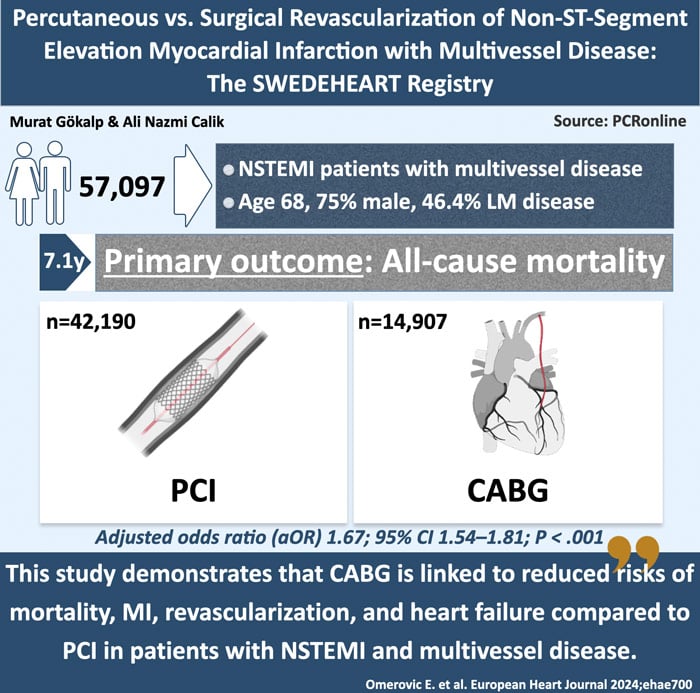
Percutaneous vs. Surgical revascularization of non-ST-segment elevation myocardial infarction with multivessel disease: The SWEDEHEART registry
Selected in European Heart Journal by A. N. Calik , M. Gökalp
This registry-based observational study compares surgical and percutaneous revascularization in patients with multivessel disease who underwent treatment for non-ST-segment elevation myocardial infarction (NSTEMI), utilizing data extracted from the SWEDEHEART registry.
References
Authors
Elmir Omerovic, Truls Råmunddal, Petur Petursson, Oskar Angerås, Araz Rawshani, Sandeep Jha, Kristofer Skoglund, Moman A Mohammad, Jonas Persson, Joakim Alfredsson, Robin Hofmann, Tomas Jernberg, Ole Fröbert, Anders Jeppsson, Emma C Hansson, Göran Dellgren, David Erlinge, Björn Redfors
Reference
European Heart Journal, ehae700
Published
November 27, 2024
Link
Read the abstractReviewers
Our Comment
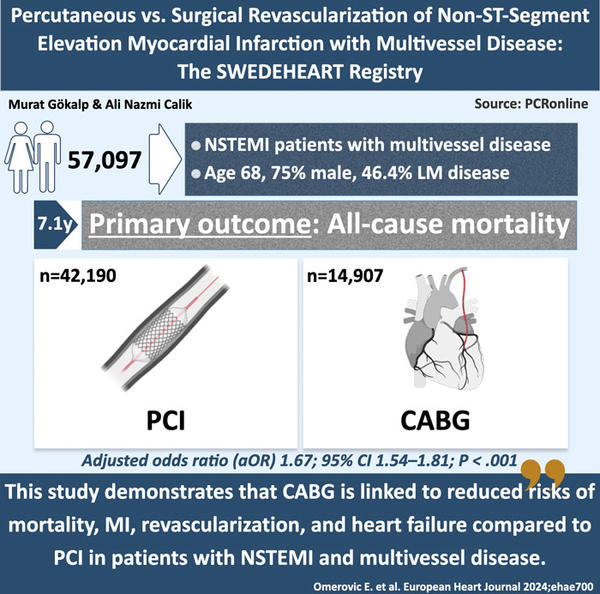
Designed by Murat Gökalp & Ali Nazmi Calik - Source: PCRonline
Why this study – the rationale/objective?
