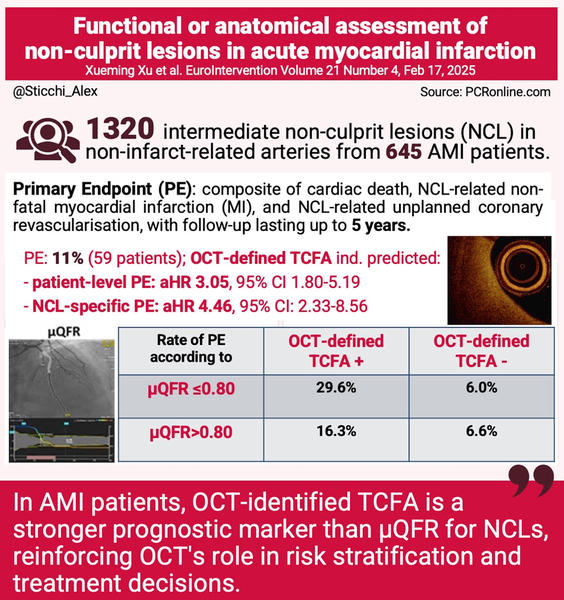
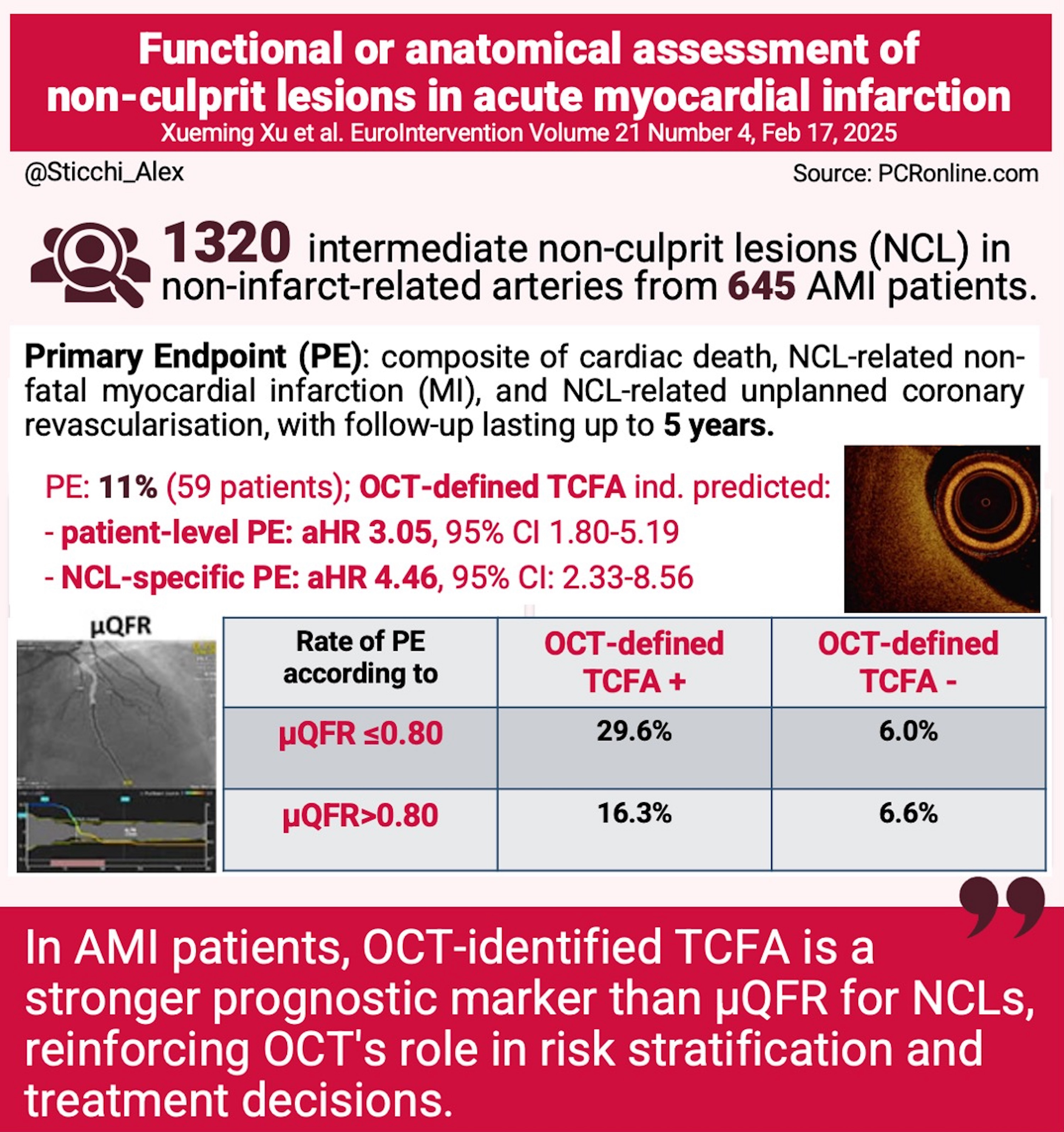
Functional or anatomical assessment of non-culprit lesions in acute myocardial infarction
Selected in EuroIntervention Journal by A. Sticchi
This study demonstrates that OCT-defined TCFA is a superior prognostic marker compared to μQFR for assessing NCLs in AMI patients.
References
Authors
Xu Xueming,Fang Chao,Jiang Senqing,Chen Yuzhu,Zhao Jiawei,Sun Sibo,Wang Yini,Li Lulu,Huang Dongxu,Li Shuang,Yu Huai,Chen Tao,Tan Jinfeng,Liu Xiaohui,Dai Jiannan,Mintz Gary,Yu Bo
Reference
DOI: 10.4244/EIJ-D-24-00720
Published
Feb 17, 2025
Link
Read the abstractReviewer
My Comment
Designed by Alessandro Sticchi. Source: PCRonline
Why this study – the rationale/objective?
Non-culprit lesions (NCLs) in acute myocardial infarction (AMI) patients are associated with an increased risk of future adverse cardiac events.
While physiological assessment techniques like quantitative flow ratio (QFR) provide insight into lesion significance, optical coherence tomography (OCT)-defined thin-cap fibroatheroma (TCFA) offers morphological evaluation of vulnerable plaques.
The study aims to compare the prognostic implications of Murray fractal law-based QFR (μQFR) and OCT-defined TCFA in AMI patients, assessing long-term outcomes related to NCLs.
