27 Aug 2023
The GUIDE-DES Trial - QCA versus IVUS guidance for DES implantation
Reported from ESC Congress 2023
Quantitative coronary angiography-guidance versus intravascular ultrasound-guidance for drug-eluting stent implantation (GUIDE-DES trial): A multicenter, non-inferiority, randomised-controlled trial
Nicola Ryan provides her take on the final results of GUIDE-DES which were presented by Taeoh Kim during the ESC 2023 congress in Amsterdam.
Note the assumptions in this article are based on the presentation alone as the trial has not yet been published.
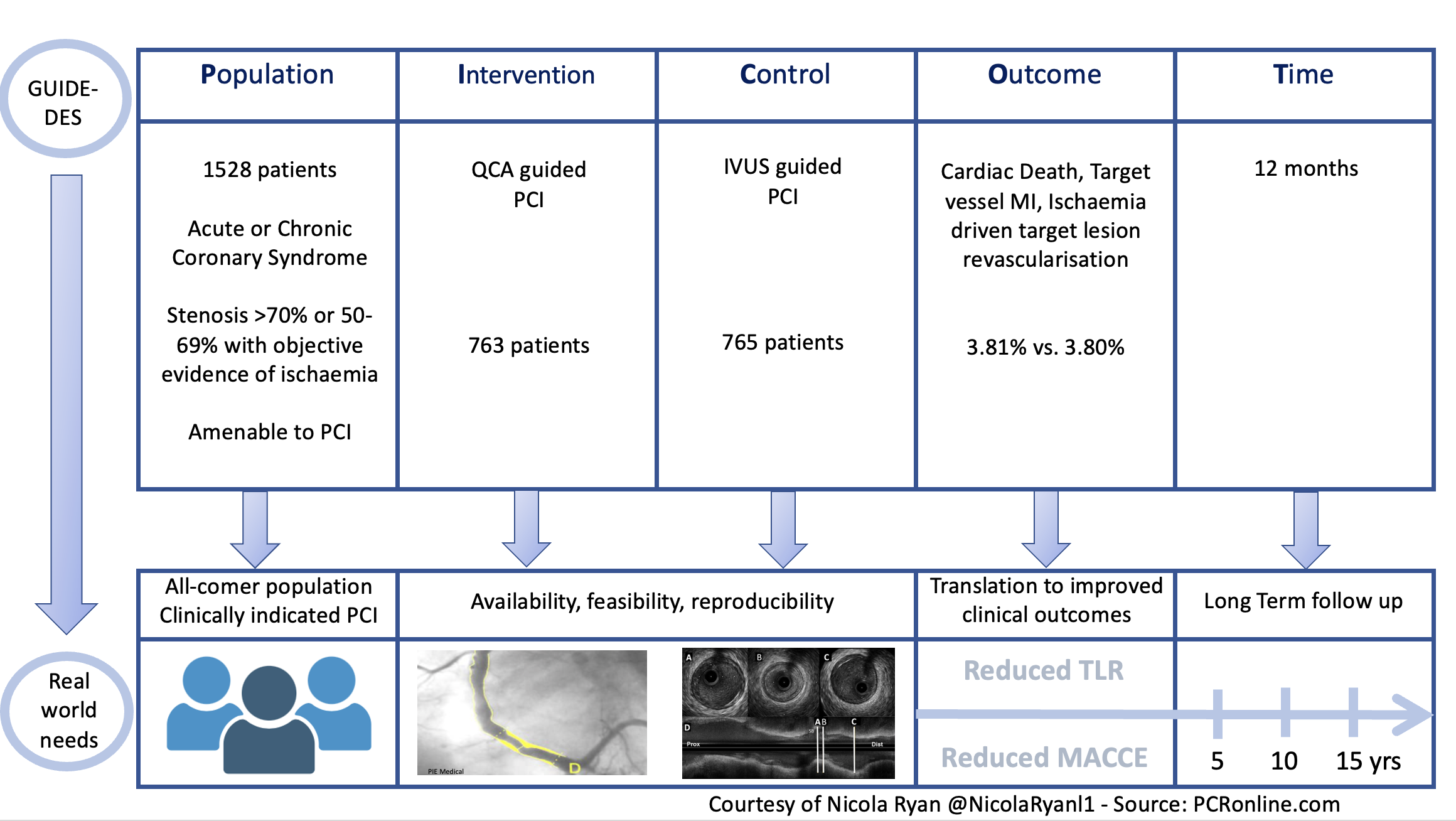
The GUIDE-DES trial is a multicenter, non-inferiority randomised control trial comparing on-site QCA-guided PCI with IVUS-guided PCI in patients undergoing PCI with DES implantation.
