Everolimus-eluting stents or bypass surgery for mutivessel coronary artery disease: 10-year outcomes of multicenter randomized controlled BEST trial
Reported from TCT 2022
Nicola Ryan provides her take on the BEST trial which was presented by Jung-Min Ahn at TCT 2022.
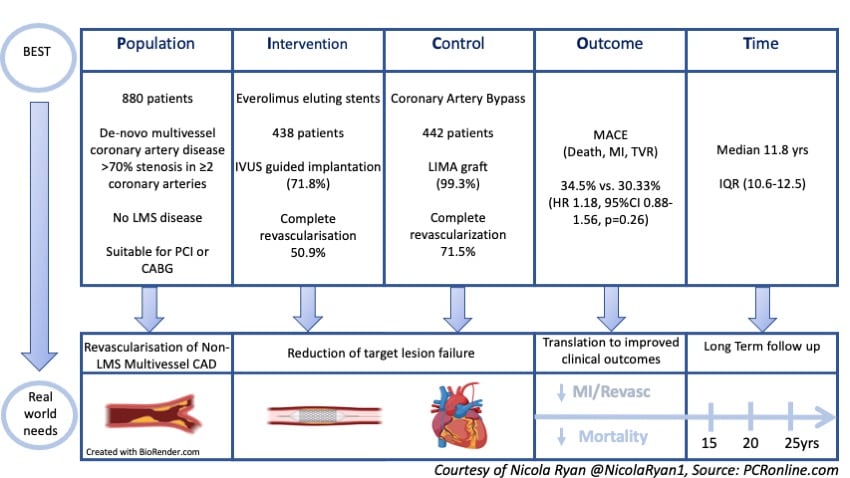
It is a randomised, multicentre, non-inferiority trial comparing PCI with second-generation everolimus-eluting stents and CABG in patients with non-left main multivessel coronary artery disease. At two-year follow-up PCI was shown to be non-inferior to CABG in terms of death, MI or target vessel revascularisation, however, at longer follow-up (median of 4.6 years) there was an increased incidence of the composite of death, MI and TVR in the PCI group, mainly driven by repeat revascularisation. In this extended follow-up, the authors report the outcome out to a median of 11.8 years.
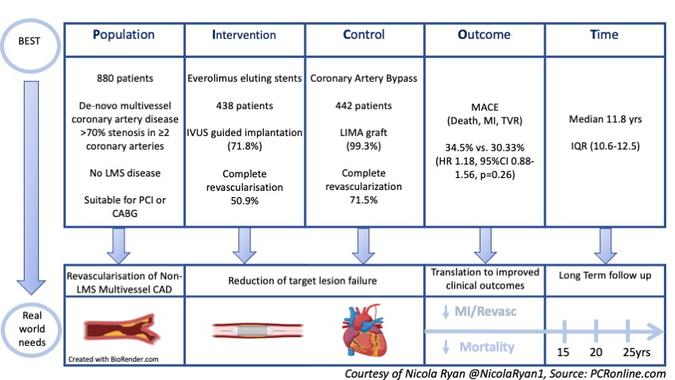
PICOT analysis of the BEST trial.
Courtesy of Nicola Ryan @NicolaRyan1, Source: PCRonline.com
Why this study – the rationale/objective?
There is limited data with regard to the longer-term outcomes of percutaneous coronary intervention (PCI) versus coronary artery bypass grafting (CABG) in patients with multivessel coronary artery disease. The SYNTAX (1) and FREEDOM (2) trials which showed a survival benefit for CABG are limited by the use of first-generation DES and to date, there is limited follow-up for FAME III (3). Furthermore, procedural aspects such as suboptimal stent implantation may also influence clinical outcomes. DES implantation guided by intra-coronary imaging (IVUS or OCT) has been shown to be superior to angiography-guided DES implantation in terms of stent restenosis and thrombosis (4,5). The relatively low utilisation of IVUS in other trials has been considered a limitation. In this extended follow-up, the authors present the long-term outcomes of PCI with second-generation DES versus CABG in a population with high rates of IVUS use and LIMA grafting.
How was it executed - the methodology?
Patients undergoing angiography with lesions >70% in major epicardial arteries in the territories of at least two coronary arteries without LMS involvement deemed suitable for treatment with PCI or CABG were eligible for inclusion. In the PCI arm, the protocol required treatment of all lesions with everolimus-eluting stents with the use of IVUS at the discretion of the operator. In the CABG arm, the internal mammary artery was recommended for revascularisation of the LAD. In this extended follow-up, the participating centres were invited to participate in February 2022 and clinical follow performed via clinic visits, telephone interviews, medical records and national health insurance service database.
- The primary endpoint was MACE a composite of death, MI or target vessel revascularisation.
- Secondary endpoints included a safety composite of death, MI or stroke and a composite of death, MI, stroke or any repeat revascularisation.
What is the main result?