The relevance of this study is reinforced by growing evidence supporting complete revascularisation in AMI patients, as recommended in the 2023 European guidelines for acute coronary syndromes. While physiological interrogation of NCLs has been previously supported in studies like Compare Acute and DANAMI-3-PRIMULTI, concerns persist regarding the reliability of functional assessments in AMI settings. This study seeks to clarify the role of μQFR versus OCT in determining long-term outcomes.
How was it executed – the methodology?
This was a retrospective observational study analyzing 645 AMI patients who underwent three-vessel OCT imaging and μQFR assessment, covering 1,320 intermediate NCLs in non-infarct-related arteries. Patients were followed for up to 5 years, with the primary composite endpoint including cardiac death, NCL-related myocardial infarction (MI), and unplanned NCL-related revascularisation.
Key methodological aspects include:
- Patient selection: AMI patients who underwent successful primary PCI, excluding those with extreme vessel tortuosity, chronic total occlusion, or previous coronary interventions.
- Imaging and analysis: OCT was used to identify plaque morphology and TCFA, while μQFR was calculated using AI-powered fractal law-based algorithms from a single angiographic view.
- Statistical methods: the study accounted for clustering effects of multiple NCLs per patient, using Kaplan-Meier estimates, Cox proportional hazards regression models, and multivariate adjustments to identify independent predictors of adverse events.
What is the main result?
