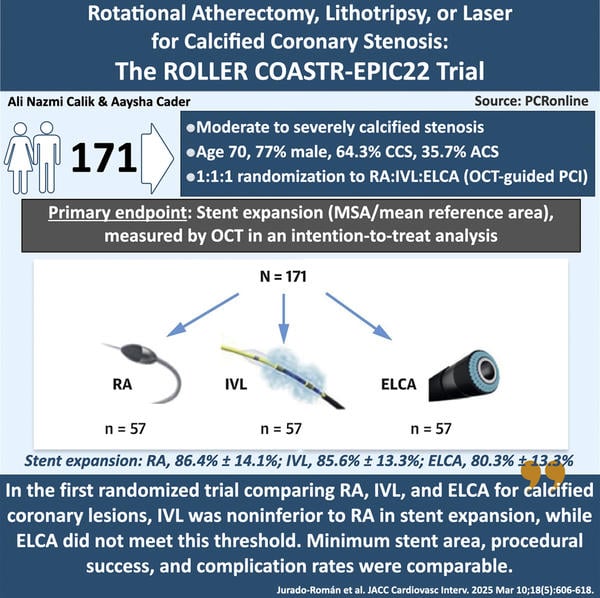
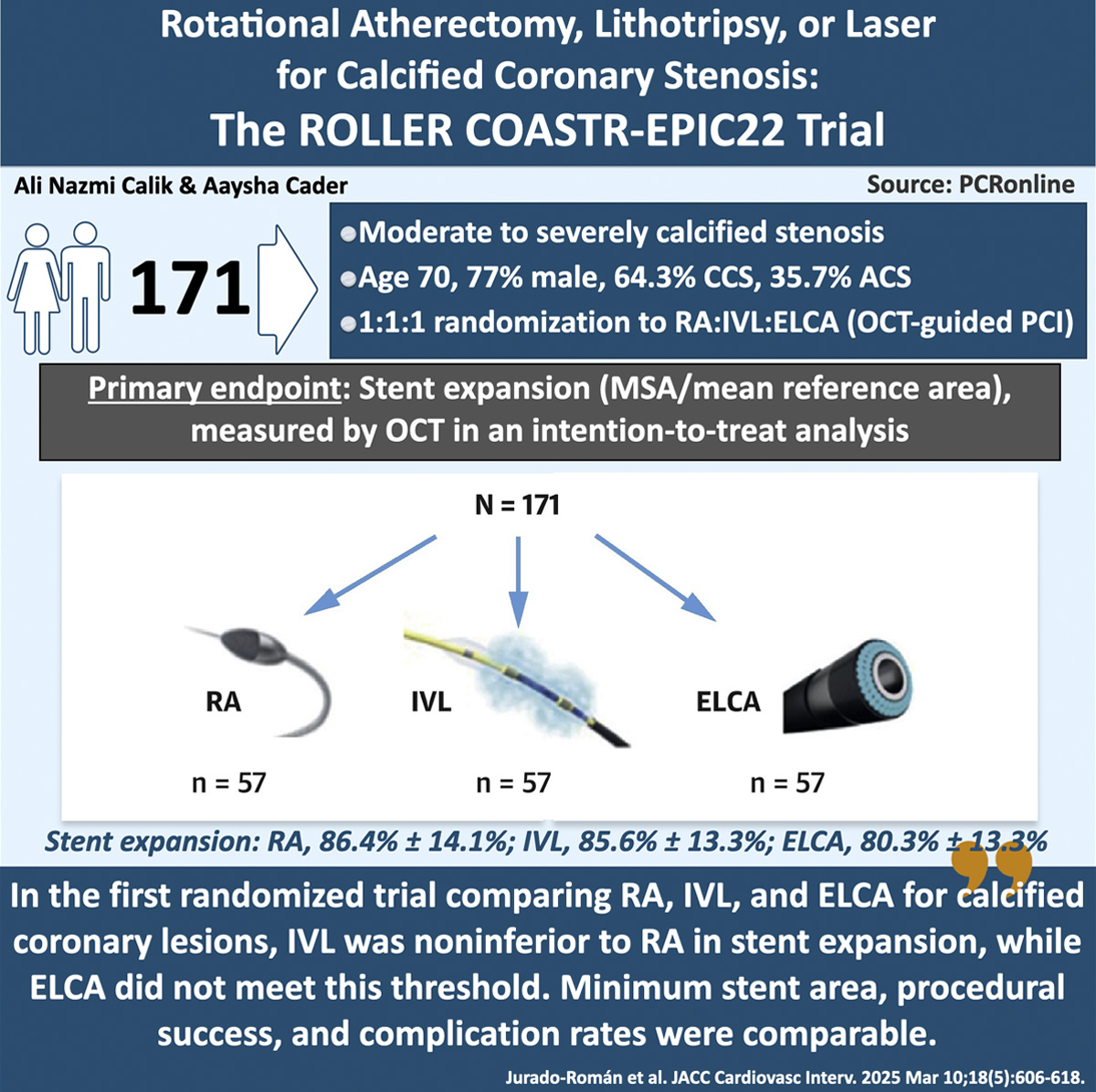
Rotational atherectomy, lithotripsy, or laser for calcified coronary stenosis: the ROLLER COASTR-EPIC22 trial
Selected in JACC: Cardiovascular Interventions by A. N. Calik , A. Cader
Due to a lack of randomised evidence, this randomised controlled trial (RCT) aimed to compare the safety and efficacy of IVL and ELCA with RA in treating heavily calcified coronary lesions before drug-eluting stent implantation.
References
Authors
Alfonso Jurado-Román, Antonio Gómez-Menchero, Borja Rivero-Santana, Ignacio J. Amat-Santos, Santiago Jiménez-Valero, Juan Caballero-Borrego, Soledad Ojeda, Gema Miñana, Ariana Gonzálvez-García, Daniel Tébar-Márquez, Santiago Camacho-Freire, Raymundo Ocaranza-Sánchez, Antonio Domínguez, Guillermo Galeote, and Raúl Moreno
Reference
J Am Coll Cardiol Intv. 2025 Mar, 18 (5) 606–618
Published
2025 Mar, 18
Link
Read the abstractReviewers
Our Comment
Designed by Ali Nazmi Calik & Aaysha Cader - Source: PCRonline
Why this study – the rationale/objective?
Percutaneous coronary intervention (PCI) in heavily calcified lesions is challenging due to difficulties in lesion crossing and suboptimal stent expansion, leading to adverse outcomes like stent thrombosis and repeat revascularisation.