Patients with NSTEMI should undergo early invasive revascularization in accordance with current European and American guidelines.1,2. The advancement of percutaneous techniques has established them as a cornerstone in reducing the risk of cardiovascular events in patients with NSTEMI. Nevertheless, coronary artery bypass grafting (CABG) remains an important treatment strategy for patients with left main or complex multivessel coronary artery disease, as well as for those with anatomy that is unsuitable for percutaneous coronary intervention (PCI).
Upon reviewing the literature, the comparison between CABG and PCI in multivessel NSTEMI patients appears to be limited. Additionally, the proportion of NSTEMI patients in the overall patient distribution is notably low. In studies focusing on left main coronary lesions, such as EXCEL (Everolimus-Eluting Stents or Bypass Surgery for Left Main Coronary Artery Disease) and NOBLE (Nordic-Baltic-British Left Main Revascularization), CABG has been associated with improved long-term survival and a lower incidence of cardiovascular events in patients with complex coronary lesions.3-5. Currently, there is a lack of studies that directly compare the two strategies in NSTEMI patients with multivessel lesions.
This study aimed to evaluate the long-term outcomes of PCI versus CABG in patients with NSTEMI and multivessel disease.
How was it executed – the methodology?
The study utilized data from the SWEDEHEART registry, which included revascularized patients with multivessel NSTEMI who met the universal definition of myocardial infarction (MI) as outlined in current guidelines, spanning from January 2005 to June 2022. In this observational study, participants were categorized into two groups based on the revascularization method used during their initial hospitalization: either CABG or PCI. Patients with cardiogenic shock or cardiac arrest, as well as those with a history of stroke, dementia, renal failure, or cancer, were excluded from the analysis. Additionally, individuals presenting with unstable angina or those who underwent both PCI and CABG were also excluded.
The primary outcome of the study was all-cause mortality, defined as death from any cause. This includes both in-hospital mortality (deaths occurring during the initial hospitalization following the NSTEMI event) and long-term mortality (deaths occurring after discharge during the follow-up period). The secondary outcomes included MI, stroke, the need for new revascularization, and heart failure.
What is the main result?
Between January 2005 and June 2022, a total of 57,097 patients were included in the study. Among these, 42,190 patients (73.9%) underwent PCI, while 14,907 patients (26.1%) received CABG. The overall cohort comprised 75.8% men and 24.2% women, with a mean age of 68.7 years (± 10.5). On average, patients in the PCI group were one year older than those in the CABG group. Furthermore, the PCI group exhibited a higher prevalence of previous PCI, CABG, MI, and hypertension. In contrast, the CABG group demonstrated a greater incidence of diabetes, left main coronary artery disease, three-vessel disease, Killip class greater than 2, and pathological ST-T segment changes on ECG.
During a median follow-up period of 7.1 years, patients who underwent PCI exhibited a 67% higher adjusted odds ratio (aOR) for all-cause mortality compared to those who received CABG, with an aOR of 1.67 (95% confidence interval [CI] 1.54–1.81; P< .001). The advantages of CABG became increasingly apparent, particularly starting five years post-revascularization. The mortality benefit associated with CABG over PCI was consistently observed at each annual follow-up interval. Throughout the entire 10-year follow-up period, CABG consistently demonstrated a lower risk of all-cause mortality compared to PCI.
Throughout the entire follow-up period, the risk of MI was significantly higher in the PCI group, demonstrating a 51% increased risk compared to the CABG group (aOR 1.51; 95% CI 1.41–1.62; P < .001). However, in the first year following revascularization, the CABG group exhibited a higher risk of MI (aOR 1.31; 95% CI 1.21–1.41; P < .001). There was no significant difference in the risk of stroke between the two groups (aOR 0.93; 95% CI 0.85–1.03; P = .215). Additionally, the likelihood of requiring repeated revascularization was three times greater in the PCI group (aOR 3.01; 95% CI 2.57–3.51; P < .001).
