the safety and efficacy of one month versus three month DAPT in high bleeding risk patients with and without NSTE-ACS, following PCI with everolimus eluting stents.
The Xience Short DAPT programme.
Courtesy of Nicola Ryan. Source: PCRonline.com
Why this study – the rationale/objective?
Dual antiplatelet therapy aims to reduce ischaemic risk after ACS and PCI, but comes with a concomitant increased risk of bleeding.
Patients with prior MI have an increased risk of ischaemic events in the longer term, therefore there has been significant interest in the optimal DAPT duration to reduce the risk of recurrent ischaemic events.
The current guidelines recommend discontinuation of dual anti-platelet therapy in most patients at one year, with consideration to early discontinuation in patients at high bleeding risk1.
Prior studies have established that PCI with DES and one month of DAPT is a safe and efficacious strategy in all-comer high bleeding risk patients2, with several studies showing abbreviated DAPT to be safe in the ACS population3–6.
The optimal duration of short DAPT in ACS patients is unknown, therefore this analysis of the XIENCE Short DAPT programme compared the clinical outcomes of one versus three months DAPT in HBR patients with and without ACS.
How was it executed – the methodology?
The Xience Short DAPT programme includes three prospective multicentre registries; Xience 90 (3 months DAPT), Xience 28 USA and Xience 28 Global (1 month DAPT) enrolling patients undergoing PCI with fluoropolymer-based cobalt-chromium everolimus eluting stents for acute or chronic coronary syndrome with at least one high bleeding risk criteria from July 2017 to February 2020.
Patients were treated with aspirin and a P2Y12 inhibitor, preferentially clopidogrel, patients were assessed at one month and three months respectively (Xience 28 and Xience 90) to ensure they remained eligible for DAPT discontinuation (no adverse events and compliant with therapy). This analysis included the Xience 28 populations with patients who were event free at one month in the Xience 90 population selected to match the Xience 28 population.
- The primary outcome was a composite of all cause death or MI between 1 and 12 months post index PCI
- The key secondary endpoint was BARC Type 2 to 5 bleeding
- Other secondary endpoints included target lesion failure (a composite of cardiovascular death, target vessel MI or target lesion revascularisation), the individual components of the composite endpoints, stroke, definite or probable stent thrombosis and BARC Type 3 to 5 bleeding.
The effects of one versus three months DAPT on outcomes was evaluation according to clinical presentation (NSTE-ACS versus chronic coronary syndrome) at the time of PCI.
What is the main result?
Of the 3,364 eligible patients, 1,164 underwent PCI for ACS (475 and 689 received one and three months DAPT respectively) and 2,200 for CCS (917 and 1,283 received one and three months DAPT respectively). Age greater than 75 years and requirement for oral anticoagulants were the most common HBR criteria, with a mean of 1.5 HBR criteria per patient. A third of the population were female, with higher PRECISE-DAPT and PARIS bleeding scores in the NSTE-ACS population.
- There was numerically higher rates of the primary endpoint in the NSTE-ACS group compared to the chronic coronary syndrome group (9.0 % vs. 7.4 % p = 0.074), mainly driven by an increased risk of MI at one year (5.3 % vs 2.8 %, p < 0.001)
- In the NSTE-ACS population the primary endpoint occurred in 9.6 % vs. 8.5 % of the one month and three months DAPT groups respectively (adj HR 1.09, 95 % CI 0.71-1.65).
- The incidence of BARC Type 2-5 bleeding was similar in the NSTE-ACS and CCS populations (10.1 % vs. 8.9 %, p = 0.213)
- In the NSTE-ACS population there was a significant reduction in BARC Type 2-5 bleeding in the one month DAPT population (7.3 % vs. 12.2 %, adj HR 0.57, 95 % CI 0.37-0.88).
- Rates of all cause death (adj HR 0.85, 95 % CI 0.41-1.37), MI (adj HR 1.13, 95 % CI 0.65-1.96), stroke (adj HR 0.39, 95 % CI 0.12-1.27 and TLF (adj HR 0.99, 95 % CI 0.61-1.59) were similar in the ACS population between 1 and 3 month DAPT groups.
- There was no difference in BARC type 3-5 bleeding between 1 and 3 months DAPT in the ACS population (adj HR 0.66, 95 %CI 0.36-1.19).
- Consistent treatment effects were seen in the CCS population across primary and secondary endpoints with no significant interaction between clinical presentation and DAPT duration.
Critical reading and the relevance for clinical practice
The results of this study show that discontinuation of DAPT one month in HBR patients who are event free post PCI with a cobalt-chromium everloimus-eluting stent is associated with a similar ischaemic risk and lower bleeding risk compared to discontinuation of DAPT at three months irrespective of clinical presentation. The NSTE-ACS population had an increased risk of ischaemic events compared to the CCS population, however there were no significant differences in ischaemic events between the one and three month DAPT groups.
