2-year outcomes of angiographic quantitative flow ratio-guided coronary interventions
Selected in JACC by N. Ryan
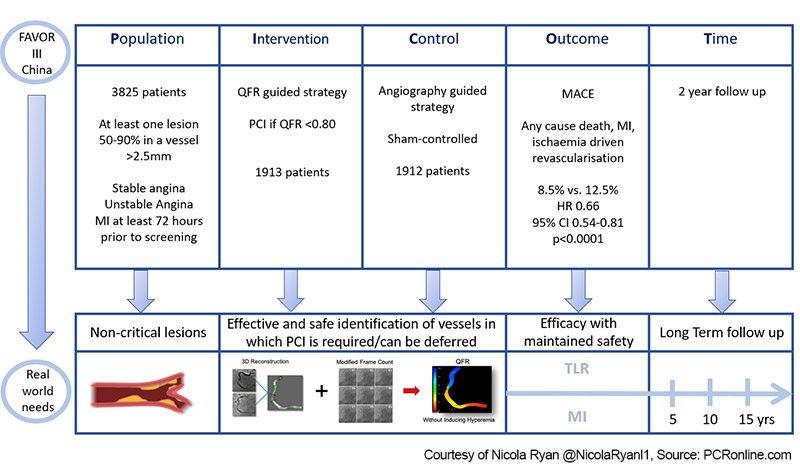
FAVOR-III China was an investigator-initiated, multicentre, randomised, blinded, sham-controlled trial comparing clinical outcomes of QFR versus angiography-guided strategies for the treatment of non-critical lesions in patients with stable or unstable angina, or MI, at least 72 hours prior to screening. The one-year results showed improved clinical outcomes with QFR-guided lesion selection1. Here, the authors report the 2-year outcomes.
References
Authors
Lei Song, Bo Xu, Shengxian Tu, Changdong Guan, Zening Jin, Bo Yu, Guosheng Fu, Yujie Zhou, Jian’an Wang, Yundai Chen, Jun Pu, Lianglong Chen, Xinkai Qu, Junqing Yang, Xuebo Liu, Lijun Guo, Chengxing Shen, Yaojun Zhang, Qi Zhang, Hongwei Pan, Rui Zhang, Jian Liu, Yanyan Zhao, Yang Wang, Kefei Dou, Ajay J. Kirtane, Yongjian Wu, William Wijns, Weixian Yang, Martin B. Leon, Shubin Qiao, Gregg W. Stone, and on behalf of the FAVOR III China Study Group
Reference
J Am Coll Cardiol. 2022 Nov, 80 (22) 2089–2101
Published
November 2022
Link
Read the abstract
Reviewer
Latest contributions
Balloon lithotripsy added to conventional preparation before stent implantation in severely calcified coronary lesions Impact of pullback pressure gradient on clinical outcomes after percutaneous coronary interventions Validation of intravascular ultrasound-defined optimal stent expansion criteria for favorable 1-year clinical outcomesMy Comment
PICOT Scheme - Courtesy of Nicola Ryan @NicolaRyanl1, Source: PCRonline.com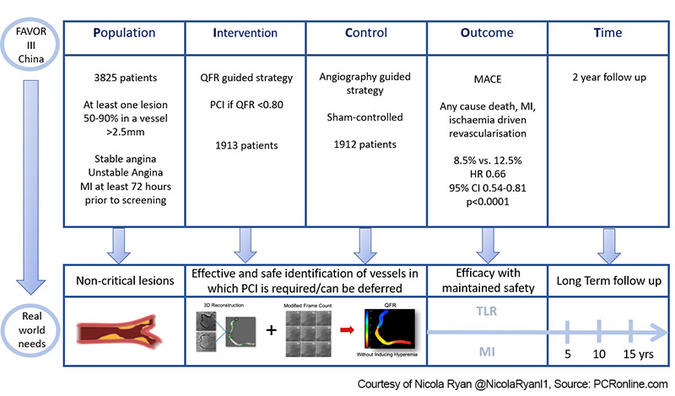
Why this study – the rationale/objective?
Invasive wire-based physiological assessment has been shown to more accurately identify flow-limiting lesions than angiography alone2.