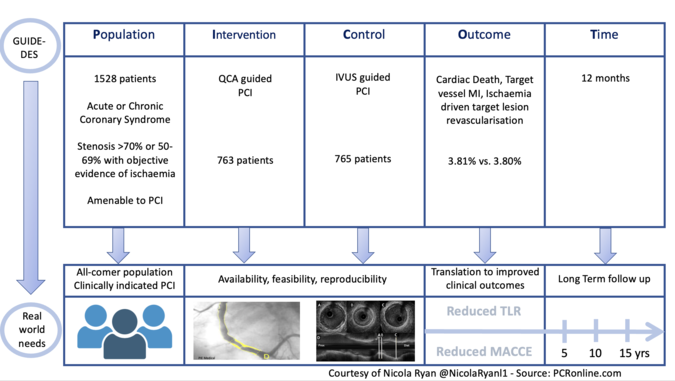
PICOT analysis of Guide DES - Courtesy of Nicola Ryan @NicolaRyanl1 - Source: PCRonline.com
Why this study – the rationale/objective?
Prior studies have shown improved outcomes in IVUS-guided PCI compared to angiography-guided PCI yet IVUS penetration remains low. The authors hypothesized that angiography-based PCI is limited by use of visual estimation of vessel size as well as lower rates of post-dilatation leading to inadequate stent deployment and poorer clinical outcomes. This trial used adjusted QCA as well as mandated post dilatation in order to attempt to overcome the limitations of angiography-guided PCI.
How was it executed - the methodology?
Patients presenting with typical chest pain or evidence of myocardial ischaemia with significant coronary artery stenosis, diameter stenosis ≥70% or 50-69% with objective evidence of ischaemia deemed amenable to intervention with PCI were eligible for inclusion in the study.
Patients were randomised 1:1 to QCA-guided DES implantation or IVUS-guided stent implantation. In the QCA guided arm, the target diameter was the measured QCA diameter + 5-10% of the measured QCA value. Protocol-mandated post-dilatation to optimise the stent at its edge and within the stent with high-pressure dilation with non-compliant balloons.
The ideal final result was defined as harmonious appearance (smooth tapering off) between the reference segment and the stent without dissection and minimal residual stenosis (<10%) on angiography.
IVUS criteria for stent optimisation were; 1) in-stent MLA > distal reference segment’s lumen CSA, 2) complete stent apposition, 3) no significant proximal or distal edge dissection (media dissection, dissection angle ≥60°, or dissection length > 2mm).
- The primary endpoint was target lesion failure, a composite of cardiac death, target vessel MI or ischaemia-driven target lesion revascularisation at 12 months.
- Secondary endpoints included death, MI, definite or probable stent thrombosis, stroke, target lesion revascularisation, any revascularisation, and economic analysis at 12 months.
What is the main result?