Various plaque modification techniques (PMTs) exist, but selecting the optimal approach depends on lesion characteristics, calcium pattern and patient factors1. Regarding this, intracoronary imaging techniques such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT) are crucial for assessing calcification severity and patterns, as well as optimising stent implantation2. While rotational atherectomy (RA) has long been the standard PMT, emerging technologies like intravascular lithotripsy (IVL) and excimer laser coronary angioplasty (ELCA) have raised questions about the most effective treatment approach.
Due to a lack of randomised evidence, this randomised controlled trial (RCT) aimed to compare the safety and efficacy of IVL and ELCA with RA in treating heavily calcified coronary lesions before drug-eluting stent implantation.
How was it executed – the methodology?
The ROLLER COASTER-EPIC22 trial (NCT04181268) is a multicentre, investigator-initiated, randomised controlled trial conducted at eight high-volume Spanish centres. It included patients (≥ 18 years) undergoing PCI for chronic or acute coronary syndromes with moderate to severe calcified stenosis as assessed by angiography in vessel diameter: 2.5–4.0 mm. ST-elevation MI culprit lesions, cardiogenic shock, and inability to tolerate dual antiplatelet therapy for six months (if not on anticoagulation) were exclusion criteria.
Eligible patients were randomised (1:1:1) via a web-based system to lesion preparation with rotational atherectomy (RA), excimer laser coronary angioplasty (ELCA), or intravascular lithotripsy (IVL). Randomisation occurred before PCI.