Despite the guideline recommendation for invasive physiological assessment, its use in real-world clinical practice is limited3.
Quantitative flow ratio (QFR) uses 3D coronary reconstruction and computational fluid dynamics to estimate FFR based on angiography alone4.
The one-year results of FAVOR III China showed improved clinical outcomes with QFR-guided lesion selection compared to angiography alone1.
It is of interest to understand if these improved outcomes persisted in the longer term.
How was it executed? - the methodology
From December 2018 to January 2020, patients presenting with stable or unstable angina, or MI, at least 72 hours prior to screening, with at least one 50-90 % stenosis in a vessel ≥ 2.5 mm diameter at coronary angiography were randomised (1:1) to QFR guided versus angiography-guided revascularisation.
Exclusion criteria included significant vessel tortuosity or overlap not amenable to QFR and renal impairment (eGFR < 45 ml l/kg/1·73 m2). Clinicians declared their intended treatment strategy for all lesions prior to randomisation. There was a pre-set 10-minute delay for real or sham QFR calculation prior to PCI. PCI was performed in lesions with QFR < 0.80 and deferred with a QFR > 0.80 in the QFR group. Participants and clinical assessors were blinded to treatment outcomes.
- The primary endpoints were reported in the one-year outcomes paper1.
- MACE and its components at 2 years was a secondary endpoint.
What is the main result?
Overall, 3,847 patients from 26 sites in China were enrolled in the trial. Following withdrawal of consent, 1,913 randomised to QFR-guided revascularisation and 1,912 randomised to angiography-guided revascularisation were included in the ITT analysis.
The majority of participants were men (70.6 %), with a mean age of 62.7 ± 10.1 years. The most common clinical presentation was ACS (63.5 %) with a third of patients diabetic. The majority of patients had single vessel CAD (46.5 % vs. 45.4%), with approximately 50 % of lesions in the LAD. Mean QFR calculation time was 3.9 ± 1.4min. Two year follow-up was available in 98.3 % of patients (98.5% QFR arm 98.1 % control).
- QFR changed treatment strategy in 23.3 % of patients (deferral 19.6 %, treatment of a vessel not initially planned for treatment 4.4 %), whilst the initial strategy was changed in 6.2 % of the angiographic group (deferral 5.2 %, treatment of a vessel not initially planned for treatment 1.5 %).
- Higher rates of functionally complete revascularisation (post-PCI QFR assessment) were achieved in the QFR-guided group (88.1 % vs. 82.2 %).
- MACE at two years was lower in the QFR arm (8.5 % vs. 12.5 %, HR 0.66, 95 % CI 0.54-0.81, p < 0.001)
- Excluding periprocedural MI, MACE remained lower in the QFR-guided arm (5.8 % vs. 8.8 %, HR 0.65, 95 % CI 0.51-0.833, p = 0.0004).
- Both MI (4.0 % vs. 6.8 % HR 0.58, 95 % CI 0.44-0.77, p = 0.0002) and ischaemia driven revascularisation (4.2 % vs 5.8 %, HR 0.72, 95 % CI 0.53-0.95, p = 0.02) were lower with a QFR guided strategy.
- There was a greater relative reduction in MACE in those in whom the strategy changed with QFR guidance (p for interaction = 0.009).
Critical reading and the relevance for clinical practice
The results of this investigator-initiated multicentre randomised blinded, sham-controlled trial showed that a QFR-guided strategy remains superior to an angiography-guided strategy in terms of clinical outcomes at two years. Overall, a QFR-guided strategy lead to a significant reduction in MACE at two years driven by reduced MI and ischaemia-driven revascularisation with no significant differences in mortality. The benefit of a QFR strategy continued over time with a reduction in relative hazard between both 0-1 years and 1-2 years post-procedure.
Based on QFR, the revascularisation strategy changed for almost a quarter of patients. Importantly, the greatest benefit in terms of reduced MACE was derived by those patients in whom QFR changed the revascularisation strategy, and outcomes were also improved in those patients who underwent QFR concordant treatment compared to those in whom treatment was discordant with QFR (8.8 % vs 17.2 %, p < 0.0001). In the QFR-guided group, 375 patients had at least one lesion deferred. In terms of outcomes in this group, there where 6 non-periprocedural MI’s, 3 (0.8 %) related to a deferred vessel, and 2 (0.5 %) were related to a stented vessel. Of the ischaemia-driven revascularisation in group where QFR lead to at least one lesion being deferred, 14/18 were related to a deferred vessel, with 2 due to restenosis, and 2 due to lesion progression.
