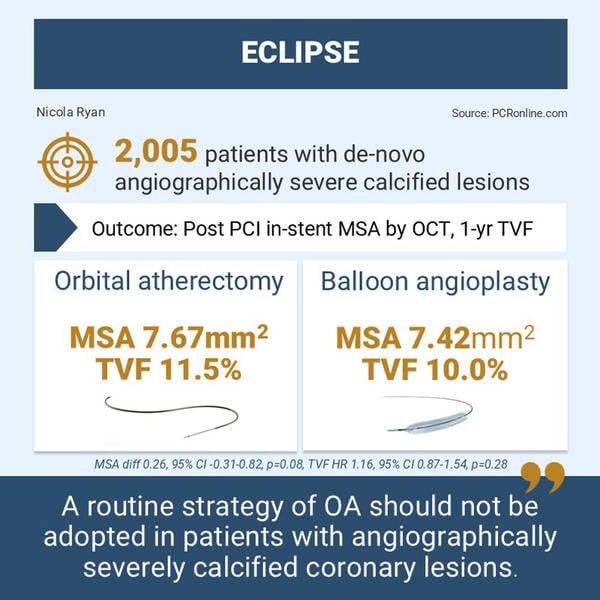
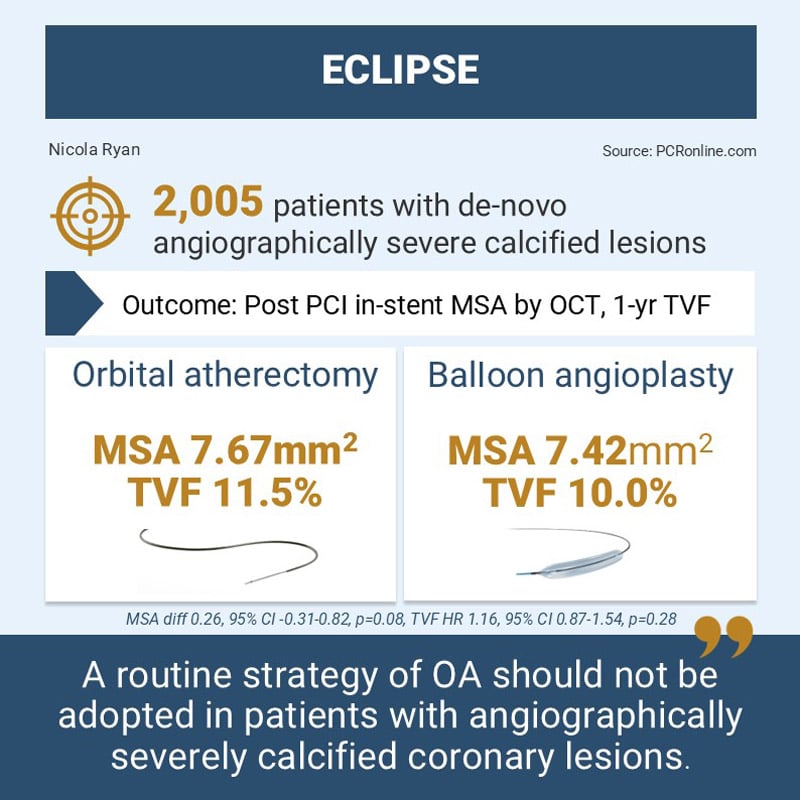
A large-scale, randomized trial of orbital atherectomy vs. conventional balloon angioplasty in severely calcified coronary arteries prior to DES implantation (ECLIPSE)
Reported from TCT 2024
Nicola Ryan provides her take on the ECLIPSE trial presented by Ajay J. Kirtane at TCT 2024 in Washington.
ECLIPSE compared orbital atherectomy with conventional balloon angioplasty in patients with calcified coronary lesions with clinical equipoise for either strategy.
Why this study – the rationale/objective?
Coronary calcium is increasingly encountered in clinical practice and is associated with increased PCI complexity. Worse immediate and long-term angiographic and clinical outcomes are observed in patients with severely calcified lesion. Orbital atherectomy (OA) allows optimal lesion preparation by ablating and fracturing calcium, allowing adequate stent expansion. In balloon un-crossable or non-dilatable coronary lesions, orbital atherectomy allows stent delivery and expansion. The additional benefit of orbital atherectomy in calcified coronary lesions with equipoise for the use of conventional balloon dilatation (BA) is unknown.
How was it executed – the methodology?
Patients with de novo severely calcified lesions as assessed by angiography; opacities without cardiac motion involving both sides of the wall with a total calcium ≥ 15 mm extending into the lesion, or by OCT or IVUS; ≥ 270° calcium in ≥ 1 cross-section were eligible for inclusion, if they were deemed to have clinical equipoise for either orbital atherectomy or balloon angioplasty.
