Optimal minimal stent area and impact of stent underexpansion in left main up-front 2-stent strategy
Selected in Circulation: Cardiovascular Interventions by S. Brugaletta
The present study aimed to revise the IVUS-derived segmental MSA criteria for optimal stent expansion in patients undergoing an up-front 2-stent strategy using the crush technique for LM bifurcation lesions to predict the 5-year clinical outcomes.
References
Authors
Ju Hyeon Kim, Do-Yoon Kang, Jung-Min Ahn, Jihoon Kweon, Yeonwoo Choi, Hoyun Kim, Jinho Lee, Jihye Chae, Soo-Jin Kang, Duk-Woo Park, and Seung-Jung Park
Reference
Circulation: Cardiovascular Interventions Volume 17, Number 1 https://doi.org/10.1161/CIRCINTERVENTIONS.123.013006
Published
January 2024
Link
Read the abstractReviewer
My Comment
Why this study – the rationale/objective?
Current guidelines recommend the use of intra-coronary imaging during left main stenting because intravascular ultrasound guidance can improve clinical outcomes by ensuring well-apposed and adequately expanded stents.
The so-called 5-6-7-8 rule of criteria, based on intravascular ultrasound measured minimal stent area in patients undergoing left main stenting, are currently proposed for evaluating optimal stent expansion to predict angiographic in-stent restenosis.
This rule is based on a study, included heterogeneous population who underwent either a single- stent (72 %) or an up-front 2-stent strategy (28 %) and predicted the risk of angiographic restenosis at 9-month follow-up.
The present study aimed to revise the IVUS- derived segmental MSA criteria for optimal stent expansion in patients undergoing an up-front 2-stent strategy using the crush technique for LM bifurcation lesions to predict the 5-year clinical outcomes.
How was it executed – the methodology?
292 consecutive patients with LM bifurcation stenosis who were treated using the crush technique were identified. The final minimal stent area was measured in the ostial left anterior descending artery (LAD), ostial left circumflex artery (LCX), and distal LM.
The primary outcome was 5-year major adverse cardiac events, including all-cause death, myocardial infarction, and target lesion revascularization.