Multiple trials have shown that PCI can be safely deferred in non-flow limiting lesions based on invasive physiological assessment, leading to improved clinical outcomes2,5–7. Contemporary guidelines recommend the use of physiology in intermediate lesions, therefore the choice to use an angiographic-based strategy rather than a pressure wire-based strategy as the comparator in this study is a limitation. On the other hand, in real-world practice, many cardiologists do not routinely use invasive physiology, citing time or resource limitations along with potential complications. The sustained improved outcomes at 2 years with QFR demonstrate that QFR adds to angiographic assessment. QFR in the context of this trial did not add significant time delays to the procedure, whether this will translate to use in settings where wire-based techniques are not currently used or a change in practice of those who routinely use wire-based physiology assessment is to be determined.
A note of caution when interpreting the results, current QFR technology requires acquisition of two angiographic images separated by > 25° for each lesion, with no significant vessel tortuosity or overlap, with current technology QFR may not be feasible in up to 20 % of cases. Accuracy and reproducibility of QFR are dependent on technique and angiographic quality.
Overall, the patients enrolled had low anatomical complexity (mean SYNTAX Scores QFR 9.3 ± 6.0 vs. angio 9.6 ± 6.3) therefore, the results may not be generalisable to a higher-risk population. Furthermore, in the population as a whole, 189 patients underwent ischaemia-driven revascularisation, and in 20.1 % of cases, the culprit lesion had < 50 % diameter stenosis at baseline angiography. This rapid progression of CAD once again raises the question of the vulnerable plaque or other features not identified by physiology alone, which contribute to disease progression.
Given the outcome of this trial, revascularisation guided by QFR appears to be a reasonable option in patients with intermediate lesions suitable for QFR analysis. The two-year results are reassuring in terms of sustained benefit above and beyond the initial early improved clinical outcomes with QFR guidance. Longer-term follow-up, as well as the results of the FAVOR Europe-Japan trial comparing QFR to pressure wire-guided revascularisation, will help determine the role of QFR in physiology-guided revascularisation.
References
- Xu B, Tu S, Song L, Jin Z, Yu B, Fu G, et al. Angiographic quantitative flow ratio-guided coronary intervention (FAVOR III China): a multicentre, randomised, sham-controlled trial. The Lancet. 2021 Dec 11;398(10317):2149–59.
- Pijls NHJ, Fearon WF, Tonino PAL, Siebert U, Ikeno F, Bornschein B, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) study. J Am Coll Cardiol. 2010 Jul 13;56(3):177–84.
- Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. European Heart Journal. 2019 Jan 7;40(2):87–165.
- Tu S, Huang Z, Koning G, Cui K, Reiber JHC. A novel three-dimensional quantitative coronary angiography system: In-vivo comparison with intravascular ultrasound for assessing arterial segment length. Catheter Cardiovasc Interv. 2010 Aug 1;76(2):291–8.
- Banning AP, Serruys P, De Maria GL, Ryan N, Walsh S, Gonzalo N, et al. Five-year outcomes after state-of-the-art percutaneous coronary revascularization in patients with de novo three-vessel disease: final results of the SYNTAX II study. European Heart Journal. 2022 Apr 1;43(13):1307–16.
- Davies JE, Sen S, Dehbi HM, Al-Lamee R, Petraco R, Nijjer SS, et al. Use of the Instantaneous Wave-free Ratio or Fractional Flow Reserve in PCI. N Engl J Med. 2017 May 11;376(19):1824–34.
- Götberg M, Christiansen EH, Gudmundsdottir IJ, Sandhall L, Danielewicz M, Jakobsen L, et al. Instantaneous Wave-free Ratio versus Fractional Flow Reserve to Guide PCI. N Engl J Med. 2017 May 11;376(19):1813–23.




No comments yet!