Coronary arteries
Anatomy of the Aortic Valvar Complex
The coronary arteries arise from the aortic sinuses. The initial portion of the aortic root, which houses the leaflets of the aortic valve, is occupied by the aortic sinuses, also called the sinuses of Valsalva. The aortic sinuses reach beyond the upper border of the cusp and form a well-defined, complete, and circumferential sinotubular ridge when viewed from the aortic aspect. These sinuses are named according to their position as the anterior, left posterior, and right posterior aortic sinuses. The right coronary artery arises from the anterior coronary sinus and the left coronary artery from the left posterior aortic sinus.
Origins of the coronary arteries
In the majority of cases, the coronary arteries arise from two separate orifices located within the left and right coronary aortic sinuses (Figure 16)14,19. Most arise below the sinotubular junction, although take-off at (9%) or above (22%) the junction is not uncommon20. Knowledge of the height of the coronary arteries with respect to the basal attachment of the native valve leaflets is important for those undertaking TAVI. Post-mortem examination of normal hearts shows that the left and right coronary arteries arise on average 12.6 ± 2.61 mm and 13.2 ± 2.64 mm from the basal attachment of their respective leaflets21.

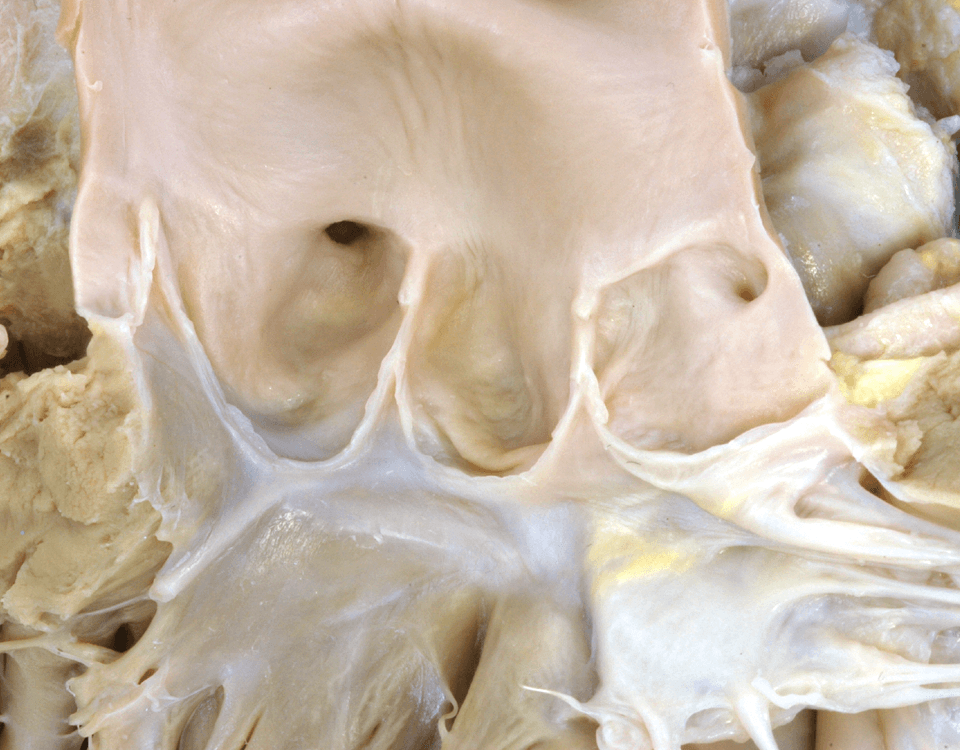
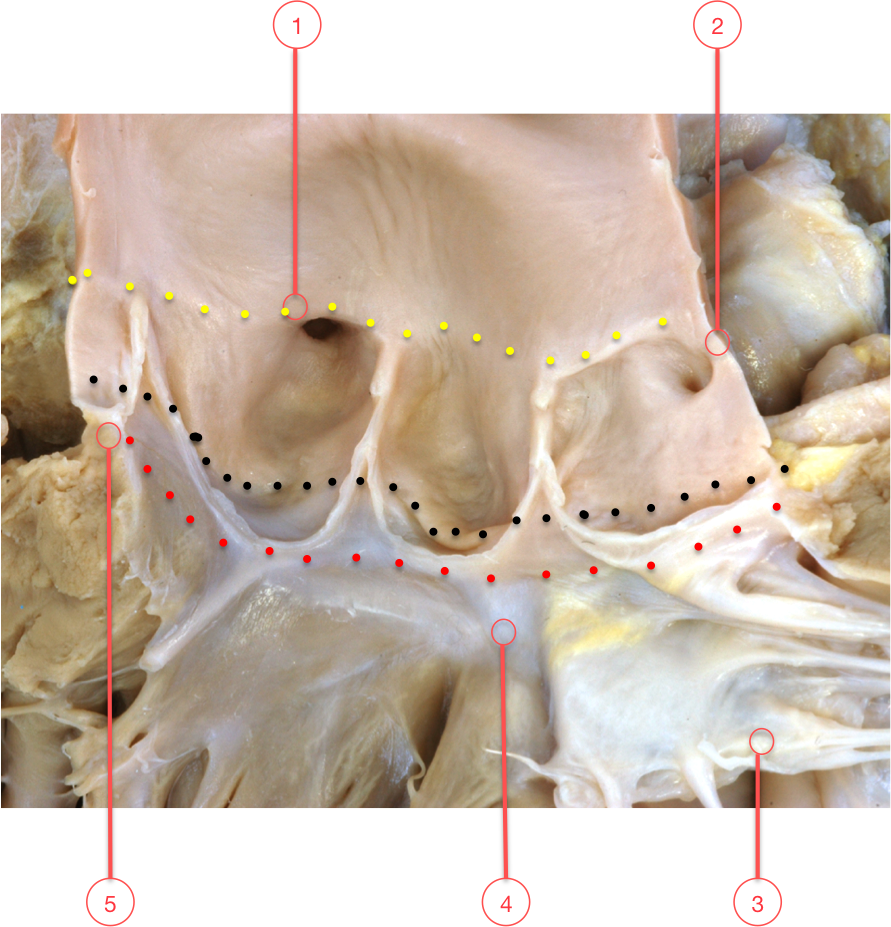
Figure 16. Origins of the coronary arteries
This figure demonstrates three lines within the aortic root, the sinotubular junction (yellow dots), the anatomic ventriculo-arterial junction (black dots) and the line marking the most proximal portion of the aortic root (red dots). The sinotubular junction and the anatomic ventriculo-arterial junction form true lines within the aortic root. The line represented by the red dots is a virtual line and represents the most proximal attachment of the aortic valvar leaflets within the left ventricular outflow tract or aortic root.
