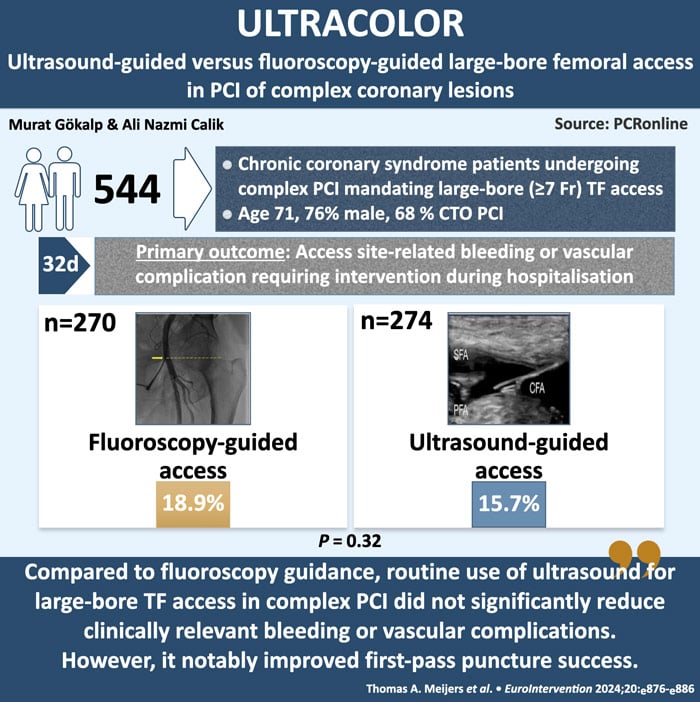
Ultrasound-guided versus fluoroscopy-guided large-bore femoral access in PCI of complex coronary lesions: the international, multicentre, randomised ULTRACOLOR Trial
Selected in EuroIntervention by A. N. Calik , M. Gökalp
Compared to fluoroscopy guidance, routine use of ultrasound for large-bore transfemoral access in complex PCI did not significantly reduce clinically relevant bleeding or vascular complications. However, it notably improved first-pass puncture success, with a very low crossover rate.
References
Authors
Tom A. Meijers; Alexander Nap; Adel aminian; Thomas Schmitz; Joseph Dens; Koen Teeuwen; Jan-Peter van Kuijk; Marleen van Wely; Yoann Bataille; Adriaan O. Kraaijeveld; Vincent Roolvink; Jan-Henk E. Dambrink; A.T. Marcel Gosselink; Renicus S. Hermanides; Jan Paul Ottervanger; Ioannis Tsilingiris; Deborah M.F van den Buijs; Niels van Royen; Maarten A.H. van Leeuwen
Reference
10.4244/EIJ-D-24-00089 • Jul 15, 2024
Published
Jul 15, 2024
Link
Read the abstractReviewers
Our Comment
ULTRACOLOR is an international, multicenter, prospective, open-label, randomized controlled clinical trial investigating whether ultrasound-guided large-bore femoral access reduces clinically relevant access site complications compared to fluoroscopy-guided large-bore femoral access in percutaneous coronary interventions (PCI) for complex coronary lesions.
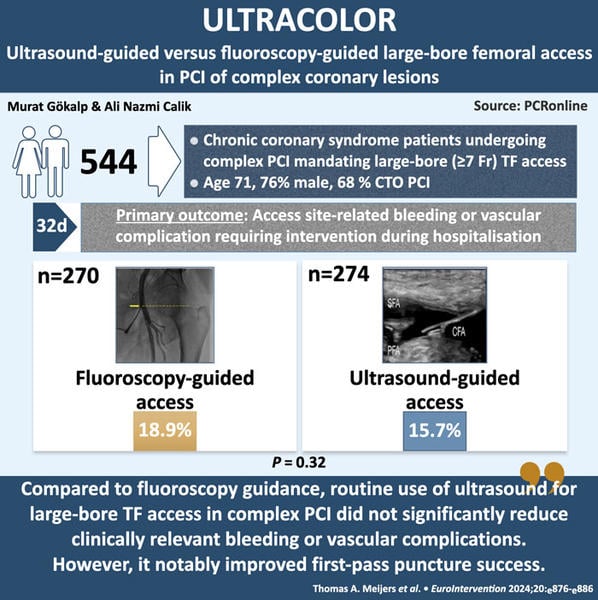
Infographic presenting the key information from the ULTRACOLOR trial.
Designed by by Murat Gokalp and Ali Nazmi Calik. Source: PCRonline.com
Why this study - the rationale/objective?
