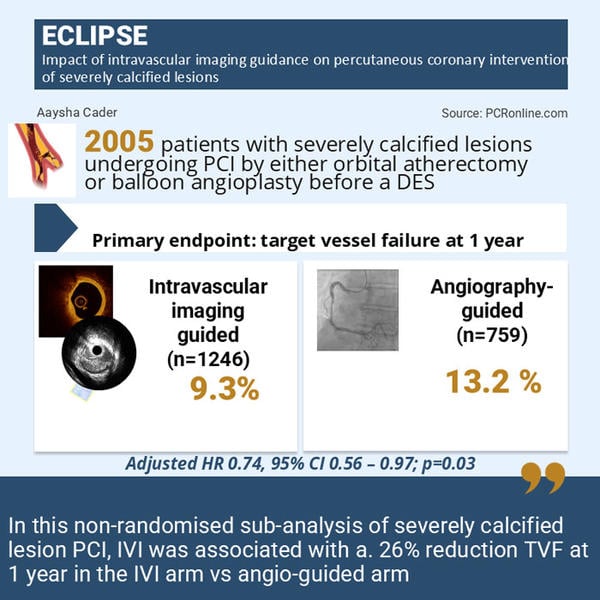
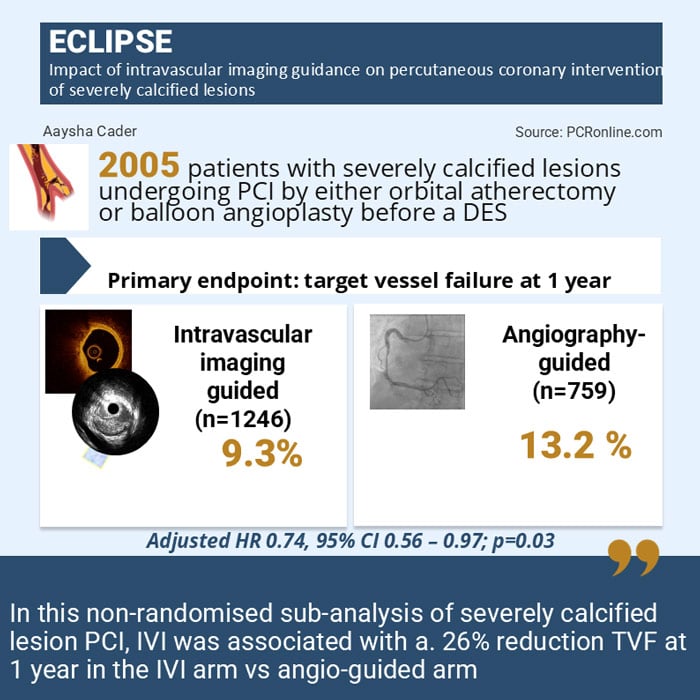
Impact of intravascular imaging guidance on percutaneous coronary intervention of severely calcified lesions: The ECLIPSE trial
Reported from ACC.25
Aaysha Cader provides her take on the ECLIPSE trial presented by Gregg W. Stone at ACC.25 in Chicago.
Designed by Aaysha Cader. Source: PCRonline.com
Why this study – the rationale/objective?
Severe coronary artery calcification is associated with increased procedural complexity, stent under-expansion, and adverse events. The multicentre, open-label randomised controlled ECLIPSE trial, initially presented at TCT 2024, found that orbital atherectomy (OA) before drug-eluting stent implantation did not increase minimal stent area (MSA) or reduce the rate of 1 year target vessel failure (TVF), as compared to balloon angioplasty (BA), in severely calcified lesions eligible for BA or OA as an initial strategy1,2.
In this sub-analysis of ECLIPSE presented at ACC 2025, investigators looked at the impact of intravascular imaging (IVI) on clinical outcomes during PCI of severely calcified lesions. This is especially relevant given the recent ESC chronic coronary syndromes guideline’s class 1A recommendation for IVI use to guide PCI of complex lesions which specified left main, true bifurcation and long lesions, but did not explicitly include calcified lesions3.
Methodology
The trial randomised 2,005 patients 1:1 to either OA vs BA as initial strategy before DES. Patients were prospectively enrolled in an OCT substudy in some sites, to characterise the effect of randomised treatment strategy on stent expansion. A final OCT sun recording MSA and other parameters was recorded in this group.
IVI sub-analysis
This non-randomised analysis of IVI vs angio-guided PCI was reported at ACC 2025. In the OA arm, a total of 1,008 patients were randomised. Among them, 627 (62.2 %) of them had IVI guidance (of whom 408 underwent OCT [of whom 276 were in OCT substudy], and 238 underwent IVUS), while 37.8 % had angiography guidance.
