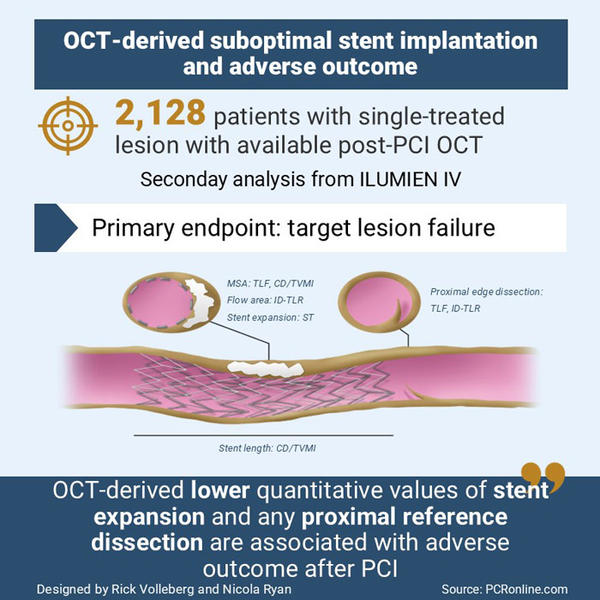
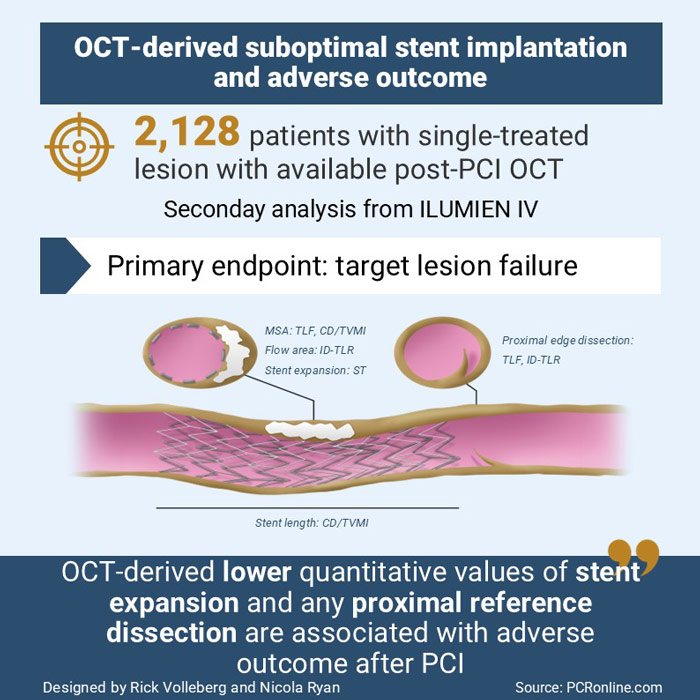
Optical coherence tomography predictors of clinical outcomes after stent implantation: the ILUMIEN IV trial
Selected in European Heart Journal by R. Volleberg , N. Ryan
The aim of this pre-specified analysis of the ILUMIEN IV trial was to assess the relationship between post-PCI OCT parameters of suboptimal stent implantation and clinical outcomes.
References
Authors
Ulf Landmesser, Ziad A Ali, Akiko Maehara, Mitsuaki Matsumura, Richard A Shlofmitz, Giulio Guagliumi, Matthew J Price, Jonathan M Hill, Takashi Akasaka, Francesco Prati, Hiram G Bezerra, William Wijns, David Leistner, Paolo Canova, Fernando Alfonso, Franco Fabbiocchi, Giuseppe Calligaris, Rohit M Oemrawsingh, Stephan Achenbach, Carlo Trani, Balbir Singh, Robert J McGreevy, Robert W McNutt, Shih-Wa Ying, Jana Buccola, Gregg W Stone
Reference
European Heart Journal, ehae521, https://doi.org/10.1093/eurheartj/ehae521
Published
28 August 2024
Link
Read the abstractReviewers
Our Comment
Summary of the ILUMIEN IV trial
Designed by Rick Volleberg and Nicola Ryan. Source: PCRonline.com
Why this study – the rationale/objective?
Optical coherence tomography (OCT) allows accurate assessment of stent implantation. The association between suboptimal PCI results, including expansion, edge dissection, malapposition, thrombus and clinical outcome, remains uncertain.
The aim of this pre-specified analysis of the ILUMIEN IV trial was to assess the relationship between post-PCI OCT parameters of suboptimal stent implantation and clinical outcomes.
How was it executed – the methodology?