After crossing the lesion with a guidewire, an initial OCT assessment was recommended, with predilatation allowed to facilitate catheter crossing. Lesion preparation followed the assigned PMT (RA, ELCA, or IVL), with a subsequent OCT assessment advised.
PCI was completed with a new-generation drug-eluting stent, with predilatation and postdilatation at the operator’s discretion. Final OCT was mandatory to evaluate stent expansion and procedural success.
Combination of the PMTs evaluated in the study was permitted if the initial therapy was unsuccessful, as they have been shown to be complementary. If an additional PMT was required, crossover to the second technique was pre-specified and based on the reason of failure.
The primary endpoint was the percentage of stent expansion, measured by OCT in an intention-to-treat (ITT) analysis. Stent expansion (%) was defined as minimum stent area (MSA) divided by mean reference vessel area.Stent expansion in the IVL and ELCA groups was compared to RA, which was the reference group in an intention-to-treat analysis (for non-inferiority).
Secondary endpoints included device, angiographic, procedural, and clinical success. Device success was defined as crossing the lesion with the initial device and adequate balloon expansion without needing a second advanced PMT.
What is the main result?
From July 2019 to December 2023, 171 patients (77.2 % men, mean age 70.9 ± 8.2 years) were enrolled. Of these, 64.3 % had stable coronary artery disease and 35.7 % had acute coronary syndromes. Baseline characteristics were similar across treatment arms. RA, ELCA, and IVL were each performed in 57 patients (33.3 % each). The left anterior descending artery was the most treated vessel (71.3 %). Core lab evaluation showed significant angiographic calcification in all cases, of which 82.5 % were severe and 17.5 % moderate. No significant differences in calcification severity or other angiographic variables were found between treatment arms (P = 0.489).
OCT evaluation at the end of the procedure could be performed in 135 patients, in whom the primary endpoint was analysed. OCT runs before and after PMTs were obtained in 34.5 % (n = 59) and 30.4 % (n = 52) of patients, respectively.
After PMTs, media dissections were seen in 71.2 % of cases (37 of 52) and calcium fractures in 69.2 % (36 of 52). In 30.8 % of patients (16 of 52), multiple calcium fractures occurred at different locations. This was less common in the RA group.
Device success rates were similar across all three treatment arms, with no significant differences in the need for a second advanced PMT (RA, 10.5 % [6 of 57]; IVL, 10.5 % [6 of 57]; ELCA, 14 % [8 of 57]). The main reason for needing a second PMT varied: in the IVL and ELCA arms, it was due to the lesion being uncrossable, while in the RA arm, it was due to the lesion being undilatable. Angiographic, procedural, and clinical success rates were also comparable across all arms.
No differences were observed in MSA in the 3 treatment arms (RA, 5.5 ± 2.1 mm2; IVL, 5.4 ± 1.8 mm2; ELCA, 5.1 ± 1.8 mm2). There were no differences in stent expansion between the IVL and RA arms (RA, 86.4 % ± 14.1 %; IVL, 85.6 % ± 13.3 %; P = 0.77), and IVL proved to be non-inferior to RA in all analyses performed.
Regarding the comparison between RA and ELCA, in the ITT analysis, ELCA did not reach the non-inferiority threshold (RA, 86.4 % ± 14.1 %; ELCA, 80.3 % ± 13.3), although the difference between RA and ELCA became non-significant when stent expansion was analysed by the last technique used (RA, 84.3 ± 15.2; ELCA, 81.4 ± 12.3) or in cases without the need for an additional PMT (RA, 85.96 ± 14.2; ELCA, 81.4 ± 12.5). The radial or ulnar approach was used in the majority of procedures (84.2 %), demonstrating also the feasibility of PMT for calcified lesions via these access sites.
Complication rates were low and similar across all three arms, with no procedure-related deaths, flow-limiting dissections, or abrupt vessel occlusions.
