Preventive PCI or medical therapy alone for atherosclerotic coronary vulnerable plaques (PREVENT)
Reported from ACC.24
Ali Nazmi Calik provides his take on the results of the PREVENT trial presented at ACC.24 in Atlanta.
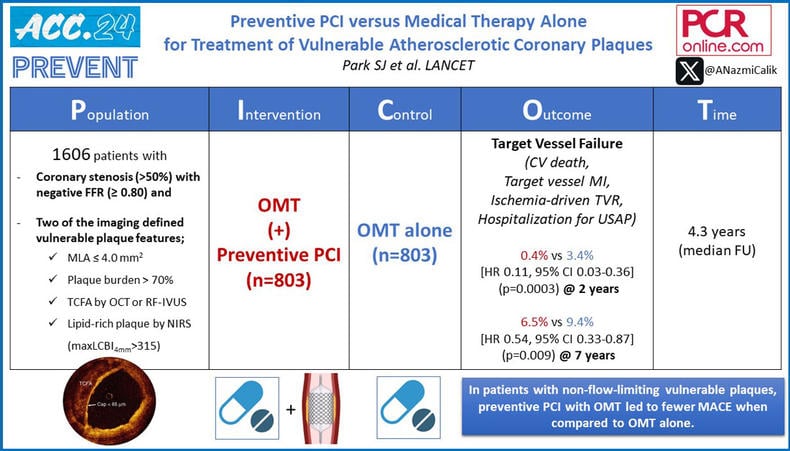
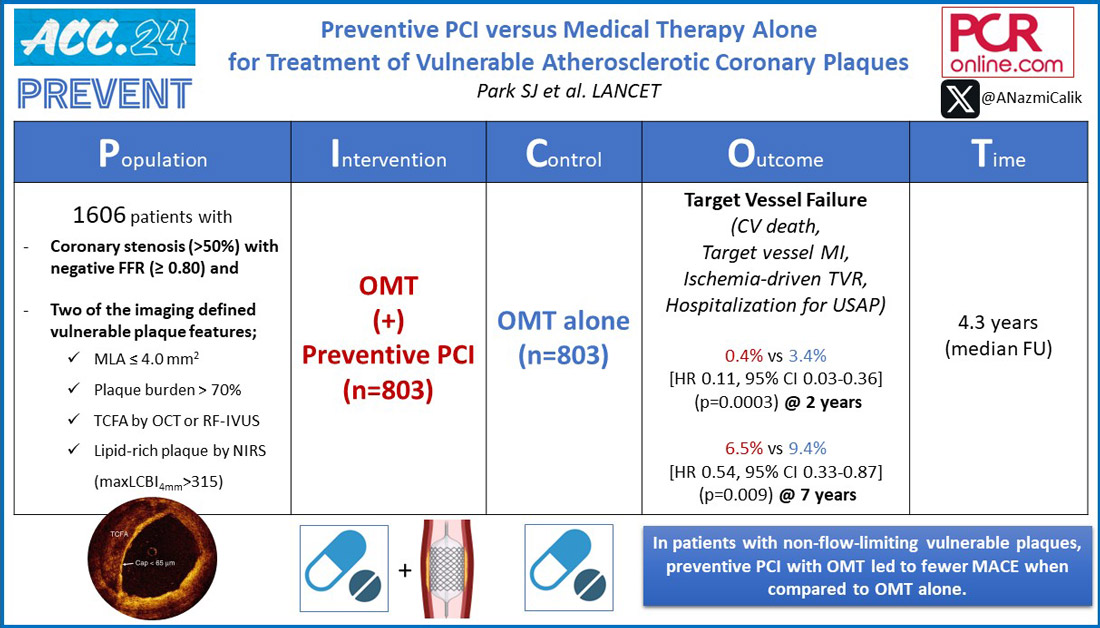
PICOT analysis of PREVENT - Courtesy of Ali Nazmi Calik - Source: PCRonline.com
Why this study – the rationale/objective?