In the BA arm, a total of 997 were randomised, among whom 619 (62.1 %) had IVI guidance (of whom 411 underwent OCT [279 were in the OCT substudy] and 255 underwent IVUS), while 37.9 % had angiography guidance.
All patients who underwent IVI were pooled, totalling 1,241 (62.5 %); pooled angio-guided PCI patients were 759.
Endpoints
The two powered co-primary endpoints of the trial were 1) TVF at 1 year and 2) acute post-procedural MSA at the maximal calcification site, assessed by OCT in a pre-specified cohort of approximately 500 patients. In the imaging sub-analysis, the primary outcome analysed was 1 year TVF.
What is the main result?
There were 1,246 patients in the IVI-guided PCI group and 759 in the angiography-guided arm. Over 70 % were male. Over 96 % were severe calcifications across both arms.
Procedural characteristics:
Lesion length in mm (27.9 [18.5, 37.5] vs 23.5 [15.6, 33.1] and reference vessel diameter in mm (2.95 [2.67, 3.30] vs 2.86 [2.55, 3.19]) were both significantly greater in the IVI arm (p < 0.0001). Calcification length, minimal lumen diameter and diameter stenosis were similar. Greater use of wires, microcatheters, total contrast and longer fluoroscopy and radiation times were noted in the IVI arm (p < 0.0001).
Furthermore, the number of OA passes, predilatation balloons, specialty balloons, as well as number, total length and maximal stent diameters were all greater in the IVI arm.
Post-stent core lab characteristics:
Reference vessel diameter, acute gain and minimal lumen diameter were greater in the IVI arm.
Primary endpoint:
There was a 26 % reduction in the primary endpoint, TVF at 1 year in the IVI arm vs angio-guided arm (9.3 % vs 13.2 %, adjusted HR 0.74, 95 % CI 0.56 – 0.97; p = 0.03).
In only the OA arm, 1 year TVF was lesser with IVI guidance vs. angiography guidance alone (HR, 0.76, 95 % CI, 0.53 to 1.11 ). In the BA arm, 1 year TVF was lesser with IVI guidance vs. angiography guidance alone (HR, 0.62, 95 % CI, 0.42 to 0.93 ), Pinteraction = 0.48.
When comparing OCT vs IVUS, 1 year TVF was lesser in the OCT arm (12.2 % vs 7.7 %), although this difference was no longer significant after adjustment for differences in baseline clinical and angiographic characteristics (adjusted HR 0.78, p =0.24).
Critical reading and the relevance for clinical practice
This non-randomised analysis of ECLIPSE trial indicated that IVI guidance for calcified lesion PCI resulted in a 26 % reduction in the 1-year risk of TVF compared with angiography guidance alone, results of which were consistent in patients treated with OA and BA.
While these results might suggest that PCI for severely calcified lesions have better outcomes with IVI guidance, it is important to note that this analysis was not randomised (therefore unable to exclude residual confounding), and it is unclear if this analysis was pre-specified, and therefore the study was not designed to compare outcomes of IVI vs angio-guidance.
Furthermore, the OCT vs. IVUS comparison was under-powered to detect differences in outcomes and therefore one cannot extrapolate that OCT is better suited to guide calcified lesion PCI over IVUS.
Finally, it will be interesting to see results from the randomised OCT cohort beyond the post-procedural MSA, when they are reported.
References
- https://www.pcronline.com/News/Whats-new-on-PCRonline/2024/TCT/ECLIPSE-trial
- Kirtane AJ, Généreux P, Lewis B, Shlofmitz RA, Dohad S, Choudary J, et al; ECLIPSE Investigators. Orbital atherectomy versus balloon angioplasty before drug-eluting stent implantation in severely calcified lesions eligible for both treatment strategies (ECLIPSE): a multicentre, open-label, randomised trial. Lancet. 2025 Mar 28:S0140-6736(25)00450-7.
- Vrints C, Andreotti F, Koskinas KC, Rossello X, Adamo M, Ainslie J, et al; ESC Scientific Document Group. 2024 ESC Guidelines for the management of chronic coronary syndromes. Eur Heart J. 2024 Sep 29;45(36):3415-3537. doi: 10.1093/eurheartj/ehae177. Erratum in: Eur Heart J. 2025 Feb 21:ehaf079.
- Impact of intravascular imaging guidance on percutaneous coronary intervention of severely calcified lesions: The ECLIPSE trial. Presented at ACC 2025





No comments yet!