The ILUMIEN IV trial compared OCT-guided PCI to angiography guidance in high-risk patients or complex lesions.
All patients, irrespective of group allocation, had a final OCT run with operators blinded to this run in the angiography group.
In this pre-specified analysis, all patients with a single treated lesion and an evaluable final OCT were included. OCT images were evaluated by an independent core laboratory with regards to 20 candidate features of suboptimal stent implantation.
- The primary clinical endpoint was target lesion failure (TLF), a composite of cardiac death, TV-MI or ID-TLR at 2-year follow-up.
- Secondary endpoints were the composite of cardiac death or TV-MI, ID-TLR and definite or probable stent thrombosis.
What is the main result?
Of the 2,487 patients enrolled in ILUMIEN IV, 2,128 (85.6 %), 1,056 in the OCT arm and 1,072 in the angiography arm, had a single treated lesion with an evaluable final OCT run and were included in this analysis.
Slightly more than a third of patients had diabetes, and long lesions were the most common high-risk lesion characteristics, just under a third of lesions were severely calcified.
The 2-year rates of TLF (6.3 %), cardiac death or TV-MI (3.3 %), ID-TLR (4.3 %) and stent thrombosis (0.9 %) were similar in this cohort to the overall study population, with no differences between the OCT and angiography groups.
At multivariable analyses:
- Predictors of TLF were:
- Minimum stent area, per 1 mm2 (HR 0.76, 95 % CI 0.68-0.86, p < 0.001)
- Any proximal edge dissection (HR 1.77, 95 % CI 1.20-2.62, p = 0.004)
- Predictors of cardiac death or target-vessel myocardial infarction were:
- Minimum stent area, per 1 mm2 (HR 0.82, 95 % CI 0.70-0.95, p = 0.009)
- Stent length, per 5 mm (HR 1.08, 95 % CI 1.02-1.15, p = 0.009)
- Predictors of ischemia driven target lesion revascularisation
- Intra-stent flow area, per 1 mm2 (HR 0.72, 95 % CI 0.62-0.84, p < 0.001)
- Proximal edge dissection (HR 1.88, 95 % CI 1.16-3.03, p = 0.01)
- Predictors of stent thrombosis
- Minimum stent expansion, per 10 % (HR 0.71, 95 % CI 0.55-0.93, p = 0.01)
Critical reading and the relevance for clinical practice
Increasing evidence supports the use of intravascular imaging for guidance of coronary lesion revascularisation, especially for complex lesions1, which led to a recent upgrade in guideline recommendation2. However, the criteria for optimal OCT-guided PCI differ between trials, and much of the data comes from observational registries.
In this pre-specified analysis from the ILUMIEN IV trial, the strongest predictors of TLF were minimum stent area and proximal edge dissections. The risk of TLF particularly increased with minimum stent area < 4.0 mm2. Intriguingly, proximal edge dissections were previously believed to not warrant additional treatment, in contrast to distal edge dissections. Acute malapposition was present in a very low percentage of cases and was not associated with poorer clinical outcomes. Finally, although statistical significance was not reached, a trend was observed towards worse clinical outcomes in the presence of residual stent edge disease.
It should be acknowledged that the present analysis includes both patients in the OCT-arm and the angiography-arm of the ILUMIEN IV trial. Considering that post-PCI OCTs were used for periprocedural decision making in the OCT-arm, it is likely that iterative treatments have been undertaken in cases of suboptimal stent implantation. However, the core lab detected suboptimal implantation criteria was higher than operator detected suggesting that there is ongoing room for improvement in education for physicians to recognize these criteria and optimize stent implantation. In the angiography-guided arm, OCT review at the time may have allowed further optimization of the stents.
Given that the ILUMIEN IV trial did not meet its primary objective of demonstrating superiority of OCT guidance over angiography guidance, all sub-analyses need to be interpreted as hypothesis generating within this context.
Overall, the findings of this analysis provide guidance to operators regarding the key post PCI OCT parameters to focus on when evaluating PCI results. In particular, the findings reinforce the consensus that efforts should be made to maximize post-PCI stent expansion with regards to both absolute and relative measures.
References
- Stone GW, Christiansen EH, Ali ZA, Andreasen LN, Maehara A, Ahmad Y, et al. Intravascular imaging-guided coronary drug-eluting stent implantation: an updated network meta-analysis. Lancet. 2024;403(10429):824-37.
- Vrints C, Andreotti F, Koskinas KC, Rossello X, Adamo M, Ainslie J, et al. 2024 ESC Guidelines for the management of chronic coronary syndromes. Eur Heart J. 2024.








No comments yet!