Critical reading and the relevance for clinical practice
This study is the first randomised trial comparing RA, IVL, and ELCA for calcified coronary lesions. The key findings of the study are:
- IVL was non-inferior to RA in stent expansion measured on OCT;
- ELCA did not meet the non-inferiority margin in ITT analysis against RA, but showed no significant difference when analysed by the last technique or without additional PMT use;
- A second PMT was required in 10.5 %-14 % of cases, with varying reasons across arms;
- Success rates and MSAs were similar across groups;
- And complication rates were low, with IVL showing the fewest numerically.
Interpreting the results requires considering that the primary endpoint was analysed on an ITT basis. In cases where multiple techniques were used, the final effect may reflect their combination (e.g., rotatripsy) or only the second technique (e.g., IVL cases treated solely with RA). This explains why ELCA vs. RA differences in the ITT analysis diminished when analysed by the last technique or in cases without a second PMT. The need for additional PMTs is understandable based on their mechanisms. In the RA arm, the main issue was undilatable lesions, due to RA's limited effect, especially on deep calcium, as seen in fewer OCT-detected fractures. In the IVL and ELCA arms, difficulty in crossing the lesion was the primary challenge. ELCA, compatible with any 0.014-inch guidewire, is commonly used for uncrossable lesions, and its ability to modify deeper vessel layers also makes it effective for undilatable lesions3.
A similar study to the ROLLER-COASTR-EPIC22 trial is the ROTA.shock trial4, which randomised 70 patients with calcified lesions to either RA or IVL, finding comparable MSA and stent expansion between the two. Despite more severe calcification in the ROLLER-COASTR-EPIC22 trial, stent expansion was nearly identical (84.7 % vs. 83 %). The less severe lesions in the ROTA.shock study may explain the lower crossover rate observed in this study, where only two patients in the IVL group required RA.
In short, this study confirms the efficacy, safety, and complementary nature of RA, IVL, and ELCA for calcified coronary lesions, as no single technique can treat all cases. While this trial compares 3 PMTs, there remain the question regarding how orbital atherectomy performs in comparison to these more established PMT for calcified lesions. Thus, selection should be guided by patient and lesion characteristics, with these findings providing valuable randomised evidence to inform clinical decisions.
When applying the results of this study to daily practice, several limitations should be considered. First, patients were not enrolled consecutively, which could introduce bias. Additionally, randomisation was performed after observing calcification, without considering whether the lesion was crossable or dilatable, which may have influenced the need for a second PMT. OCT data before and after PMT was available for only one-third of the sample, limiting its interpretability. The use of small burrs (1.25 and 1.5 mm) in many patients may have also impacted the results. Finally, the necessity for a second technique complicated the interpretation of stent expansion in the ITT analysis, however reflects an increasingly prevalent real-world practice where multiple tools in the calcium modification armamentarium are being used..
To conclude, in the first randomised trial comparing RA, IVL, and ELCA for calcified coronary lesions, IVL was non-inferior to RA in stent expansion, while ELCA did not meet this threshold. No significant differences were found between the three treatments in terms of MSA, procedural success, or complications, although complications were numerically lower with IVL.
References
- Jurado-Román A, Gómez-Menchero A, Gonzalo N, et al. Plaque modification techniques to treat calcified coronary lesions. Position paper from the ACI-SEC. REC Interv Cardiol. 2023;5:46–61.
- di Mario C, Koskinas KC, Räber L. Clinical benefit of IVUS guidance for coronary stenting: the ultimate step toward definitive evidence? J Am Coll Cardiol. 2018;72:3138–3141.
- Karacsonyi J, Armstrong EJ, Truong HTD, et al. Contemporary use of laser during percutaneous coronary interventions: insights from the Laser Veterans Affairs (LAVA) multicenter registry. J Invasive Cardiol. 2018;30:195–201.
- Blachutzik F, Meier S, Weissner M, et al. Coronary intravascular lithotripsy and rotational atherectomy for severely calcified stenosis: results from the ROTA.shock trial. Catheter Cardiovasc Interv. 2023;102:823–833.








No comments yet!