- OCT-defined TCFA was the dominant predictor of long-term adverse outcomes (adjusted hazard ratio [HR] 3.05, 95 % confidence interval [CI]: 1.80-5.19, p < 0.001 at the patient level; HR 4.46, 95 % CI: 2.33-8.56 at the lesion level).
- Patients with TCFA(+) and μQFR ≤ 0.80 had the highest event rate (29.6 %), significantly higher than other groups.
- μQFR ≤ 0.80 alone was not an independent predictor of long-term clinical outcomes.
- TCFA provided significant prognostic value for both STEMI (HR 3.27) and NSTEMI (HR 3.26) patients, whereas μQFR ≤ 0.80 did not.
- The cumulative incidence curve suggests that events in TCFA(+) lesions occur within weeks or months post-PCI, highlighting their clinical urgency.
Critical reading and the relevance for clinical practice
This study demonstrates that OCT-defined TCFA is a superior prognostic marker compared to μQFR for assessing NCLs in AMI patients.
These findings emphasize the importance of morphological plaque assessment for risk stratification and clinical decision-making in the acute setting of myocardial infarction. Future studies should explore whether early OCT-guided interventions for high-risk plaques can improve long-term clinical outcomes and reduce recurrent cardiac events.
Diagnostic implications:
The study underscores the superiority of OCT over μQFR in identifying high-risk non-culprit lesions (NCLs) in acute myocardial infarction (AMI) patients. While μQFR offers a functional assessment of lesion significance, it may not detect vulnerable plaques prone to rupture. OCT, with its high-resolution imaging, can identify morphological features such as thin-cap fibroatheromas (TCFAs), which are associated with a higher risk of adverse cardiac events. This distinction is crucial, as relying solely on functional assessments like μQFR or FFR may overlook lesions with vulnerable morphologies that could lead to future cardiac events. Studies have shown that non-culprit plaques with high-risk features, even if not flow-limiting, are linked to increased rates of ischemic recurrence.
Clinical decision-making:
The findings advocate for an imaging-guided strategy in managing NCLs among AMI patients. Identifying TCFAs through OCT can inform clinicians about the necessity for preventive interventions, potentially including preemptive percutaneous coronary intervention (PCI) or intensified medical therapy. The COMPLETE trial demonstrated that routine angiography-guided PCI of non-culprit lesions reduced the composite endpoint of cardiovascular death or myocardial infarction by 26%. However, the benefit of routine PCI of non-culprit lesions is, as a result, the non-culprit lesions having characteristics that were consistent with a vulnerable plaque is not known.
Comparison with existing guidelines:
Current guidelines recommend complete revascularisation in AMI patients with multivessel disease, often guided by functional assessments. However, this study, along with others, suggests that an imaging-guided approach using OCT may provide additional prognostic value by identifying plaques at higher risk of causing future events, regardless of their functional significance. This challenges the traditional reliance on functional metrics alone and supports incorporating morphological assessment into routine practice. The presence of high-risk plaque features in non-culprit lesions has been associated with an increased rate of ischemic recurrence, highlighting the potential benefit of imaging-guided strategies.
Limitations:
- Study design: the retrospective and single-center nature of the study introduces potential selection bias and limits the generalizability of the findings.
- Sample size: the relatively small number of patients with μQFR ≤0.80 may reduce the statistical power for subgroup analyses.
- Clinical outcomes: while OCT identifies morphological features of vulnerability, it remains to be conclusively proven whether interventions based on OCT findings alone improve long-term clinical outcomes.
- Resource availability: widespread implementation of OCT may be limited by availability, cost, and the need for specialized training.
In conclusion, integrating OCT into the evaluation of NCLs in AMI patients offers a more comprehensive assessment by revealing high-risk morphological features not detectable through functional assessment alone. This approach has the potential to enhance risk stratification and guide therapeutic decision-making, ultimately aiming to reduce recurrent cardiac events.
Future prospective, multicenter trials are warranted to validate these findings and to establish standardized protocols for OCT-guided management of non-culprit lesions in the context of acute myocardial infarction.




No comments yet!