Recruitment to the trial began in September 2018, overall, 1528 patients were randomised; 763 assigned to QCA guided PCI and 765 assigned to IVUS guided PCI. In 7 of the QCA group IVUS was used to evaluation potential complications and post PCI IVUS failed in 6 of the IVUS group. The majority of patients were men in their 60’s with typical CVRF, 70% of the population presented with chronic coronary syndrome. Whilst half the population had multivessel disease the SYNTAX Score was low at 13, no information was provided with regard to lesion complexity or the presence of bifurcation disease, though from the rationale and design paper extreme angulation ≥90° proximal to or within the target lesion excessive tortuosity 2 ≥45° angles proximal to or within the target lesion and heavy calcification proximal to or within the target lesion were all exclusion criteria (1). Almost half of treated lesions were in the LAD with post dilatation carried out in 97%
- There was no difference in the primary endpoint 3.81% in the QCA guided arm versus 3.80% in the IVUS guided arm at 12 months, p for non-inferiority 0.0002
- Amongst the secondary endpoints there were no differences between the arms at 12 months.
Critical reading and the relevance for clinical practice
The results of this study show in this population QCA-guided DES implantation was non-inferior to IVUS-guided DES implantation in terms of target lesion failure at 12 months. Key to interpreting the results of this trial is appreciating that the authors used adjusted QCA measurements for stent sizing and optimisation rather than simply measured QCA.
It has previously been demonstrated that QCA underestimates MLD in small arteries and overestimates MLD in large arteries compared to IVUS (2). Based on this knowledge the authors used adjusted QCA to guide stent selection. Adjusted QCA was calculated as measured QCA + 10% for vessels ≤3.5mm, decreasing by 1% for every mm up to 4mm, in vessels ≥4mm adjusted QCA was calculated as measured QCA + 5%. Step-wise post-dilatation of the stent with non-compliant balloons was mandated to reach target diameters with a recommendation to use stent boost technology when available to ensure optimal expansion.
There were similar outcomes for all secondary outcomes in both groups with low rates of stent thrombosis overall. When analysed by subgroups there were no differences in QCA guided versus IVUS guided PCI. To date, there is no data available with regard to lesion complexity and the time taken to calculate QCA as well as adjusted QCA.
Evaluation of QCA requires appropriate angiographic views typically two orthogonal angles with semi-automation of the measurements.
Significant overlap of the coronary arteries or the presence of diffuse disease can impede QCA assessment. Therefore from the presentation alone, it is difficult to discern the generalisability of this trial.
The time to calculate QCA is dependent on operator experience may increase procedural time compared to IVUS. Furthermore, it will be of interest to understand if there were significant differences in the radiation doses as well as contrast use between groups. Ultimately there are a number of factors which have led to suboptimal uptake of IVUS in real-world clinical practice, whilst adjusted-QCA requires training if improved outcomes can be achieved in selected cases it may allow optimal IVUS utilisation, e.g. in diffuse disease, bifurcations or heavily calcified lesions, in resource-limited situations.
References
- Lee PH, Hong SJ, Kim HS, Yoon Y won, Lee JY, Oh SJ, et al. Quantitative coronary angiography versus intravascular ultrasound guidance for drug-eluting stent implantation (GUIDE-DES): study protocol for a randomised controlled non-inferiority trial. BMJ Open. 2022 Jan 1;12(1):e052215.
- Goto K, Mintz GS, Litherland C, Lansky AJ, Weisz G, McPherson JA, et al. Lumen Measurements From Quantitative Coronary Angiography and IVUS: A PROSPECT Substudy. JACC: Cardiovascular Imaging. 2016 Aug;9(8):1011–3.
Latest news from ESC Congress 2023






1 comment
Congratulation Nicola for the quality of your critical analysis This RCT demonstrated the non inferiority of adjudted QCA as compared to IVUS … Adjusted QCA requires adequate training and a systematic use in all PCI procedure in daily practice. With a correct training …. of course with the basic of adéquate orthogonal views for all lesion to be treated after systematic IC nitrate , the required time is no more matter of a limitation The cost - effectiveness is important ! This study demonstrate that IVUS is not required in routine and can be only used in selected cases to control results and/ or optimize results post PCI in very calcified lésions or edge dissection or LM bif… or others Thank you for your analysis Jean Marco