Lastly, the risk of heart failure during the entire follow-up period was also higher in the PCI group, with a 15% increased risk compared to the CABG group (aOR 1.15; 95% CI 1.07–1.25; P < .001). In the subgroup analysis of the study, CABG demonstrated a significantly greater survival benefit for patients with left ventricular dysfunction, those with severe coronary artery disease, and individuals under the age of 70 (all Pinteraction < .001).
Critical reading and the relevance for clinical practice
This study, utilizing data from the SWEDEHEART registry, offers valuable insights into the comparison of revascularization strategies for NSTEMI patients with multivessel disease. The results indicated that CABG consistently resulted in a 41% lower risk of all-cause mortality compared to PCI over the entire 10-year follow-up period. Furthermore, the rates of recurrent MI and the need for repeated revascularization were significantly lower in the CABG group than in the PCI group. This advantage was particularly evident among certain subgroups, including patients with left main disease, left ventricular dysfunction, and those younger than 70 years.
These results are consistent with earlier studies and meta-analyses indicating that CABG is more effective than PCI in improving long-term survival for patients with complex coronary artery disease. The findings further underscore that CABG offers a more durable solution for patients with reduced LVEF, providing enhanced protection against ischemic events over time. Conversely, PCI remains a viable treatment option for patients with less complex coronary conditions; however, it is linked to higher rates of recurrent revascularization and a slightly elevated risk of MI in the early post-procedural phase.
Although the study's findings are compelling, they originate from an observational cohort, which is an important factor to consider. The absence of randomization means that the observed differences between the PCI and CABG groups may be attributable to baseline patient characteristics rather than the revascularization techniques themselves. Furthermore, while the long-term follow-up is a significant strength of the study, shifts in clinical practice, advancements in PCI technology (including newer drug-eluting stents), and changes in post-procedural care throughout the study period could influence the applicability of the results.
One significant limitation of the study is the lack of specific procedural details, such as the types of grafts used in CABG or the particular stent technologies utilized in PCI. For instance, the choice between arterial and vein grafts in CABG may affect outcomes, as arterial grafts are generally linked to improved long-term survival compared to vein grafts. Similarly, the type and number of stents employed in PCI can influence long-term revascularization results. The lack of SYNTAX scores and comprehensive procedural data limits the ability to conduct more detailed evaluations of the relationship between the complexity of coronary disease and revascularization outcomes.
From a clinical perspective, the study strongly advocates for CABG as a revascularization strategy for NSTEMI patients with multivessel coronary artery disease, particularly in high-risk subgroups, including those with left main disease, left ventricular dysfunction, and younger patients. Further, this study emphasizes the importance of a personalized approach to determining the most suitable revascularization strategy. Clinical decisions should consider factors such as comorbidities, coronary anatomy, and patient preferences, ensuring tailored treatment for each individual. Further randomized controlled trials comparing contemporary PCI techniques with CABG are essential to validate these findings and update clinical guidelines for this complex patient group.
References
- Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J 2023;44: 3720–826. https://doi.org/10.1093/eurheartj/ehad191
- Lawton JS, Tamis-Holland JE, Bangalore S, Bates ER, Beckie TM, Bischoff JM, et al. 2021 ACC/AHA/SCAI Guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2022;145:e18–114. https://doi.org/10.1161/CIR.0000000000001038
- Stone GW, Sabik JF, Serruys PW, Simonton CA, Genereux P, Puskas J, et al. Everolimus-eluting stents or bypass surgery for left main coronary artery disease. N Engl J Med 2016;375:2223–35. https://doi.org/10.1056/NEJMoa1610227
- M Makikallio T, Holm NR, Lindsay M, Spence MS, Erglis A, Menown IB, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet 2016;388:2743–52. https://doi.org/10.1016/S0140-6736(16)32052-9
- Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severecoronary artery disease. N Engl J Med 2009;360:961–72. https://doi.org/10.1056/NEJMoa0804626





No comments yet!