23 Aug 2021
Stent expansion indexes to predict clinical outcomes: an IVUS substudy from ADAPT-DES
Selected in JACC Cardiovascular Interventions by S. Brugaletta
The purpose of the present investigation was to revisit all stent expansion indexes to identify the best predictor of 2-year percutaneous coronary intervention (PCI) lesion-specific outcome measures (i.e. clinically-driven target lesion revascularization [TLR] or definite stent thrombosis) using the ADAPT-DES IVUS substudy cohort.
References
Authors
Tatsuhiro Fujimura, Mitsuaki Matsumura, Bernhard Witzenbichler, D. Christopher Metzger, Michael J. Rinaldi, Peter L. Duffy, Giora Weisz, Thomas D. Stuckey, Ziad A. Ali, Zhipeng Zhou, Gary S. Mintz, Gregg W. Stone, and Akiko Maehara
Reference
J Am Coll Cardiol Intv. 2021 Aug, 14 (15) 1639–1650
Published
August,14 2021
Link
Read the abstractReviewer
My Comment
Why this study? – the rationale/objective
Numerous prior IVUS or optical coherence tomographic studies have shown absolute minimum stent area (MSA) to be the most powerful predictor of future adverse events, including stent thrombosis and restenosis. However, an achievable MSA is limited by vessel size; thus, any single absolute cutoff of MSA to predict adverse events may fail when extrapolated to different populations.
The purpose of the present investigation was to revisit all stent expansion indexes to identify the best predictor of 2-year percutaneous coronary intervention (PCI) lesion-specific outcome measures (i.e. clinically-driven target lesion revascularization [TLR] or definite stent thrombosis) using the ADAPT-DES IVUS substudy cohort.
How was it executed? – the methodology
ADAPT-DES (Assessment of Dual Antiplatelet Therapy With Drug-Eluting Stents) was a prospective, multi-center registry of 8,582 patients undergoing percutaneous coronary intervention (PCI) with drug-eluting stents. Native coronary artery lesions treated with IVUS-guided PCI with final analyzable IVUS were included. Ten stent expansion indexes (MSA, MSA/vessel area at MSA site, conventional stent expansion [MSA/average of proximal and distal reference luminal area], minimum stent expansion using Huo-Kassab or linear model accounting for vessel tapering, stent asymmetry [minimum/maximum stent diameter within the entire stent], stent eccentricity [smallest minimum/maximum stent diameter at a single slice within the stent], IVUS-XPL [Impact of intravascular Ultrasound Guidance on Outcomes of Xience Prime Stents in Long Lesions] criteria, ULTIMATE [Intravascular Ultrasound-Guided Drug-Eluting Stents Implantation in “All-Comers” Coronary Lesions] criteria, and ILUMIEN IV criteria) were evaluated for their associations with lesion-specific 2-year clinically-driven target lesion revascularization (TLR) or definite stent thrombosis.
What is the main result?
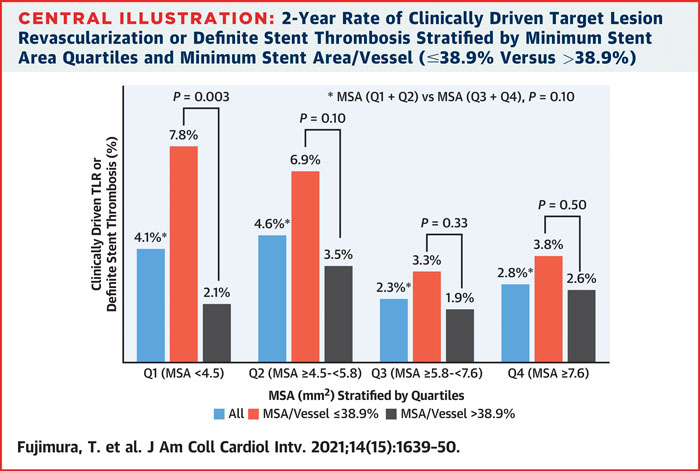
Overall, 2,140 lesions in 1,831 patients were included; final MSA measured 6.2 +/- 2.4 mm2. Among the 10 stent expansion indexes, only MSA/vessel area at the MSA site was independently associated with 2-year clinically driven TLR or definite stent thrombosis (hazard ratio: 0.77; 95 % confidence interval: 0.59-0.99; P = 0.04) after adjusting for morphologic and procedural parameters.

Source: JACC Cardiovascular Interventions
Critical reading and the relevance for clinical practice
In this IVUS-guided PCI cohort with excellent final MSA overall, stent/vessel area at the MSA site, an index of relative stent expansion, was superior to absolute MSA and other expansion indexes in predicting 2-year clinically driven TLR or definite stent thrombosis.
In our daily practice, imaging in PCI is underused, most of the time because it is time-consuming and measurement of parameters is not easy for those who are not trained to. The present paper, by identifying only one parameter, may help to have wider use of imaging techniques for PCI optimization. We should consider that nowadays, we may optimize our PCI outcome, not by using a specific stent platform instead of another (they are all at the same level of efficacy with a currently low margin of improvement), but instead by analyzing an IVUS or OCT pullback in order to have a correct stent expansion and apposition.
It would be nice to have the same analysis, as done in this paper, also for OCT.
The use of artificial intelligence in imaging software may help interventional cardiologists in incorporating these techniques into their daily practice.
In which percentage of PCI do you routinely use intracoronary imaging techniques?






1 comment
45%