Percutaneous coronary intervention versus coronary artery bypass grafting in patients with left main disease with and without diabetes: findings from a pooled analysis of 4 randomized clinical trials
Selected in Circulation by A. Sticchi , A. Colombo
This analysis shows that diabetic patients undergoing revascularization face substantially higher 5-year rates of all-cause mortality, myocardial infarction, repeat revascularizations, and stroke compared to non-diabetic patients.
References
Authors
Prakriti Gaba, Joseph F. Sabik, Sabina A. Murphy, Andrea Bellavia, Patrick T. O’Gara, Peter K. Smith, Patrick W. Serruys, A. Pieter Kappetein, Seung-Jung Park, Duk-Woo Park, Evald H. Christiansen, Niels R. Holm, Per H. Nielsen, Marc S. Sabatine, Gregg W. Stone and Brian A. Bergmark
Reference
https://doi.org/10.1161/CIRCULATIONAHA.123.065571 | Circulation. 2024;149:1328–1338
Published
March, 11 2024
Link
Read the abstractReviewers
Our Comment
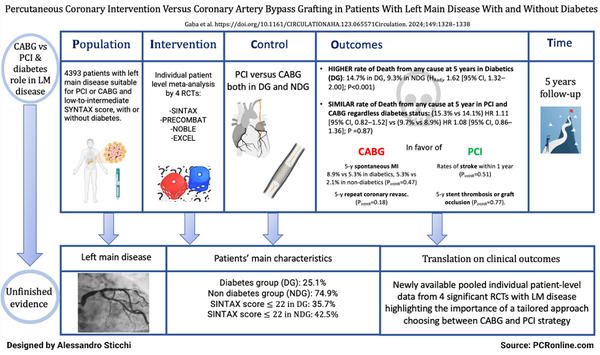
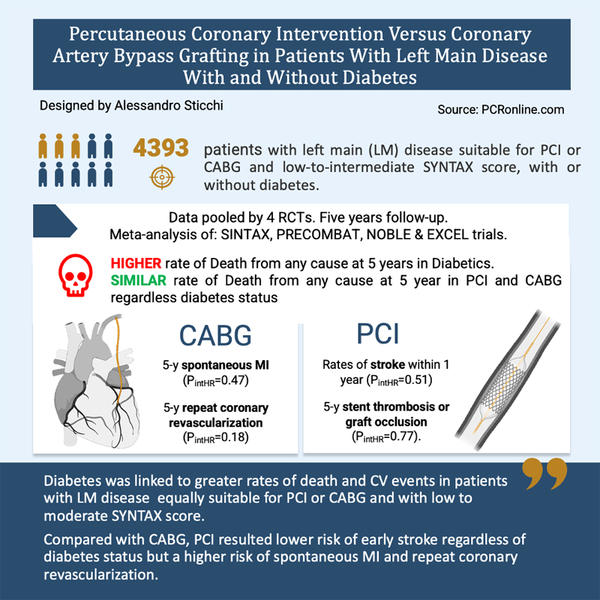
Picot scheme highlighting key aspects of the analysis.
Courtesy of Alessandro Sticchi. Source: PCRonline
Why this study? – the rationale/objective
The study aimed to analyze outcomes in patients with left main coronary artery disease, considering the variations between those with and without diabetes when treated with either percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG).
Historically, decisions between PCI and CABG have been contentious, specifically for patients with diabetes. The study seeks to fill this gap by using a comprehensive pooled analysis to guide more nuanced treatment decisions and optimize patient outcomes in this high-risk population.
How was it executed? - the methodology
The methodology involved a pooled analysis of individual patient data from four pivotal trials — SYNTAX, PRECOMBAT, NOBLE, and EXCEL — which are significant in the domain of coronary revascularization. Patients from these studies, who were diagnosed with left main coronary artery disease and were deemed suitable for either PCI or CABG by clinical teams, were included.
The analysis focused on major cardiovascular outcomes, including all-cause mortality, myocardial infarction, and repeat revascularization over a five-year follow-up period, using Kaplan-Meier curves and Cox proportional hazards models to assess and compare the efficacy and safety of the two treatment modalities across different patient subgroups.
What is the main results?