What is the main result?
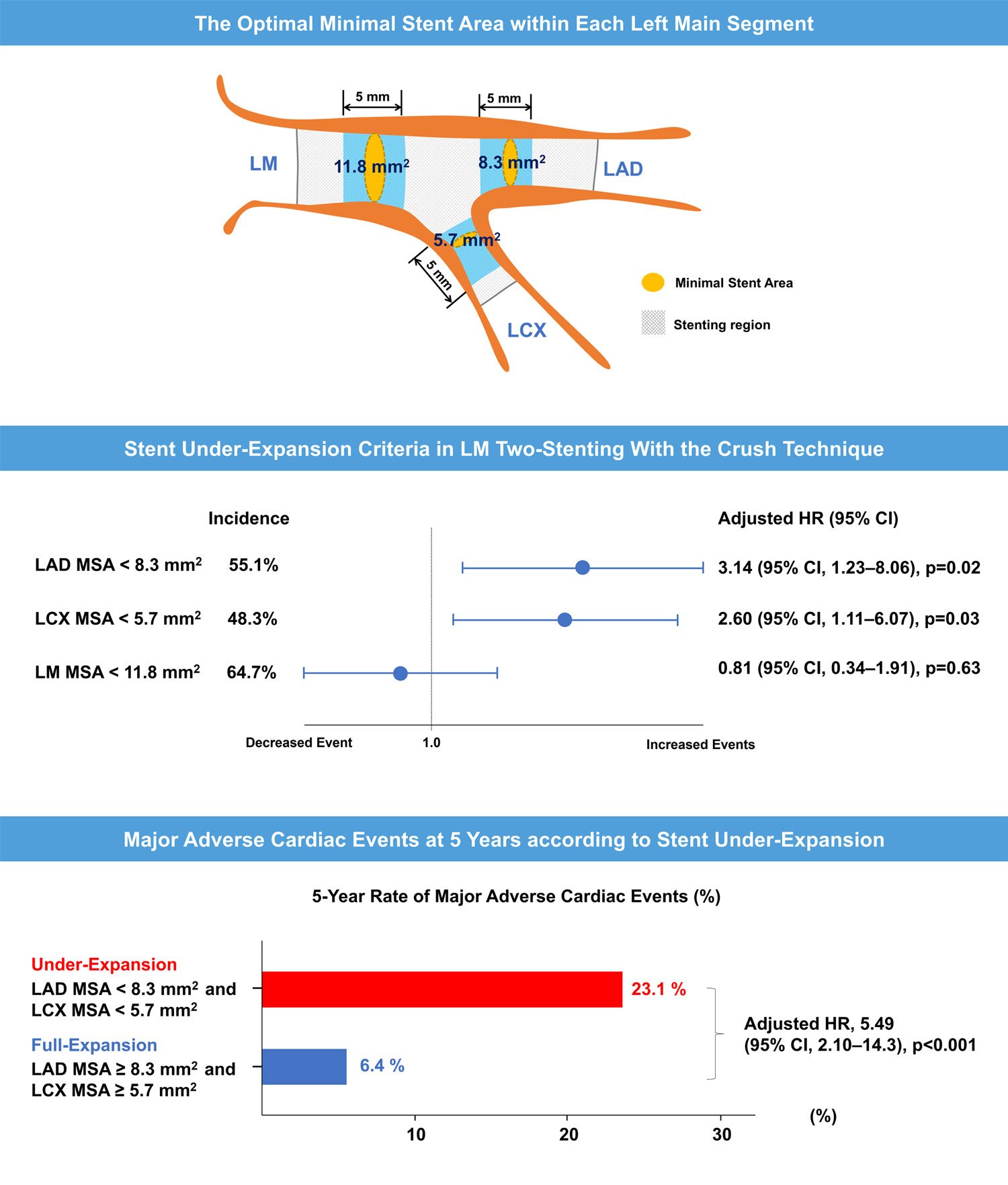
The minimal stent area cutoff values that best predicted the 5-year major adverse cardiac events were 11.8 mm2 for distal LM (area under the curve, 0.57; P = 0.15), 8.3 mm2 for LAD ostium (area under the curve, 0.62; P = 0.02), and 5.7 mm2 for LCX ostium (area under the curve, 0.64; P = 0.01).
Using these criteria, the risk of 5-year major adverse cardiac events was significantly associated with stent underexpansion in the LAD ostium (hazard ratio, 3.14; [95 % CI, 1.23–8.06]; P = 0.02) and LCX ostium (hazard ratio, 2.60 [95 % CI, 1.11–6.07]; P = 0.03) but not in the distal LM (hazard ratio, 0.81 [95 % CI, 0.34–1.91]; P = 0.63).
Patients with stent underexpansion in both ostial LAD and LCX had a significantly higher rate of 5-year major adverse cardiac events than those with no or 1 underexpanded stent of either ostium (P < 0.01).
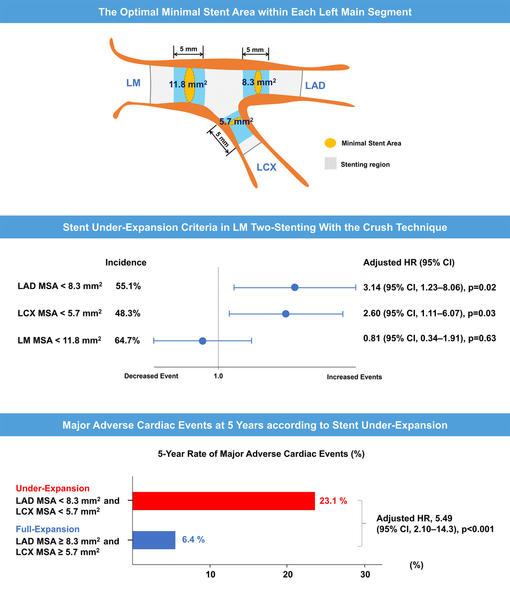
Graphical representation summarising the study on stent under-expansion in the LAD and LCX ostium
Source: Circulation: Cardiovascular Interventions
Critical reading and the relevance for clinical practice
When performing left main PCI, we wonder which is the optimal stent area to reach, not only in left main, but also in LAD and LCx.
Since years, the rule of 5-6-7-8 is well known, but not applied in clinical practice, as it comes from Asian patients whose BMI is lower than European patients. In this regard, the present study give us a new rule which can be easily applied in an overall population.
Whereas, to me, it is very much clear that area to be reached in left main should be at least 11 mm2, according to the size of the stent usually implanted at this level (> 3.5 mm of diameter), it is very interesting to see that we should put an extra eye on checking LAD and LCx ostium, as stent underexpansion in the LAD and LCX ostium was significantly associated with long-term outcomes in patients who underwent up-front 2-stenting for LM bifurcation stenosis.
Last but not least, this study also reinforces the need of imaging IVUS in LM PCI.





No comments yet!