The aortic valvar leaflets cross the anatomic ventriculo-arterial junction at six points around the circumference of the valve, incorporating a crescent of muscle into the base of the sinus of the right coronary aortic leaflet and a portion of the left coronary aortic leaflet. Typically, the non-adjacent sinus has fibrous tissue in this area with fibrous tissue making up the remainder of the base of the left sinus.
In this heart, the interleaflet triangle between the right coronary aortic sinus and the non-adjacent sinus is supported by muscle and does not reach the right fibrous trigone and the rightward extent of the membranous septum.
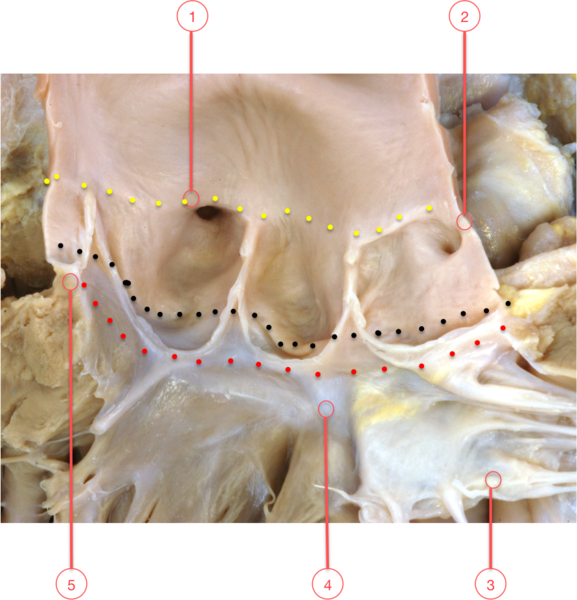
Figure 16. Origins of the coronary arteries
1 - Right coronary orifice
2 - Left coronary orifice
3 - Mitral valve
4 - Membranous septum
5 - Ventriculo-arterial junction
Accurate assessment of the distance between the basal attachment point of the leaflets and the coronary arterial orifices is an important component of screening in advance of implantation, and of procedural planning. All current prostheses available for TAVI are designed with a skirt of fabric or tissue sewn within the stent or frame in order to create a seal with the native aortic root and reduce paravalvular leak.
If the origin of the coronary arteries is low within the sinuses of Valsalva, and/or the prosthesis is placed too high, the skirt can obstruct the arterial orifices and rapidly induce myocardial ischaemia and haemodynamic collapse (Myocardial infarction) [link]. An identical situation can be observed if the deployment of the prosthesis displaces the native leaflets such that they cover the arterial orifices in patients with low-lying coronary arteries.
Consequently, the height of the orifices within the sinuses should be assessed using multislice computed tomography (MDCT) (Prosthesis size).
According to the MDCT, the mean distance from the basal attachment point of the leaflets to the orifices of the left coronary and right coronary arteries was 14.4 ± 2.9 mm and 17.2 ± 3.3 mm, respectively9. Although these measurements were similar in those with and those without aortic stenosis, there was important variability which underscores the need for assessment in individual patients, the more so since the height of the orifice of the left coronary artery ranged from 7.1 to 22.7 mm9.
The width of the sinuses of Valsalva has also been recognised to be an important determinant of potential arterial occlusion in the setting of TAVI (Prosthesis size). A minimum sinus width is recommended in order to accommodate the redundant native aortic leaflets (consult Medtronic CoreValve criteria).
In cases where transcutaneous implantation is being considered for treatment of a failing surgical bioprosthesis, it is important to know both the position (annular or supra-annular implantation) and design characteristics of the surgical prosthesis, as coronary arterial occlusion is more commonly described than TAVI for native aortic valves stenosis. For more information, consult Coronary obstruction [Link].