RIPCORD 2: does routine pressure wire assessment influence management strategy of coronary angiography for diagnosis of chest pain?
Reported from the European Society of Cardiology ESC Congress 2021
Why this study – rationale/objective
The benefits of intracoronary physiology have been demonstrated in intermediate lesions in patients already selected to undergo PCI. In the pilot RIPCORD trial the investigators showed that systematic assessment of all vessels with FFR changed management strategy in a quarter of patients.
The rationale of the RIPCORD2 trial was to address the hypothesis the systematically assessing all vessels >2.25mm in diameter with >30% visual stenosis would be superior to angiography alone in terms of resource utilisation and quality of life at one year.
How was it executed – the methodology
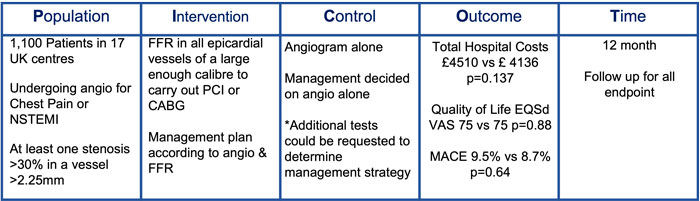
Ripcord 2 was an open-label, multicentre randomised control trial conducted in 17 UK centres. Patients undergoing angiography for unstable angina or NSTEMI with any epicardial stenosis visually > 30 % in at least one vessel amenable to PCI/CABG (approx. 2.25 mm) were randomised to systematic FFR or angiography alone. FFR assessment of all epicardial vessels of a calibre amenable to PCI or CABG was carried out in the FFR arm and this information integrated into operator decision making. Following angiography +/- FFR the operator determined the management plan 1) OMT alone, 2) PCI, 3) CABG, 4) more information/further tests required
- The co-primary endpoints were total hospital costs and quality of life (EQ-5D-5L questionnaire) at 12 months
- The prespecified secondary endpoints were clinical events at 12 months.
What is the main result?
RIPCORD 2 randomised 1100 patients, 584 to systematic FFR assessment and 552 to angiography alone. The majority (75%) were men in their 60’s with typical cardiovascular risk factors. Over half the population presented with ACS. Overall it was a low complexity population with 71% having angiographically 0 or 1 vessel disease.
- At 12 month follow up total hospital costs did not vary between the systematic FFR group and the angio only group £4510 (2721-7415) vs. £4136 (2613-7015) p=0.137
- There were no differences in quality of life between the two groups 75 (60-90) vs 75 (60-87) p=0.88
- Overall MACE did not vary between FFR guided and angio guided 9.5% vs. 8.7% p=0.64
- Further tests were requested in 14.7% of the angiographic guidance group vs 1.8% of the systematic FFR group p<0.00001
- FFR guided group had longer procedures (69min vs. 42.4min, p<0.001), more contrast (206ml vs. 146.2ml, p<0.001) and radiation (5292.3cGy/cm2 vs. 5029.7cGy/cm2, p<0.001) use
- Systematic FFR was associated with a complication rate of 1.8%
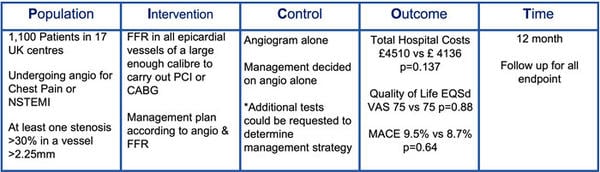
Analysis according to the PICOT principle - courtesy of Nicola Ryan
Critical Interpretation and relevance for clinical practice
It must be understood that the paper has yet to be published for RIPCORD 2 therefore all assumptions are based upon the presented data.
The results of this study show that there is no benefit in terms of resource utilisation, quality of life or clinical outcomes at one year from systematic use of FFR in patients undergoing diagnostic angiography. In RIPCORD the overall complexity of the disease was low with the majority of patients having angiographically 0 or 1 vessel coronary artery disease, in these patients use of physiology may have had a lower impact on their overall treatment strategy compared to patients with multivessel CAD. Use of intracoronary physiology to assess intermediate stenosis is established in clinical practice and supported by the guidelines and several large clinical trials.
The investigators included any visual stenosis >30% in vessels >2.25mm in diameter, given the myocardium subtended by the majority of 30-50% stenosis it is unlikely that these will be sufficiently flow limiting to produce an ischaemic FFR, the proximal LAD being the obvious exception. Furthermore many operators would not consider stent implantation in a vessel of 2.25mm. In this study the individual effect of the FFR measurements were not reported, it maybe that whilst at a population level there was no benefit selective use of FFR may have provided individual patient benefit.
The results of RIPCORD 2 can be interpreted as routine use of pressure wire in all vessels at the time of diagnostic angiography should not be recommended. However selective use of intracoronary physiology remains appropriate, 14.7% of the angiography guided group required further testing to determine a management strategy in this cohort, intracoronary physiology at the time of the diagnostic angiogram may have assisted in timely decision making.
Related interview
View this interview with Nick Curzen, principal investigator of RIPCORD 2




No comments yet!