The primary reason for acute coronary syndrome (ACS) and sudden cardiac death is often the rupture and thrombosis of lipid-rich atherosclerotic plaques in coronary arteries, commonly referred to as vulnerable plaques, which often appear mild on angiography and are often non-flow-limiting on haemodynamic assessment. (1-3) Nonetheless, by intravascular imaging, vulnerable plaques are recognized as thin-capped fibroatheromas consisting of a large plaque with a lipid-rich necrotic core, delineated from the artery's lumen by a thin fibrous cap. (4-6)
Despite the evident correlation between vulnerable plaques and an increased risk of adverse cardiovascular outcomes, whether revascularising non-flow-limiting (ie, non-ischaemic) vulnerable plaques is safe and effective is uncertain.
The PREVENT trial sought to assess the impact of preventive percutaneous coronary intervention (PCI) on major adverse cardiovascular events among patients presenting with high-risk, non-flow-limiting vulnerable plaques identified through intracoronary imaging.
How was it executed - the methodology
Following PCI of the culprit lesions in patients with ACS and chronic coronary syndrome (CCS), any untreated non-culprit lesions showing an angiographic diameter stenosis of 50% or more were evaluated for functionality using fractional flow reserve (FFR). Intermediate non-flow-limiting lesions (with an FFR > 0.80) were further analyzed using intracoronary imaging techniques such as grey-scale intravascular ultrasonography (IVUS), radiofrequency IVUS, a combination of grey-scale IVUS and near-infrared spectroscopy (NIRS), or optical coherence tomography (OCT), based on the discretion of experienced interventional cardiologists.
Vulnerable plaques were identified as lesions meeting at least two of the following criteria:
- Minimal lumen area (MLA) of less than 4.0 mm² by IVUS or OCT
- Plaque burden exceeding 70% by IVUS
- Presence of a lipid-rich plaque by NIRS ([maxLCBI4mm] >315)
- Thin-cap fibroatheroma (TCFA) detected by RF-IVUS or OCT
Eligible patients with one or two non-flow-limiting vulnerable plaques were randomly assigned 1:1 to either undergo PCI along with optimal medical therapy (OMT) or receive OMT alone. PCI of vulnerable plaques was performed with bioresorbable vascular scaffolds and cobalt-chromium everolimus-eluting metallic stents.
The primary outcome was a composite of death from cardiac causes, target-vessel myocardial infarction, ischaemia-driven target-vessel revascularisation, or hospitalisation for unstable or progressive angina, all at 2 years after randomisation.
Secondary outcomes were the individual components of the primary composite outcome, death from any cause, any myocardial infarctions, any revascularisation, definite stent or scaffold thrombosis, stroke, bleeding events, angına status, procedural complications, and the patient-oriented composite of all-cause death, all myocardial infarctions, or any repeat revascularisation.
What is the main result?
The investigator-initiated, multicentre, open-label, randomised controlled PREVENT study included 1606 randomly assigned patients with a total of 1672 qualifying lesions. Among them, 803 patients (with 831 lesions) were allocated to the preventive PCI plus OMT group, while 803 patients (with 841 lesions) were designated to receive OMT alone.
Baseline characteristics were similar between the groups. The median age was 65 years, with 429 (27%) women. Whereas 84% of patients had stable coronary artery disease, 12% had unstable angina, and 4% had experienced a recent myocardial infarction within one week.
The median FFR value of the 1672 target lesions was 0.86, with a mean diameter stenosis of 54.5%. Regarding the established criteria for plaque vulnerability per patient, 97% met the criterion of a MLA < 4.0 mm², 96% had a plaque burden > 70%, 11% had a maxLCBI4mm > 315, and 5% were identified as having TCFA.
At 2 years, the primary outcome occurred in three (0.4%) patients in the preventive PCI group and in 27 (3.4%) patients in the OMT group (HR 0.11, 95% CI 0.03-0.36, p=0.0003).
During a median follow-up of 4.3 years (maximum up to 7.9 years), patients who underwent PCI consistently exhibited a significantly reduced cumulative incidence of the composite primary endpoint, with a 46% lower risk observed throughout this timeframe (6.5% vs 9.4% ; HR 0.54, 95% CI 0.33-0.87, p=0.009).
Preventive PCI also reduced the composite patient-oriented risk of all-cause death, all myocardial infarctions, or any repeat revascularisation. (HR 0.69, 95% CI 0.50–0.95, p=0.022).
Furthermore, in the post-hoc as-treated analysis, the durability of preventive PCI seemed to be more sustained when using cobalt-chromium everolimus-eluting metallic stents compared to bioresorbable vascular scaffolds.