Previous subgroup analysis of the MASTER DAPT trial where HBR patients who underwent PCI with biodegradable polymer sirolomus eluting stents were randomised to one month or three months DAPT did not demonstrate any difference in ischaemic risk but reduced bleeding risk with one month DAPT in patients with recent MI7. Different to the current analysis three quarters of patients in the MASTER DAPT trial continued with P2Y12 monotherapy as apposed to aspirin monotherapy.
In the Xience Short DAPT programme, study protocol mandated withdrawal of the P2Y12 inhibitor and continuation with aspirin monotherapy. In an exploratory landmark analysis between one and three months post PCI, there was a numerical increase in the risk of death or MI in the NSTE-ACS group with one versus three months DAPT (adj HR 20.5, 95 % CI 0.74-5.66) driven mainly by increased risk of MI (p interaction = 0.040). This was not seen in the analysis between 3-12 months. Whilst it is not possible to draw definitive conclusions with regard to the influence, this may have had on the exploratory landmark analysis, more recent evidence suggests that withdrawal of aspirin and continuation of P2Y12 monotherapy may be a preferable strategy in patients with both ischaemic and bleeding risks.
This analysis is of interest to the community as high bleeding risk patients are frequently encountered in clinical practice with increasing life expectancy as well as increased complexity of patients undergoing PCI, particularly in the ACS setting. Whilst the increased ischaemic events in the ACS population need to be carefully considered when abbreviating DAPT, extending DAPT to three months compared to one month does not confer an ischaemic benefit, but is associated with increased bleeding events. Importantly, BARC Type 3-5 bleeding events were similar between one and three month DAPT, however BARC Type 2 bleeding is relevant for both patients and healthcare resources.
One month DAPT appears a reasonable strategy in a population similar to that enrolled in the Xience Short DAPT programme. Of note, this study only includes patients who were event free and compliant with medications at one month review, therefore this is a strategy that can only be applied following clinical review at one month. The optimal antiplatelet agent for monotherapy remains an important topic for investigation, with more recent evidence suggesting that P2Y12 monotherapy may be preferable.
It must be borne in mind that there is a number of limitations to this trial including the fact that patients with STEMI and complex coronary lesions were excluded. Despite propensity matching there may be residual confounding as this prespecified analysis was not randomised.
Whilst this analysis was not designed to support one-month of DAPT in all-comers it increases the evidence supporting one month of DAPT in HBR patients including those with ACS. As always, decisions with regard to ischaemic and bleeding risk, along with choice of antiplatelet agent need to be carefully assessed and individualised to each patient
References
- Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC Guidelines for the management of acute coronary syndromes: Developed by the task force on the management of acute coronary syndromes of the European Society of Cardiology (ESC). European Heart Journal. 2023 Oct 7;44(38):3720–826.
- Urban P, Meredith IT, Abizaid A, Pocock SJ, Carrié D, Naber C, et al. Polymer-free Drug-Coated Coronary Stents in Patients at High Bleeding Risk. N Engl J Med. 2015 Nov 19;373(21):2038–47.
- Baber U, Dangas G, Angiolillo DJ, Cohen DJ, Sharma SK, Nicolas J, et al. Ticagrelor alone vs. ticagrelor plus aspirin following percutaneous coronary intervention in patients with non-ST-segment elevation acute coronary syndromes: TWILIGHT-ACS. Eur Heart J. 2020 Oct 1;41(37):3533–45.
- Valgimigli Marco, Frigoli Enrico, Heg Dik, Tijssen Jan, Jüni Peter, Vranckx Pascal, et al. Dual Antiplatelet Therapy after PCI in Patients at High Bleeding Risk. New England Journal of Medicine. 2021 Oct 27;385(18):1643–55.
- Kim BK, Hong SJ, Cho YH, Yun KH, Kim YH, Suh Y, et al. Effect of Ticagrelor Monotherapy vs Ticagrelor With Aspirin on Major Bleeding and Cardiovascular Events in Patients With Acute Coronary Syndrome: The TICO Randomized Clinical Trial. JAMA. 2020 Jun 16;323(23):2407–16.
- Watanabe H, Domei T, Morimoto T, Natsuaki M, Shiomi H, Toyota T, et al. Effect of 1-Month Dual Antiplatelet Therapy Followed by Clopidogrel vs 12-Month Dual Antiplatelet Therapy on Cardiovascular and Bleeding Events in Patients Receiving PCI: The STOPDAPT-2 Randomized Clinical Trial. JAMA. 2019 Jun 25;321(24):2414.
- Smits PC, Frigoli E, Vranckx P, Ozaki Y, Morice MC, Chevalier B, et al. Abbreviated Antiplatelet Therapy After Coronary Stenting in Patients With Myocardial Infarction at High Bleeding Risk. Journal of the American College of Cardiology. 2022 Sep 27;80(13):1220–37.




No comments yet!