FAVOR III China: Angiographic quantitative flow ratio-guided coronary intervention - a multicentre, randomised, sham-controlled trial
Reported from TCT 2021
Nicola Ryan provides her take on this investigator initiated, multicentre, randomised, blinded, sham controlled trial compares clinical outcomes of QFR versus angiography guided strategies for the treatment of non-critical lesions in patients with stable or unstable angina or MI at least 72 hours prior to screening. This trial was presented by Bo Xu.
Why this study – the rationale/objective?
Pressure wire based physiological assessment has been shown to more accurately identify flow limiting lesions than angiography alone. Despite the guideline recommendation for invasive physiological assessment its use in real world clinical practice is limited. Quantitative flow ratio (QFR) uses 3D coronary reconstruction and computational fluid dynamics to estimate FFR based on angiography alone. Prior studies have shown a good correlation between QFR and FFR.
How was it executed - the methodology?
From December 2018 to January 2020, patients presenting with stable or unstable angina or MI at least 72 hours prior to screening, with at least one 50-90% stenosis in a vessel ≥2.5mm diameter at coronary angiography were randomised (1:1) to QFR guided versus angiography guided revascularisation. Exclusion criteria included significant vessel tortuosity or overlap not amenable to QFR and renal impairment (eGFR <45ml l/kg/1·73 m2). Clinicians declared their intended treatment strategy for all lesions prior to randomisation. There was a pre-set 10 minute delay for real or sham QFR calculation prior to PCI. PCI was performed in lesions with QFR <0.80 and deferred with a QFR >0.80 in the QFR group. Participants and clinical assessors were blinded to treatment outcomes.
- The primary outcome was MACE a composite of all cause death, MI and ischaemia driven revascularisation at one year.
- The major secondary endpoint was the one year MACE rate excluding peri-procedural MI
- Other secondary endpoints included PCI strategy changes, death, MI, TVR and revascularisation and stent thrombosis.
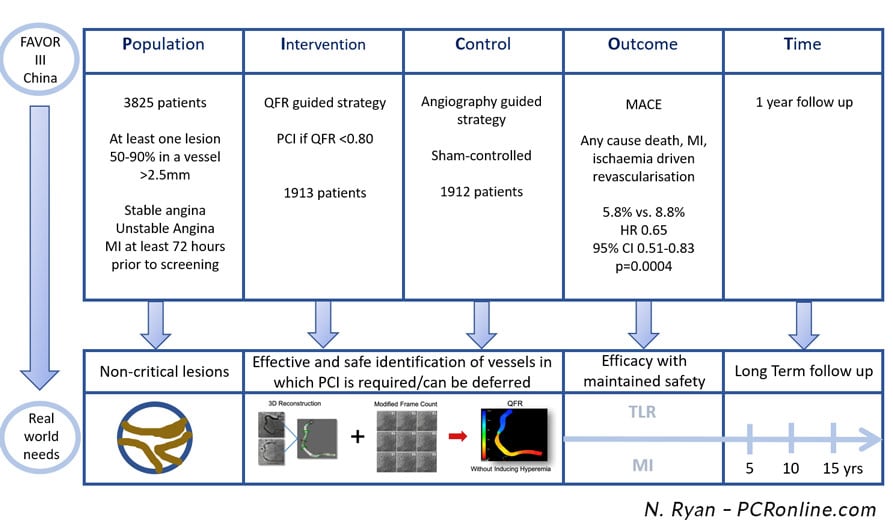
PICOT analysis of the FAVOR-III China Trial - source : Nicola Ryan
What is the main result?
Overall, 3847 patients from 26 sites in China were enrolled in the trial. Following withdrawal of consent 1913 randomised to QFR guided revascularisation and 1912 randomised to angiography guided revascularisation were included in the ITT analysis. The majority of participants were men (70.6%) with a mean age of 62.7±10.1 years. The most common clinical presentation was ACS (63.5%) with a third of patients diabetic. The majority of patients had single vessel CAD (46.5% vs. 45.4%), with approximately 50% of lesions in the LAD. Mean QFR calculation time was 3.9±1.4min.
- The primary endpoint occurred in 5.8% (11/1913) of patients in the QFR group compared to 8.8% (167/1912) in the angiography group (HR 0.65, 95% CI 0.51-0.83, p=0.004) at one year.
- The major secondary endpoint occurred in 3.1% (59/1913) of patients in the QFR group and 4.8% (91/1912) of patients in the angiography group (HR 0.64, 95%CI 0.46-0.89, p=0.0078).
- Lower rates of the primary endpoint in the QFR group were driven by lower rates of MI 3.4% vs. 5.7% and ischaemia driven revascularisation 2.0% vs. 3.1%).
- QFR changed treatment strategy in 23.3% of patients (deferral 19.6%, treatment of a vessel not initially planned for treatment 4.4%), whilst the initial strategy was changed in 6.2% of the angiographic group (deferral 5.2%, treatment of a vessel not initially planned for treatment 1.5%).
- Higher rates of functionally complete revascularisation (post-PCI QFR assessment) were achieved in the QFR guided group (88.1% vs. 82.2%).
Critical reading and the relevance for clinical practice
The results of this investigator initiated multicentre randomised blinded, sham controlled trial showed that a QFR guided strategy was superior to an angiography guided strategy in terms of clinical outcomes at one year. Overall, QFR gave a 35% risk reduction in MACE at one year driven by reduced MI, both periprocedural and non-procedural, and ischaemia driven revascularisation. Importantly, subgroup analysis including by gender, presentation (ACS or not) and lesion location favoured a QFR guided strategy. Based on QFR the revascularisation strategy changed for almost a quarter of patients. QFR calculation was rapid with a mean calculation time of 3.9±1.4 mins and lead to reduced numbers of stents implanted, contrast use and radiation exposure along with a shorter procedural time.
Multiple trials have shown that PCI can be safely deferred in non-flow limiting lesions based on invasive physiological assessment leading to improved clinical outcomes. Contemporary guidelines recommend the use of physiology in intermediate lesions therefore the choice to use an angiographic based strategy rather than a pressure wire based strategy as the comparator in this study is a limitation. On the other hand in real world practice many cardiologists do not routinely use invasive physiology citing time or resource limitations along with potential complications. This study demonstrates that QFR adds to angiographic assessment without adding significant time delays to the procedure, whether this will translate to use in settings where wire based techniques are not currently used or a change in practice of those who routinely use wire based physiology assessment is to be determined.
A note of caution when interpreting the results, current QFR technology requires acquisition of two angiographic images separated by >25° for each lesion with no significant vessel tortuosity or overlap, with current technology QFR may not be feasible in up to 20% of cases. Accuracy and reproducibility of QFR is dependent on technique and angiographic quality. Overall the patients enrolled had low anatomical complexity (mean SYNTAX Scores QFR 9.3±6.0 vs. Angio 9.6±6.3) therefore the results may not be generalisable to a higher risk population.
Given the outcome from this trial revascularisation guided by QFR appears to be a reasonable option in patients with intermediate lesions suitable for QFR analysis. Longer term follow up as well as the results of the FAVOR Europe-Japan trial comparing QFR to pressure wire guided revascularisation will help determine the role of QFR in physiology guided revascularisation.




No comments yet!