02 Feb 2022
Improved 3-year cardiac survival after IVUS-guided long DES implantation: a patient-level analysis from 2 randomized trials
Selected in JACC: Cardiovascular Interventions by N. Ryan
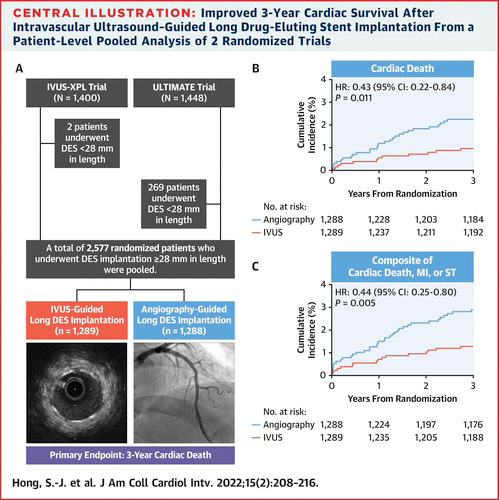
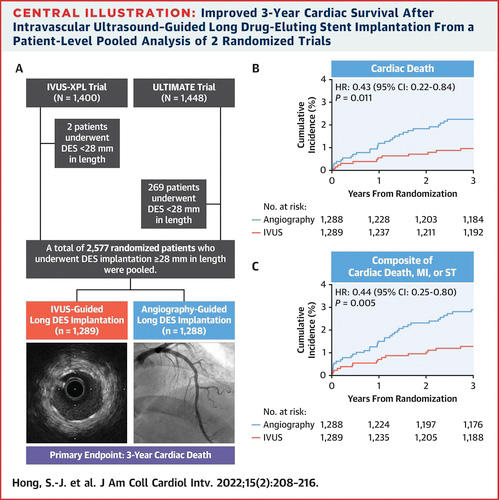
This study aimed to increase the power to detect differences in patient survival (freedom from cardiac deaths) with IVUS versus angiography guidance by pooling the individual patient data from the IVUS-XPL and ULTIMATE trials.
References
Authors
Sung-Jin Hong, Jun-Jie Zhang, Gary S. Mintz, Chul-Min Ahn, Jung-Sun Kim, Byeong-Keuk Kim, Young-Guk Ko, Donghoon Choi, Yangsoo Jang, Jing Kan, Tao Pan, Xiaofei Gao, Zhen Ge, Shao-Liang Chen, and Myeong-Ki Hong
Reference
J Am Coll Cardiol Intv. 2022 Jan, 15 (2) 208–216
Published
January 2022
Link
Read the abstract
Reviewer
Latest contributions
Balloon lithotripsy added to conventional preparation before stent implantation in severely calcified coronary lesions Impact of pullback pressure gradient on clinical outcomes after percutaneous coronary interventions Validation of intravascular ultrasound-defined optimal stent expansion criteria for favorable 1-year clinical outcomesMy Comment
Why this study – the rationale/objective?
The IVUS-XPL1 (Impact of intravascular ultrasound guidance on the outcomes of Xience Prime stents in long lesions) trial demonstrated that the 5-year composite endpoint of cardiac death, target lesion related MI or ischaemia driven TLR were significantly lower in the IVUS guided arm (5.6 % vs 10.7 %, HR 0.5, 95 % CI 0.34-0.75, p = 0.001). Whilst the ULTIMATE2 (Intravascular ultrasound-guided drug-eluting stents implantation in all-comers coronary lesions) trial demonstrated that at three years, TVF (cardiac death, target vessel MI and clinically driven TVR) was significantly higher in the angiography guided group compared to the IVUS guided group (10.7 % vs. 6.6 %, HR 0.60, 95 % CI 0.42-0.87, p = 0.01).
Neither of the above trials demonstrated a reduction in cardiac death, MI, or stent thrombosis in the longer term.
This study aimed to increase the power to detect differences in patient survival (freedom from cardiac deaths) with IVUS versus angiography guidance by pooling the individual patient data from the IVUS-XPL and ULTIMATE trials.
How was it executed? - the methodology
In this analysis, the authors pooled the data of 2,577 patients from the IVUS-XPL and ULTIMATE trials undergoing angiography versus IVUS guided PCI in long lesions, treated with stents > 28 mm in length. In both trials, patients were randomised in a 1:1 fashion to IVUS or angiography guidance.
- The primary endpoint was cardiac death at three-year follow-up.
- The composite endpoint of cardiac death, MI, or stent thrombosis at 3-year was also reported.
- Optimal PCI in the IVUS group required all three IVUS criteria (MLA > 5 mm or 90 % of the MLA at the distal reference segments, plaque burden 5 mm proximal or distal to the stent edge < 50 % and no edge dissection involving the media with length > 3 mm) in the ULTIMATE trial, whilst IVUS-XPL IVUS optimisation was a minimal luminal cross-sectional area greater than the luminal cross-sectional area at the distal reference segment.
What is the main result?
Overall, 1,289 patients were randomised to IVUS guidance and 1,288 to angiography guidance. Almost three quarters of patients were male, 38 % presented with stable angina with no significant differences in cardiovascular risk factors. From an angiographic point of view, > 50% had an LMS or LAD lesion, with MVD common (> 60 %).
