In-Stent CTO percutaneous coronary intervention: individual patient data pooled analysis of 4 multicenter registries
Selected in JACC: Cardiovascular Interventions by N. Ryan
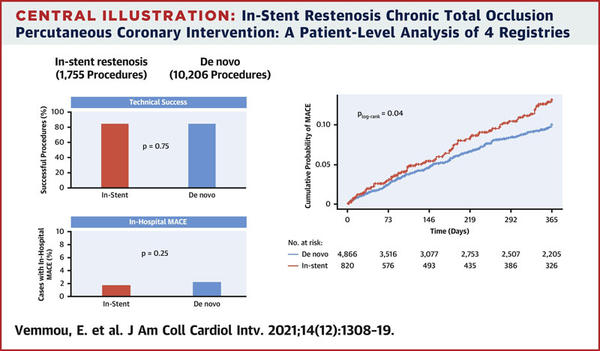
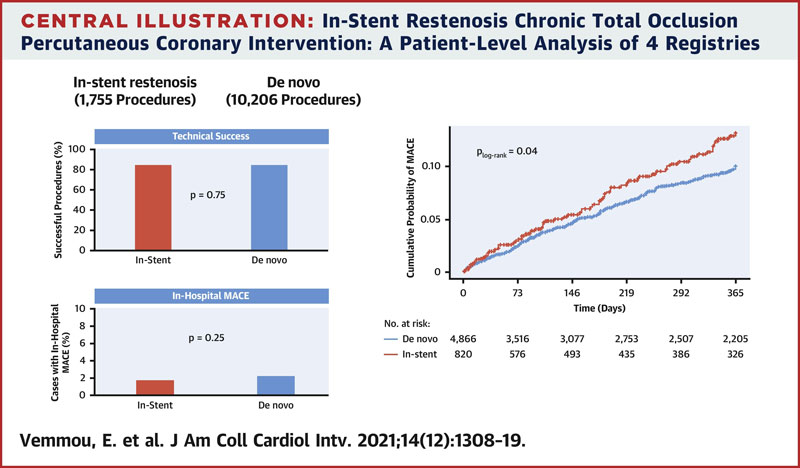
This analysis highlights that, in appropriate hands, ISR CTO-PCI is safe, with similar success rates to de-novo CTO-PCI.
References
Authors
Evangelia Vemmou, Alexandre S. Quadros, Joseph A. Dens, Nidal Abi Rafeh, Pierfrancesco Agostoni, Khaldoon Alaswad, Alexandre Avran, Karlyse C. Belli, Mauro Carlino, James W. Choi, Ahmed El-Guindy, Farouc A. Jaffer, Dimitri Karmpaliotis, Jaikirshan J. Khatri, Dmitrii Khelimskii, Paul Knaapen, Alessio La Manna, Oleg Krestyaninov, Pablo Lamelas, Soledad Ojeda, Lucio Padilla, Manuel Pan, Pedro Piccaro de Oliveira, Stéphane Rinfret, James C. Spratt, Masaki Tanabe, Simon Walsh, Ilias Nikolakopoulos, Judit Karacsonyi, Bavana V. Rangan, Emmanouil S. Brilakis, and Lorenzo Azzalini
Reference
J Am Coll Cardiol Intv. 2021 Jun, 14 (12) 1308–1319
Published
June,14 2021
Link
Read the abstractReviewer
Latest contributions
Balloon lithotripsy added to conventional preparation before stent implantation in severely calcified coronary lesions Impact of pullback pressure gradient on clinical outcomes after percutaneous coronary interventions Validation of intravascular ultrasound-defined optimal stent expansion criteria for favorable 1-year clinical outcomesMy Comment
Why this study? – the rationale/objective
Depending on the study, PCI of in-stent restenosis chronic total occlusions (ISR CTO) comprise 5-25 % of all CTO-PCI’s. There are specific technical challenges associated with ISR CTO-PCI, including maintaining an intrastent track, poor distal runoff, associated with long stented segments, difficulties re-entering if the wire is sub-stent, and high rates of restenosis.
Historically, poorer outcomes were reported with ISR CTO-PCI; however, more recent studies suggest success rates similar to de-novo CTO-PCI.
This study combined individual patient-level data from four international registries to examine the outcomes of ISR CTO-PCI.
How was it executed? – the methodology
A patient-level pooled analysis of 11,961 CTO PCIs performed in 11,728 patients from 107 centers between 2012 and 2020 was carried out. The included registries were PROGRESS-CTO (6,683 procedures), LATAM (1,700 procedures), RECHARGE (1,308 procedures), and a 7-centre registry from Italy, Belgium, Japan, Spain, Canada, and the United States (2,270 procedures).
- In-stent CTOs were defined as occlusions at the stent, or within 5 mm proximal or distal to the stent.
