Operator volumes and in-hospital outcomes: an analysis of 7,740 rotational atherectomy procedures from the BCIS national database
Selected in JACC: Cardiovascular Interventions by N. Ryan
Find out more about the results of this analysis which suggest that operator experience may be an important effect modifier in ROTA-PCI.
References
Authors
Tim Kinnaird, Sean Gallagher, Andrew Sharp, Majd Protty, Tariq Salim, Peter Ludman, Samuel Copt, Nick Curzen, and Mamas A. Mamas
Reference
10.1016/j.jcin.2021.04.034
Published
June 16, 2021
Link
Read the abstractReviewer
Latest contributions
Balloon lithotripsy added to conventional preparation before stent implantation in severely calcified coronary lesions Impact of pullback pressure gradient on clinical outcomes after percutaneous coronary interventions Validation of intravascular ultrasound-defined optimal stent expansion criteria for favorable 1-year clinical outcomesMy Comment
Why this study? – the rationale/objective
Overall, there does not appear to be an association between operator volume and unselected PCI outcomes. However, in certain complex high-risk procedures, such as CTO-PCI and LMS-PCI, higher volume operators have better outcomes.
Rotational atherectomy during PCI (ROTA-PCI) is technically challenging with numerous factors influencing outcomes.
To date, the relationship between ROTA-PCI volume and patient outcomes has not been well defined.
How was it executed? – the methodology
The British Cardiovascular Intervention Society (BCIS) PCI database was analyzed for all ROTA-PCI procedures carried out from 2013 to 2016, the period for which the number of procedures per operator was available.
- The outcomes of interest were in-hospital mortality, in-hospital MACCE (death, MI, CVA), in-hospital bleeding, emergency CABG or repeat PCI, acute coronary procedural complications (no flow, perforation, dissection, and major side-branch loss).
- Operators were divided into 4 quartiles (Q) categorized by annualized average operator ROTA-PCI volume, with a median number of ROTA-PCI procedures per year of 1 (Q1), 6.75 (Q2), 11.5 (Q3), 16 (Q4).
- Individual logistic regressions were performed to quantify the independent association between annual operator ROTA-PCI volume and in-hospital patient outcomes.
What is the main result?
Overall, 7,740 ROTA-PCI procedures were carried out over the four-year period, with a median operator volume of 2.5 procedures / year (range 0.25-55.25). In the wider 2006-2016 period, the ROTA-PCI increased from 0.7 % of all PCI procedures in 2006 to 2.4 % in 2016, p <0.001.
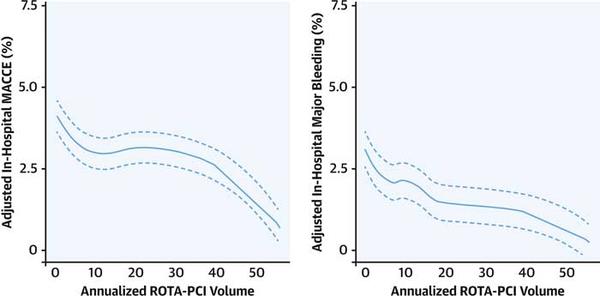
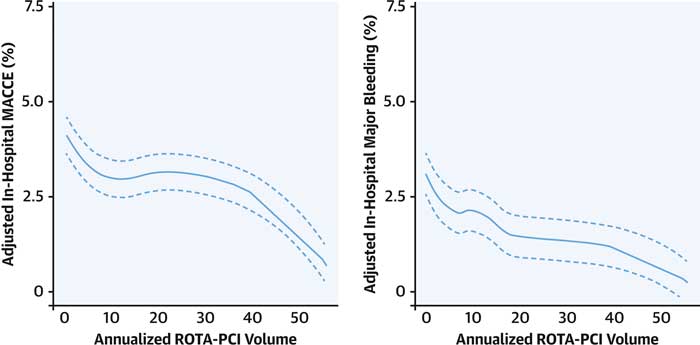
- There was an inverse relationship between operator ROTA-PCI volume and in-hospital mortality (OR 0.986 / case 95 % CI 0.975-0.996, p = 0.007) and MACCE (OR 0.983 / case 95 % CI 0.975-0.993, p < 0.001)
- An annual volume of < 4 ROTA-PCI procedures / year was associated with increased MACCE (p < 0.005); over half of operators (55 %) did not exceed this threshold
- Lower rates of emergency cardiac surgery (OR 0.964 / case, 95 % CI 0.939-0.991, p = 0.0080), arterial complications (OR 0.975 / case, 95 % CI 0.975-0.982, p < 0.001) and in-hospital major bleeding (OR 0.985 / case, 95 % CI 0.977-0.993, p < 0.001) were seen with higher volume ROTA-PCI operators
- Higher volume operators undertook more complex procedures with more vessels and lesions treated (p < 0.001), were more likely to treat the LMS (p < 0.001), and use intravascular imaging (p < 0.001), and less likely to use femoral access (p < 0.001)
Source: JACC Cardiovascular Interventions
Critical reading and the relevance for clinical practice:
The results of this analysis suggest that operator experience may be an important effect modifier in ROTA-PCI. ROTA-PCI is generally used in more complex calcific anatomy therefore even the placement of the guidewire more challenging and procedural complications more frequent than in PCI without rotational atherectomy, operator experience can be an important factor in resolving these complications. Important differences were seen in both in-hospital MACCE as well as in-hospital major bleeding with increased operator experience. Experienced operators less commonly used femoral access, suggesting that procedural planning and appropriate access site selection may reduce bleeding complications.
Of note: in this unselected analysis, approximately 40 % of all ROTA-PCI cases were carried out in the context of an acute coronary syndrome. The relationship between operator volume and MACCE was modified by ACS (p for interaction 0.033). Over half of all operators did not carry out > 4 cases / year, which was associated with decreased MACE; this highlights the need for appropriate procedural planning in ACS-PCI, as well as the organization of ACS services to allow either support from a more experienced colleague or transfer to a centre with appropriate procedural expertise.
A note of caution when interpreting the results: this analysis was carried out in a single country, where the median operator volume is 178 procedures / year, which must be considered when generalising the outcomes to countries with lower procedural volumes. Furthermore, information regarding lifetime operator experience as well as ROTA-PCI experience was not available.
Given the aging population, as well as increased number of patients presenting with complex calcific disease, rotational atherectomy is an important tool in ensuring adequate plaque preparation and optimal stent implantation. This analysis highlights that in ROTA-PCI operator experience influences patient outcomes, therefore it is imperative that operators work in a collegiate fashion to ensure optimal patient outcomes.






No comments yet!