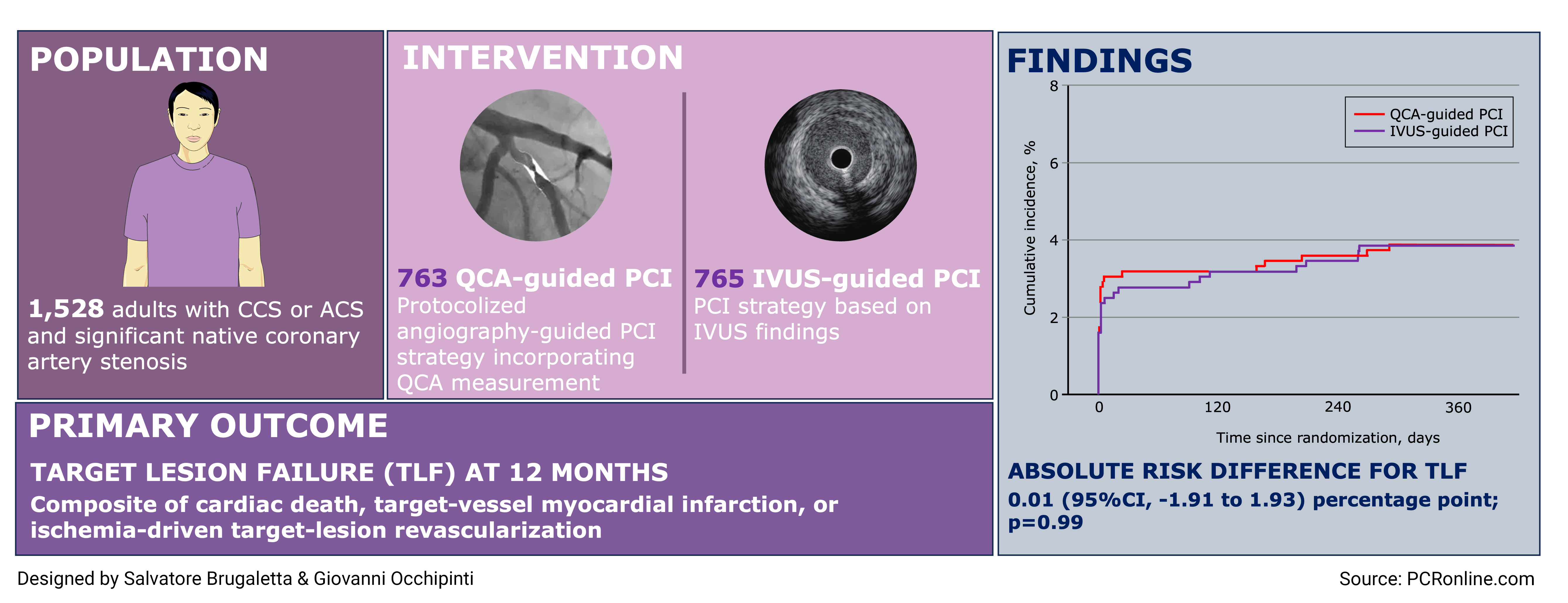
Quantitative coronary angiography vs intravascular ultrasonography to guide drug-eluting stent implantation - a randomized clinical trial
Selected in JAMA Cardiology by G. Occhipinti , S. Brugaletta
The trial aimed to establish the non-inferiority of QCA-guided PCI compared to IVUS-guided PCI with respect to the primary endpoint of TLF at 12 months, defined as a composite of cardiac death, target vessel MI, or ischemia-driven target lesion revascularization.
References
Authors
Pil Hyung Lee, Soon Jun Hong, Hyun-Sook Kim, Young won Yoon, Jong-Young Lee, Seung-Jin Oh, Ji Sung Lee, Soo-Jin Kang, Young-Hak Kim, Seong-Wook Park, Seung-Whan Lee, Cheol Whan Lee, for the GUIDE-DES Trial Research Group
Reference
JAMA Cardiol. Published online March 13, 2024. doi:10.1001/jamacardio.2024.0059
Published
March 13, 2024
Link
Read the abstractReviewers
Our Comment
Why this study – the rationale/objective?
Over the past decade, mounting evidence supports the notion that intravascular imaging (IVI) guidance for percutaneous coronary interventions (PCI) enhances clinical outcomes, compared to the two-dimensional visualization of coronary artery provided by invasive coronary angiography (ICA), as a result of superior precision in defining vessel diameter, ensuring optimal stent expansion, and identifying acute complication.
However, IVI may be unavailable in many centers and the present study aimed to evaluate a novel, on-site, quantitative coronary angiography (QCA)-guided strategy as non-inferior to the IVUS-guided strategy in patients undergoing PCI.
How was it executed – the methodology?
This was a randomized, open-label, non-inferiority clinical trial that included adults (aged ≥ 18 years) with chronic or acute coronary syndrome and angiographically confirmed native coronary artery stenosis requiring PCI. Patients were enrolled in 6 cardiac centers in Korea from February 23, 2017, to August 23, 2021, and follow-up occurred through August 25, 2022. All principal analyses were performed according to the intention-to-treat principle.