In the orbital atherectomy arm, a 1.25 mm burr was used with a mandatory balloon dilatation post-atherectomy, pre-stent implantation. Post-dilatation was mandatory with a 1:1 balloon at ≥ 18 ATM. In the balloon angioplasty arm, cutting and scoring balloons were permitted but not IVL. An OCT sub-study was included within the trial.
The primary endpoints were:
- Post PCI in-stent MSA by OCT (OCT sub-study group)
- 1-year TVF
The secondary endpoints were:
- Procedural success – stent implantation with ≤ 20 % residual stenosis and no major complications
- Strategy success – procedural success without crossover
What is the main result?
Overall 2,005 patients were enrolled, 1,008 randomised to the orbital atherectomy arm, and 997 to balloon angioplasty. In the OCT cohort, there were 825 potentially eligible patients, of whom 555 had evaluable OCT, 276 patients, 286 lesions in the OA arm and 279 patients, 292 lesions in the BA arm. The majority of patients were male, with a mean age of 69 years, and traditional cardiovascular risk factors were common. Notable approximately 5.5 % of the population were on haemodialysis. The majority of lesions were in the LAD, and slightly under a third were bifurcations or trifurcations. The mean core lab assessed percent diameter stenosis was 67 % in both arms. Overall, there was a high rate of femoral access (47 %) and intravascular imaging was performed in approximately 62 % of cases well balanced between groups.
- There was no difference in the MSA between groups (OA 7.67 ± 2.27 vs. BA 7.42 ± 2.54, diff 0.26, 95 % CI -0.31-0.82, p = 0.08).
- At one year, TVF did not differ between groups (OA 11.5 % vs. BA 10.0 %, HR 1.16, 95 % CI 0.87-1.54, p = 0.28)
- Both procedural success (OA 85.5 % vs BA 86.1 %, p = 0.71) and strategy success (OA 84.0 % vs. BA 82.8 %, p = 0.49) were similar with orbital atherectomy and balloon angioplasty.
Critical reading and the relevance for clinical practice
The ECLIPSE trial demonstrated that, in patients with calcified coronary lesions and equipoise for the use of orbital atherectomy or conventional balloon angioplasty, orbital atherectomy did not improve MSA or TVF at one-year follow-up.
Prior studies of calcium debulking are based on the use of rotational atherectomy (RA) and demonstrated significantly higher crossover rates than those observed in ECLIPSE. In PREPARE-CALC, 16 % crossed over from balloon modification (cutting or scoring balloon) to RA, and 12.5 % from BA to RA in ROTAXUS, compared to 4.9 % in ECLIPSE. This likely reflects the patient population included in the trials as the mean diameter stenosis by QCA was 67 % in ECLIPSE, compared to 80 % in ROTA-TAXUS, and 83 % in PREPARE-CALC. ROTA-TAXUS and PREPARE-CALC both demonstrated a higher strategy success with RA compared to BA, which was not demonstrated in ECLIPSE, again likely representing the population enrolled in the trial.
The MSA in ECLIPSE was large at > 7.4 mm2 in both arms, which is a predictor of improved clinical outcomes, suggesting that optimal plaque preparation was achieved in both arms. In the balloon angioplasty arm, there were relatively low rates of use of both cutting (10.1 %) and scoring (11.0 %), with the majority of patients treated with conventional balloons, again suggesting the calcium was amenable to treatment with conventional balloons. Overall procedural complications were low with increased slow flow (1.4 % vs. 0.4 %, p = 0.03) in the OA arm and numerically but not statistically higher perforations with OA. At thirty days, there was a higher rate of cardiac death in the OA arm, with 2 deaths adjudicated as attributable to the device, and 2 as possibly attributable to the device. At one year, there were no differences in clinical outcomes.
Whilst intravascular imaging was not mandated within the trial, there was a high rate of imaging both OCT and IVUS, although not an initial powered endpoint when TVF was stratified by OCT cohort there was a reduction in TVF in the OCT cohort (OCT cohort 7.2 % vs non-OCT cohort 12.2 %, HR 0.57, 95 % CI 0.4-0.81, p = 0.0016, adj HR 0.68, 95 %CI 0.55-0.84, p = 0.0003). Given that the trial failed to meet its primary endpoint, this can only be hypothesis generating but supports the overall body of evidence that use of intracoronary imaging in calcified lesions improves outcomes.
The results of the ECLIPSE trial suggest that a routine strategy of OA should not be adopted in patients with angiographically severely calcified coronary lesions. The overall high rates on intracoronary imaging and improved outcomes in the imaging cohort adds weight to the recommendation for imaging guided PCI in patients with calcified coronary disease. A strategy of careful assessment of plaque characteristics and choosing the most appropriate tool to achieve optimal plaque preparation prior to implantation of stents is likely to give the best long-term outcomes.





No comments yet!