In the treatment of complex lesions, including heavily calcified lesions, left main lesions, complex bifurcations, and chronic total occlusions (CTOs), large-bore (7 or 8 Fr) catheters are preferred for improved backup support and better compatibility1,2. Recent studies have demonstrated the feasibility and increased safety of large-bore transradial access (TRA) for complex PCI compared to transfemoral access (TFA)3,4. The safety of large-bore TFA remains a topic of discussion in patients for whom TRA is not suitable.
Ultrasound-guided puncture of the femoral artery in coronary procedures, including large-bore access for complex PCI, is not routinely employed, likely due to a lack of robust evidence. Furthermore, previous studies have demonstrated that routine ultrasound-guided femoral access does not reduce bleeding and vascular complications compared to fluoroscopy-guided access5.
The aim of this study is to compare the efficacy of ultrasound-guided large-bore TFA with fluoroscopy-guided access concerning vascular complications and bleeding in patients undergoing complex PCI.
How was it executed - the methodology
Patients aged 18 years or older with chronic coronary syndrome and complex coronary lesions (including chronic total occlusion, left main lesions, heavily calcified lesions, and complex bifurcations) who were scheduled for PCI and required large-bore (7 or 8 Fr) TFA were included in the study. Patients with ST-segment elevation myocardial infarction or cardiogenic shock were excluded.
Patients were randomized in a 1:1 ratio to receive either ultrasound-guided puncture (after palpation of the femoral artery, the puncture was performed by visualizing the artery with ultrasound) or fluoroscopy-guided puncture (after palpation of the femoral artery, the location of the femoral head was confirmed using fluoroscopy, and the puncture was performed).
The primary endpoint was defined as clinically relevant access site-related bleeding or vascular complications requiring intervention at the primary femoral access site during the index hospitalization. Bleeding was classified according to the Bleeding Academic Research Consortium (BARC) criteria and was considered clinically relevant when the score was 2, 3, or 56.
What is the main result?
From June 2021 to March 2023, a total of 544 patients were included and randomized to either ultrasound-guided large-bore transfemoral access (274 patients) or fluoroscopy-guided large-bore transfemoral access (270 patients).
The median age of the patients was 71 years, with 76 % being male. The right femoral artery was predominantly used as the primary access site (92 %). An additional arterial access site was utilized in 56 % of patients, of whom 21 % had femoral and 79 % had radial secondary access. The first-pass puncture success rate was higher in the ultrasound-guided group (92 % vs. 85 %; p = 0.02). The median number of attempts was 1 in each group (interquartile range [IQR] 1-1). The median time to access was 60 seconds (IQR 60-135) for ultrasound-guided access and 60 seconds (IQR 60-150) for fluoroscopy-guided access. High puncture occurred significantly more often in the ultrasound-guided access group (5 % vs. 1 %; p = 0.03), while low puncture occurred more frequently in the fluoroscopy-guided group (10 % vs. 5 %; p = 0.02). Accidental venepuncture occurred in 4 % of patients with fluoroscopy-guided access compared to 2 % with ultrasound-guided access (p = 0.18). The median procedural duration was 75 minutes (IQR 55-120) for ultrasound-guided access and 75 minutes (IQR 50-120) for fluoroscopy-guided access. The success rates for patients undergoing CTO PCI and non-CTO complex PCI were 91 % and 99 %, respectively.
The primary endpoint, at discharge, occurred in 15.7 % of patients in the ultrasound-guided group, compared to 18.9 % in the fluoroscopy-guided group (p = 0.32). There were no significant differences in the individual components of the primary endpoint between the two groups. The same applied for secondary safety outcomes, including secondary access site BARC 2, 3 or 5 bleeding or vascular complication requiring intervention and MACE.
The occurrence of primary access site BARC 2, 3 or 5 bleeding or vascular complications requiring intervention at follow-up (32 days) did not show a statistically significant difference between the fluoroscopy-guided and ultrasound-guided group (21 % vs 16 %; p = 0.19).
Critical reading and the relevance for clinical practice
The ULTRACOLOR study offers valuable insights into ultrasound-guided puncture and fluoroscopy-guided puncture for large-bore TFA in patients for whom radial access is not feasible. While ultrasound-guided access increases the rate of first-pass punctures, it was found to produce results comparable to fluoroscopy-guided access regarding procedural site bleeding and vascular complications, both during hospitalization and at the 30-day follow-up. Additionally, when examining secondary endpoints, similar outcomes were noted, including those related to MACE.