Post-dilation was more commonly undertaken in the IVUS guided group (88 % vs 7 9%, p < 0.001) with larger final balloon sizes (3.62 ± 0.66 vs. 3.51 ± 0.63, p < 0.001) and larger post intervention QCA minimum lumen diameters (2.56 ± 0.47 vs 2.49 ± 0.45, p < 0.001).
- Cardiac death was less common in the IVUS guided group (1 % vs. 2.2 %, HR 0.43, 95 % CI 0.22-0.84, p = 0.011) at 3-year follow-up.
- The composite endpoint of cardiac death, MI, or ST occurred less commonly in the IVUS guided group (1.3 % vs. 1.0 %, HR 0.44, 95 %CI 0.25-0.80, p = 0.005).
- Target lesion related MI occurred in 3 patients (0.2 %) in the IVUS group vs. 9 patients (0.7 %) in the angiography group (HR 0.33, 95 % CI 0.09-1.22, p = 0.081).
- Stent thrombosis was numerically lower in the IVUS guided group (0.2 % vs 0.7 %, HR 0.33, 95 % CI 0.09-1.23, p = 0.082).
- Significantly lower rates of ischaemia driven revascularisation were seen with IVUS guidance (3.8 % vs 6.5 %, HR 0.57, 95 % CI 0.4-0.82, p = 0.002).
- Results were consistent at subgroup analysis including, sex, age, presence of diabetes, and clinical presentation.
- In the IVUS group, the composite endpoint of cardiac death MI or ST occurred less commonly those who met IVUS criteria for optimal PCI (0.5 % vs 2.2 %, HR 0.22, 95 % CI 0.06-0.75, p = 0.008) with numerically but not statistically significantly lower rates of cardiac death (0.5 % vs 1.5 %, HR 0.31, 95 % CI 0.08-1.15, p = 0.064).
Source = JACC: Cardiovascular Interventions
Critical reading and the relevance for clinical practice
The results of this pooled patient-level analysis show that at three years, an IVUS guided PCI strategy compared to an angiography-guided strategy results in lower rates of cardiac death, as well as a reduction in the composite hard endpoint of cardiac death, MI, or stent thrombosis.
Previously the non-randomised ADAPT-DES trial3 showed a reduction in MACE (cardiac death, MI, or ST,4.9 % vs 7.5 %, adj HR 0.72; 95 % CI 0.59–0.89, p = 0.003), stent thrombosis (0.55 % vs 1.16 %, adj HR 0.40; 95 % CI 0.22–0.73, p = 0.003), and MI (3.5 % vs 5.6 %, adj HR 0.65, 95 % CI 0.51–0.83 p = 0.0006) at two years with IVUS guidance. This randomised data supports the reduction of hard endpoints with IVUS guidance rather than simply a reduction in repeat revascularistion.
In this analysis, the benefit of IVUS guidance persisted across important subgroups, including clinical presentation, stent length, risk factors, sex, and age. Importantly, in the IVUS group, those who met IVUS criteria for optimal PCI had a lower rate of the composite endpoint (cardiac death, MI, ST) and a numerically lower rate of cardiac death (not statistically significant likely due to the small numbers included). This reinforces that the use of IVUS alone is insufficient to improve outcomes and that the interpretation and action based on IVUS results are key to reduced hard endpoints.
A note of caution when interpreting the results, IVUS interpretation requires appropriate training, and even in the context of these RCT IVUS defined optimal PCI was only achieved in 52 % of patients. Furthermore, the criteria for IVUS defined optimal PCI differed between the two trials with the rates of cardiac death differing between IVUS defined optimal and non-optimal PCI in the ULTIMATE trial but not the IVUS-XPL, suggesting that the ULTIMATE criteria may be more predicative of improved outcomes.
Finally, this analysis only included patients with stents > 28 mm in length implanted therefore, generalisation of survival benefit to patients undergoing PCI with shorter stents cannot be assumed.
In summary, this pooled patient-level analysis provides long-term randomised control data showing the benefit of IVUS guided PCI in patients with long lesions. The current guidelines recommend IVUS use in selected patients however this adds support to the evidence for it’s more liberal use. Given the improved outcomes with optimal versus suboptimal IVUS guided PCI, it is important that IVUS images are carefully reviewed and stents optimised to gain most benefit from IVUS use.
References
- Hong S-J, Mintz GS, Ahn C-M, Kim J-S, Kim B-K, Ko Y-G, et al. Effect of Intravascular Ultrasound-Guided Drug-Eluting Stent Implantation: 5-Year Follow-Up of the IVUS-XPL Randomized Trial. JACC Cardiovasc Interv. 2020 Jan 13;13(1):62–71.
- Gao X-F, Ge Z, Kong X-Q, Kan J, Han L, Lu S, et al. 3-Year Outcomes of the ULTIMATE Trial Comparing Intravascular Ultrasound Versus Angiography-Guided Drug-Eluting Stent Implantation. JACC Cardiovasc Interv. 2021 Feb 8;14(3):247–57.
- Maehara A, Mintz GS, Witzenbichler B, Weisz G, Neumann F-J, Rinaldi MJ, et al. Relationship Between Intravascular Ultrasound Guidance and Clinical Outcomes After Drug-Eluting Stents. Circulation: Cardiovascular Interventions. 2018 Nov 1;11(11):e006243.