Overall, between July 2008 and September 2013, 880 patients were included in the trial, 438 randomised to PCI with everolimus-eluting stents (EES) and 442 to CABG. The trial was stopped early in October 2013 due to slow enrolment (880/1776). The majority of patients were men in their 60’s with high rates of diabetes (41%) and three-vessel disease (77%). Complete revascularisation was achieved in 50.9% of the PCI group and 71.5% of the CABG group. IVUS was used in 71.8% of cases with 99.3% of patients receiving a LIMA to the LAD. Near complete follow-up was achieved, 98.3% in the PCI group and 99.9% in the CABG group, with a median follow of 11.8 years (10.6-12.5).
- There was no difference in the primary endpoint (death, MI, TVR) between groups PCI 34.5% vs. CABG 30.3% (HR 1.18, 95% CI 0.88-1.56, p=0.26).
- The safety endpoint was similar between groups 28.8% PCI vs. 27.1% CABG (HR 1.07, 95% CI 0.75-1.53, p=0.70).
- Spontaneous MI (7.1% vs. 3.8%, HR 1.86, 95%CI 1.06-3.27, p=0.03) and repeat revascularisation (22.6% vs. 12.7%, HR 1.92, 95%CI 1.58-2.32, p<0.001) were more common after PCI.
- In the PCI group, IVUS use was associated with a lower rate of the primary endpoint compared to no-IVUS use (HR 0.45, 95%CI 0.33-0.61, p<0.001).
Critical reading and the relevance for clinical practice
The results of this study show that in patients with non-LMS multivessel coronary artery disease the rate of death, MI or TVR was not significantly different between patients treated with second-generation everolimus-eluting stent and patients treated with CABG at long-term follow-up. Importantly the rates of spontaneous MI and repeat revascularisation were higher in the PCI group. A key caveat that must be borne in mind when interpreting the results of this trial is that the BEST trial was terminated early due to slow recruitment and therefore is underpowered for clinical endpoints.
Multiple factors influence the outcomes after implantation of DES including technical factors related to both implantation and stent design, clinical presentation, lesion characteristics and medical therapy. In this trial the use of both second generation DES as well as the high rates of IVUS adoption may explain the differences between this and the SYNTAX and FREEDOM trials. Interestingly in the PCI subgroup, IVUS use was associated with a lower rate of the primary endpoint. Furthermore, there were high rates of statin prescription in both groups at follow-up. Medical therapy for secondary prevention of CAD has significantly evolved since the trial began recruitment which may improve overall outcomes in both groups. Over the 14-year period since the trial began recruitment surgical techniques have also evolved, as demonstrated by the lower than expected event rate in the surgical arm of the FAME III trial therefore contemporary CABG may have lower event rates than those demonstrated in this study.
Of note, the majority of patients in this trial had low or intermediate SYNTAX Scores and were deemed suitable for intervention with either PCI or CABG therefore generalisation to a wider population cannot be assumed. Furthermore, complete revascularisation was only achieved in 50% of the PCI arm, given that incomplete revascularisation has been associated with increased event rates consideration needs to be given to the ability to achieve complete revascularisation when discussing revascularisation strategies both within the heart team and with patients. Overall, this study provides important data with regard to the long-term outcomes of patients undergoing both PCI and CABG with non-LM multivessel disease and allows informed discussions between physicians and their patients with regard to the event rates with both revascularisation modalities.
References
- Thuijs DJFM, Kappetein AP, Serruys PW, Mohr FW, Morice MC, Mack MJ, et al. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomised controlled SYNTAX trial. The Lancet. 2019 Oct 12;394(10206):1325–34.
- Farkouh ME, Domanski M, Dangas GD, Godoy LC, Mack MJ, Siami FS, et al. Long-Term Survival Following Multivessel Revascularization in Patients With Diabetes. Journal of the American College of Cardiology. 2019 Feb 19;73(6):629–38.
- Fearon WF, Zimmermann FM, De Bruyne B, Piroth Z, van Straten AHM, Szekely L, et al. Fractional Flow Reserve–Guided PCI as Compared with Coronary Bypass Surgery. New England Journal of Medicine. 2022 Jan 13;386(2):128–37.
- Shin DH, Hong SJ, Mintz GS, Kim JS, Kim BK, Ko YG, et al. Effects of Intravascular Ultrasound–Guided Versus Angiography-Guided New-Generation Drug-Eluting Stent Implantation: Meta-Analysis With Individual Patient–Level Data From 2,345 Randomized Patients. JACC: Cardiovascular Interventions. 2016 Nov 14;9(21):2232–9.
- Zhang J, Gao X, Kan J, Ge Z, Han L, Lu S, et al. Intravascular Ultrasound Versus Angiography-Guided Drug-Eluting Stent Implantation: The ULTIMATE Trial. Journal of the American College of Cardiology. 2018 Dec 18;72(24):3126–37.






No comments yet!