- Procedural success was defined as technical success without any in-hospital MACE (death, MI, tamponade requiring pericardiocentesis or surgery and stroke)
- One-year MACE was defined as the composite of all-cause death, MI, or TVR at 12-month follow-up
What is the main result?
Overall, 1,755 ISR CTO-PCI procedures were carried out in 1,727 patients (14.7 % of all CTO-PCI’s). Patients undergoing ISR CTO-PCI had a higher prevalence of traditional cardiovascular risk factors including diabetes, hypertension, and hyperlipidaemia, as well as increased prior MI (57.1 % vs 42 %, p < 0.0001) and CABG (26.5 % vs. 24 %, p = 0.0275). Long-term follow-up was available in 5,701 patients (48.6 % of the population), with a median duration of follow-up of 306 days (IQR 57 to 365 days).
- There were no differences in the vessel attempted; however, radial access was less common in the ISR group (42.6 % vs. 49.6 %, p < 0.0001).
- Mean J-CTO score was higher in the ISR group (2.32 ± 1.26 vs. 2.22 ± 1.27, p = 0.0111) with interventional collaterals less common in the ISR group (55.9 % vs. 62.2 % p < 0.0001). De-novo CTOs more commonly had moderate to severe calcification (48.3 % vs 35.6 %, p < 0.001) and proximal cap ambiguity (36.2 % vs 26.8 %, p < 0.0001).
- Anterograde wiring was the most commonly used strategy (ISR 84.8 % vs. 81 % p = 0.0002) with ADR (25.3 % vs 26.4 %, p = 0.302) and retrograde techniques (26.2 % vs 36 %, p < 0.0001) less commonly used in ISR CTO PCI.
- Intravascular imaging was more commonly used in the ISR group (40.5 % vs 32.7 %, p < 0.001)
- There were no significant differences in technical success (84.9 % vs. 85.2 %, p = 0.75), procedural success (83.7 % vs. 83.9 %, p = 0.82), and in-hospital MACE (1.7 % vs. 2.2 %, p = 0.25) between the groups.
- At 12-month follow-up MACE ( HR 1.31 95 % CI 1.01-1.70, p = 0.04) and TVR (HR 1.34 95 % CI 1.00-1.81, p = 0.005) were higher in the ISR group with similar rates of MI (HR 1.5 95 % CI 0.78-2.9, p = 0.23) and death (HR 1.30, 95 %CI 0.74-2.26, p = 0.36).
Source: JACC Cardiovascular Interventions
Critical reading and the relevance for clinical practice
The results of this analysis suggest that ISR CTO-PCI, carried out by high volume dedicated CTO-PCI operators, has similar success and in-hospital MACE rates to de-novo CTO-PCI. There were important differences in the successful crossing technique with anterograde wiring, most commonly successful in both groups, and more commonly used in ISR CTO-PCI. The decreased use of retrograde techniques is likely, in part, explained by the reduced incidence of interventional collaterals in the ISR groups compared to the de-novo CTO group.
Overall, the MACE was higher in the ISR subgroup mainly driven by increased TVR. The ISR CTO group had an increased incidence of CVRF particularly diabetes mellitus as well as increased MI, CABG, and peripheral artery disease. All of these factors are associated with increased overall ISR and likely reflect a more aggressive atherosclerotic plaque subtype.
The use of intravascular imaging was low in both the ISR and de-novo CTO arms, likely reflecting local practice and reimbursement. Furthermore, there is no information available with regard to intravascular imaging findings. This requires further examination, particularly in the ISR group, as understanding the mechanism of stent failure potentially influences treatment strategies as well as optimise the PCI outcomes. A small retrospective single centre Korean study has shown no differences in outcomes with IVUS guided CTO PCI up to 5 years in patients with ISR versus de-novo CTO1.
A note of caution when interpreting the results, long-term follow-up was available for under half of the population. All procedures were carried out by high volume dedicated CTO-PCI operators, therefore the procedural and technical success rates may not be generalisable to non-CTO-PCI operators. Information with regard to diabetic control and medical therapy is not available, given the higher risk of restenosis in patients with diabetes and CABG, this is of interest.
This analysis highlights that, in appropriate hands, ISR CTO-PCI is safe, with similar success rates to de-novo CTO-PCI. Given the increased MACE at one-year driven mainly by TVR, further emphasis needs to be placed on optimisation of ISR CTO procedures, including the use of intravascular imaging and optimal medical therapy to control CVRF.
References
- Yoon Y-H, Lee P, Lee S-W, Kwon O, Lee K, Kang D-Y, et al. Clinical outcomes after percutaneous coronary intervention for in-stent chronic total occlusion [Internet]. EuroIntervention. [cited 2021 Jul 4]. Available from: https://eurointervention.pcronline.com/article/importance-of-stent-optimization-for-favourable-outcomes-after-percutaneous-coronary-intervention-for-chronic-in-stent-occlusions




No comments yet!