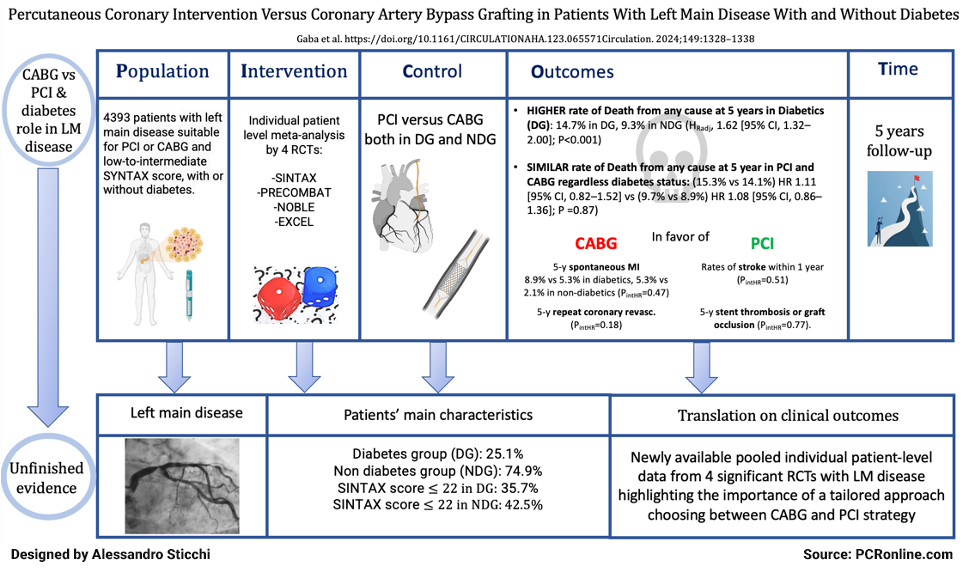
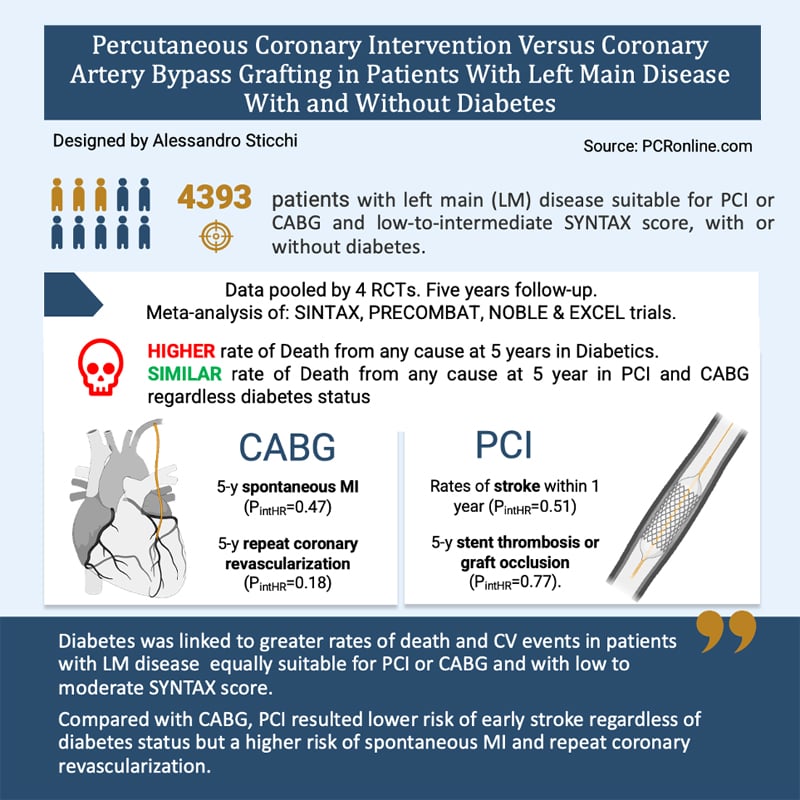
Scheme summarizing the outcomes of the analysis.
Courtesy of Alessandro Sticchi. Source: PCRonline
The study's findings are significant and provide a detailed breakdown of outcomes by treatment type and patient diabetic status.
Among the 4,393 patients analyzed, diabetic patients had notably worse outcomes than their non-diabetic counterparts across several metrics: higher rates of five-year all-cause mortality (14.7 % in diabetics vs. 9.3 % in non-diabetics, P < 0.001), myocardial infarction (6.7 % vs. 3.7 %, P < 0.001), and repeat revascularization (18.5 % vs. 13.2 %, P < 0.001).
Despite these differences, the study showed no significant difference in all-cause mortality between PCI and CABG within diabetic (15.3 % for PCI vs. 14.1 % for CABG; hazard ratio [HR], 1.11 [95 % CI, 0.82–1.52]) and non-diabetic patients (9.7 % for PCI vs. 8.9 % for CABG, HR 1.08 [95 % CI, 0.86–1.36; PintHR = 0.87).
It was highlighted that diabetic patients with higher atherosclerotic burden (as indicated by higher SYNTAX scores) showed better survival rates with CABG compared to PCI.
Within one year of treatment for left main coronary artery disease, patients undergoing PCI had lower rates of stroke compared to those who had CABG, at 0.7 % versus 2.7 % for diabetic patients, and 0.6 % versus 1.3 % for non-diabetic patients, with this benefit consistent regardless of diabetes status (PintHR = 0.51). The rates of stent thrombosis or graft occlusion lower with PCI versus CABG regardless of diabetes status through 5 years (diabetes: 14/563 [2.6 %] versus 29/541 [5.9 %]; HR, 0.46 [95 % CI, 0.24–0.88]; no diabetes: 30/1634 [1.9 %] versus 70/1655 [4.5 %]; HR, 0.42 [95 % CI, 0.27–0.64]; PintHR = 0.77).