Critical reading and the relevance for clinical practice
In the PREVENT trial, the strategy of preventive PCI to treat vulnerable plaques resulted in a decrease in composite risk of death from cardiac causes, target-vessel myocardial infarction, ischemia-driven target-vessel revascularization, or hospitalization for unstable or progressive angina at the 2-year mark when compared to OMT alone. This reduction was evident across each component of the composite outcome and persisted throughout the 7-year follow-up period.
The rationale behind preventive PCI is to stabilize high-risk vulnerable plaques by allowing the necessary neointima to form over the stent or scaffold. This process helps to effectively thicken the fibrous cap, thereby decreasing the likelihood of plaque rupture. Demonstrated in a prior randomized trial that was not powered for clinical outcomes, preventive PCI on vulnerable plaques effectively expanded the coronary artery lumen, decreased plaque lipid content, and thickened the neointima compared to OMT alone. (7) In contrast, the preventive PCI strategy employed in the PREVENT trial, where patients in both groups received OMT and strict management of risk factors, decreased the risks of major cardiac events arising from vessels containing vulnerable plaques compared to OMT alone. These findings suggest that performing preventive PCI of non-flow-limiting high-risk vulnerable plaques could improve patient outcomes beyond the benefits achievable with OMT alone. Contrary to current clinical guidelines that advocate for PCI solely for flow-limiting lesions or those causing acute coronary syndromes, the results from PREVENT suggest potential expansion of PCI indications to include non-flow-limiting, high-risk vulnerable plaques.
It is important to consider several limitations of the trial when applying the results to daily practice. Despite the primary outcome rates being significantly lower than anticipated in both groups, the number of patients randomly assigned was adequate to demonstrate the benefits of preventive PCI based on the observed risk difference. A second limitation is that the study population was exclusively recruited from South Korea, Japan, Taiwan, and New Zealand, with only 27% of patients being women. This factor could potentially restrict the generalizability of the trial results. Another limitation is that the majority of patients in this trial had chronic coronary syndromes. It is worth noting that vulnerable plaques could be more prevalent and biologically dynamic in individuals with troponin-positive acute coronary syndromes. Another consideration regarding generalizability is the utilization of intracoronary imaging for identifying vulnerable plaques, which is not universally adopted as a global standard. Operators unfamiliar with using intracoronary imaging for real-time detection of vulnerable plaques may require specific training before incorporating this technique into practice.
In conclusion, in the PREVENT trial involving patients with non-flow-limiting vulnerable plaques, the combination of preventive PCI and optimal medical therapy led to reduced major adverse cardiac events over long-term follow-up compared to medical therapy alone. These findings offer new perspectives on the impact of preventive PCI on non-flow-limiting high-risk vulnerable plaques.
References
- Gaba P, Gersh BJ, Muller J, Narula J, Stone GW. Evolving concepts of the vulnerable atherosclerotic plaque and the vulnerable patient: implications for patient care and future research. Nat Rev Cardiol 2023; 20: 181–96.
- Kedhi E, Berta B, Roleder T, et al. Thin-cap fibroatheroma predicts clinical events in diabetic patients with normal fractional flow reserve: the COMBINE OCT-FFR trial. Eur Heart J 2021; 42: 4671–79.
- Mol JQ, Volleberg RHJA, Belkacemi A, et al. Fractional flow reserve- negative high-risk plaques and clinical outcomes after myocardial infarction. JAMA Cardiol 2023; 8: 1013–21.
- Stone GW, Maehara A, Lansky AJ, et al. A prospective natural- history study of coronary atherosclerosis. N Engl J Med 2011; 364: 226–35.
- Erlinge D, Maehara A, Ben-Yehuda O, et al. Identification of vulnerable plaques and patients by intracoronary near-infrared spectroscopy and ultrasound (PROSPECT II): a prospective natural history study. Lancet 2021; 397: 985–95.
- Prati F, Romagnoli E, Gatto L, et al. Relationship between coronary plaque morphology of the left anterior descending artery and 12 months clinical outcome: the CLIMA study. Eur Heart J 2020; 41: 383–91.
- Stone GW, Maehara A, Ali ZA, et al. Percutaneous coronary intervention for vulnerable coronary atherosclerotic plaque. J Am Coll Cardiol 2020; 76: 2289–30.




No comments yet!