This study makes a significant contribution by comparing the clinical outcomes of ultrasound-guided puncture and fluoroscopy-guided puncture, especially in the context of the UNIVERSAL trial. In the UNIVERSAL trial, researchers compared ultrasound-guided transfemoral access (TFA) with fluoroscopy-guided TFA in patients undergoing non-complex PCI with standard sheath sizes. Although the first-pass puncture rate was higher in the ultrasound-guided group, no significant differences were found in procedural site bleeding and vascular complications5. Recently, two meta-analyses have been published that focus on ultrasound-guided versus non-ultrasound-guided femoral puncture in coronary procedures, both of which included the same nine trials. These analyses found that the occurrence of clinically relevant bleeding events classified as BARC 2 and 3 was not significantly reduced with the use of ultrasound guidance7. In this context, the findings align with existing literature as well as the results of the UNIVERSAL trial. Another notable aspect of this analysis is that ultrasound-guided access was linked to a significantly lower frequency of sheath placement below the femoral bifurcation. This is logical, as ultrasound allows for direct visualization of the femoral bifurcation. By utilizing this technique, it helps prevent suboptimal puncture height and minimizes the risk of puncturing calcified plaques.
It is important to consider the limitations of the ULTRACOLOR Trial, including the inability to blind operators to the randomized strategy, which may have introduced bias, and the use of secondary access sites, potentially influencing the outcomes. The trial was underpowered to detect smaller differences in access site complications, and subgroup analyses were constrained by a relatively small sample size. Additionally, the use of micropuncture was minimal, and there was variability in operator experience with ultrasound, despite the provision of standardized training.
In conclusion, compared to fluoroscopy guidance, routine use of ultrasound for large-bore transfemoral access in complex PCI did not significantly reduce clinically relevant bleeding or vascular complications. However, it notably improved first-pass puncture success, with a very low crossover rate. Furthermore, the total time spent in the catheterization lab and the time to achieve access were comparable between the two techniques, suggesting that ultrasound-guided access is a viable option in these patients.
References
- Ikari Y, Nagaoka M, Kim JY, Morino Y, Tanabe T. The physics of guiding catheters for the left coronary artery in transfemoral and transradial interventions. J Invasive Cardiol. 2005;17:636-41.
- Ghione M, Agudo P, Kilickesmez K, Estevez-Loureiro R, Zivelonghi C, Lindsay A, Foin N, Secco GG, Di Mario C. Tools and techniques - clinical: catheter compatibility in CTO recanalisation. EuroIntervention. 2013;9: 290-1.
- Meijers TA, Aminian A, van Wely M, Teeuwen K, Schmitz T, Dirksen MT, Rathore S, van der Schaaf RJ, Knaapen P, Dens J, Iglesias JF, Agostoni P, Roolvink V, Hermanides RS, van Royen N, van Leeuwen MAH. Randomized Comparison Between Radial and Femoral Large-Bore Access for Complex Percutaneous Coronary Intervention. JACC Cardiovasc Interv. 2021;14:1293-303.
- Gorgulu S, Kalay N, Norgaz T, Kocas C, Goktekin O, Brilakis ES. Femoral or Radial Approach in Treatment of Coronary Chronic Total Occlusion: A Randomized Clinical Trial. JACC Cardiovasc Interv. 2022;15:823-30.
- Jolly SS, AlRashidi S, d’Entremont MA, Alansari O, Brochu B, Heenan L, Skuriat E, Tyrwhitt J, Raco M, Tsang M, Valettas N, Velianou JL, Sheth T, Sibbald M, Mehta SR, Pinilla-Echeverri N, Schwalm JD, Natarajan MK, Kelly A, Akl E, Tawadros S, Camargo M, Faidi W, Bauer J, Moxham R, Nkurunziza J, Dutra G, Winter J. Routine Ultrasonography Guidance for Femoral Vascular Access for Cardiac Procedures: The UNIVERSAL Randomized Clinical Trial. JAMA Cardiol. 2022;7:1110-8.
- Vranckx P, White HD, Huang Z, Mahaffey KW, Armstrong PW, Van de Werf F, Moliterno DJ, Wallentin L, Held C, Aylward PE, Cornel JH, Bode C, Huber K, Nicolau JC, Ruzyllo W, Harrington RA, Tricoci P. Validation of BARC Bleeding Criteria in Patients With Acute Coronary Syndromes: The TRACER Trial. J Am Coll Cardiol. 2016;67:2135-44.
- Mehran R, Pocock S, Nikolsky E, Dangas GD, Clayton T, Claessen BE, Caixeta A, Feit F, Manoukian SV, White H, Bertrand M, Ohman EM, Parise H, Lansky AJ, Lincoff AM, Stone GW. Impact of bleeding on mor- tality after percutaneous coronary intervention results from a patient-level pooled analysis of the REPLACE-2 (randomized evaluation of PCI linking angiomax to reduced clinical events), ACUITY (acute catheterization and urgent intervention triage strategy), and HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infarction) trials. JACC Cardiovasc Interv. 2011;4:654-64.






No comments yet!