However, the five-year rates of spontaneous myocardial infarction (MI) and repeat revascularization were higher in the PCI group, with spontaneous MI occurring in 8.9 % of diabetic patients compared to 4.4 % in the CABG group, and in 5.3 % of non-diabetic patients compared to 2.1 % with CABG.
Similarly, repeat revascularization rates were 24.5 % for diabetic patients with PCI versus 12.4 % with CABG, and 16.3 % versus 10.1 % for non-diabetic patients. The absolute risk differences for both spontaneous MI and repeat revascularization were greater in diabetic patients (4.9 % and 9.9 %, respectively) than in non-diabetics (2.1 % and 4.3 %), particularly beyond the first year (PintHR = 0.047 and 0.016, respectively).
Critical reading and relevance for clinical practice
The impressive individual patient level meta-analysis of Gaba et al. reflects on the study's implications and the ongoing debate between PCI and CABG for treating left main coronary artery disease, particularly in diabetic patients.
It shows that diabetic patients undergoing revascularization face substantially higher 5-year rates of all-cause mortality, myocardial infarction, repeat revascularizations, and stroke compared to non-diabetic patients. Specifically, patients with diabetes show a 5-year all-cause mortality rate of about 14.7 % compared to 9.3 % in non-diabetics, which underscores the severe impact of diabetes on long-term outcomes.
Moreover, while the overall 5-year survival was similar between PCI and CABG in patients with left main disease, regardless of diabetic status, the study indicated that in diabetic patients with significant atherosclerotic burden (high SYNTAX scores), CABG was associated with better survival outcomes. This finding suggests that the anatomical extent of the disease significantly influences the choice of revascularization strategy.
Additionally, patients treated with PCI had lower early stroke rates but faced higher rates of long-term myocardial infarction and repeat revascularizations compared to those treated with CABG. For example, diabetic patients treated with PCI exhibited 8.9 % incidence of spontaneous myocardial infarction compared to 4.4 % in those who underwent CABG.
These data should not merely fuel the procedural debates, but should be used to enhance patient-centered care. In real-world clinical settings, decisions are ideally made with a comprehensive 'Heart Team' approach considering clinical, anatomical factors, patient preference and social circumstances. The choice between PCI and CABG involves balancing the benefits of reduced invasiveness and quicker recovery with PCI against the longer-term durability and lower re-intervention rates with CABG.
The discussions on PCI vs. CABG for left main coronary artery disease need to move beyond dichotomies and embrace a more nuanced understanding of each patient’s unique clinical profile. This approach ensures that treatment decisions are not only based on broad clinical trial results, but are tailored to individual patient needs, potentially improving both outcomes and patient satisfaction. An important issue, captured by the SYNTAX score, is not the left main disease per se but the associated triple vessel disease.
The continuous refinement of PCI, with a burgeoning toolkit that includes intravascular ultrasound (IVUS) and optical coherence tomography (OCT) for superior plaque characterization, as well as pressure wire assessments for functional lesion significance, will enhance procedural success rates. Moreover, lithotripsy's adaptation for modifying calcified coronary lesions may abrogate some of the historical limitations of PCI in heavily calcified vessels, a frequent concern in diabetic atherosclerosis.
We summarize the messages of this study in these points:
- Treatment strategy tailoring: Decisions between percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) for left main coronary artery disease should be tailored to individual patient profiles, including diabetes status and anatomical disease complexity, to optimize outcomes.
- Diabetes as a determinant: Patients with diabetes experience higher rates of adverse events such as death, myocardial infarction, and repeat revascularizations when treated for left main coronary artery disease, highlighting the need for careful consideration of revascularization strategy in this subgroup.
- Balancing short and long-term benefits: While PCI offers advantages in terms of lower early stroke rates, CABG provides more durable protection against myocardial infarction and the need for future revascularizations. This illustrates the importance of balancing short-term benefits with long-term outcomes. Specifically, patients treated with PCI had lower early stroke rates but faced higher rates of spontaneous MI and repeat revascularizations compared to those treated with CABG.
- Collaborative decision-making: A heart team approach involving cardiologists, surgeons, and other healthcare professionals is crucial for discussing revascularization options, ensuring that treatment decisions are based on a comprehensive evaluation of clinical evidence and patient preferences.
- Evolving treatment paradigms: Ongoing debates and research should focus on the complementary roles of PCI and CABG rather than positioning them as competitive options, with the goal of advancing guidelines and clinical practices that reflect the latest evidence and patient-centered care principles. New way to perform PCI, such as the use of imaging and physiology, and the extensive application of new technologies (for instance: lithotripsy, DCBs) could represent a game changer.






No comments yet!