After guidewire crossing of the target lesion, patients were randomized in a 1:1 ratio to undergo either QCA- or IVUS-guided PCI. In the QCA-guided PCI arm, lumen diameters at reference segments were measured using the automatic calibration software, and stent size chosen based on the distal reference segment's diameter. Balloon post-dilation was mandatory. In the IVUS-guided PCI arm, stent size was determined via IVUS measurements, with balloon post-dilation left to the operator's discretion.
The trial aimed to establish the non-inferiority of QCA-guided PCI compared to IVUS-guided PCI with respect to the primary endpoint of target lesion failure (TLF) at 12 months, defined as a composite of cardiac death, target vessel myocardial infarction, or ischemia-driven target lesion revascularization. This comparison was based on an 8 % expected event rate in the control arm, with a non-inferiority margin of 3.5 %, and 80 % power at a 1-sided type I error of 2.5 %.
What is the main result?
A total of 1,528 patients who underwent PCI were enrolled and randomly assigned to either QCA-guided PCI group (n = 763; mean age, 64.1 years) or IVUS-guided PCI group (n = 765; mean age, 64.6 years). Approximately one-third of patients in both groups had i) diabetes mellitus, and ii) presented with acute coronary syndromes. Female were under-represented (n = 189; 24.8 % in the QCA-guided PCI group; n = 143; 18.7 % in the IVUS-guided PCI group).
At 12 months, the primary end point of TLF occurred in 29 patients (3.81 %) in the QCA-guided PCI group and 29 patients (3.80 %) in the IVUS-guided PCI group (absolute risk difference, 0.01 percentage points [95 % CI, –1.91 to 1.93 percentage points]; HR, 1.00 [95 % CI, 0.60-1.68]; P = 0.99). Secondary clinical events were infrequent and similar in both groups. Nine cases of definite or probable stent thrombosis occurred, of which 4 cases occurred in the subacute phase (> 24 hours to 30 days after PCI).
In terms of death, 13 events occurred, of those 7 in the investigational arm and 6 in the control group (absolute risk difference, 0.13 percentage points [95 % CI, –0.79 to 1.06 percentage points]). A total of 51 cases of myocardial infarction occurred, 26 in the QCA-guided PCI group and 25 in the IVUS-guided PCI (absolute risk difference, 0.14 percentage points [95 % CI, –1.66 to 1.94 percentage points]).
In post hoc subgroup analyses, the risk of the primary end point was consistent regardless of subgroup, with no significant interactions.
Trial summary designed by Salvatore Brugaletta & Giovanni Occhipinti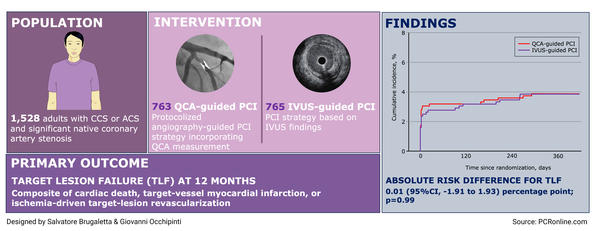
Critical reading and the relevance for clinical practice
Temporal trends in IVI-guided PCI in the United States demonstrate an increase from 9.5 % to 15.4 % between 2013 and 2019. To address potential limitations in the low rate of IVUS utilization - generally attributed to financial constraints, regulatory and reimbursement issues, and limited expertise - this study incorporated a protocol integrating real-time QCA measurement, which, without interrupting catheterization laboratory workflow, imposes no additional costs to PCI procedures and utilizes widely available equipment.
While previous large randomized trials comparing IVUS- with ICA-guided PCI (e.g., ULTIMATE and IVUS-XPL trials) revealed a lower incidence of target vessel failure with IVUS-guided PCI, primarily due to a significant reduction in target lesion revascularization, other smaller trials have yielded comparable outcomes, leading to some degree of uncertainty.
On this background, the GUIDE-DES trial represents the first effort to demonstrate the feasibility of a protocolized angiography-guided PCI strategy in clinical practice, in an evolving landscape suggesting potential future attractiveness related to the introduction of deep learning models capable of automatically segmenting vessels. Despite being the largest and most recent trial comparing QCA- versus IVUS-guided PCI, the reduced statistical power to detect differences between the two groups, within a context of low-event rate for the primary endpoint (observed: 3.8 % versus expected: 8.0 %), may disappoint expectations and reduce the reliability of the results.
While randomized controlled trials serve as the foundation of clinical guidelines, their complexity in design may not always yield expected results. This is particularly true in non-inferiority trials, where the choice of pre-defined non-inferiority margins according to expected event rate for the primary endpoint is crucial. To have wider margins or significantly higher expected event rates during trial design limit the sample size, but it may carry the risk of failing in achieving the desired results.
Moving to a critical appraisal, although hypothesis-generating, we could assume that QCA-guided PCI approach potentially yields comparable outcomes with respect to IVUS-guided PCI.
However, it is important to consider the clinical context where these findings were achieved, which is of a low angiographic complexity, characterized by a mean Syntax Score of ~ 13 points.
Nevertheless, quantitative assessment of the vessel at the lesion level may represent an interesting tool with the potential to enhance the post-procedural performance in specific anatomical scenarios. This approach, together with the upcoming development of artificial intelligence technologies, may open the way toward use of real-time QCA for PCI guidance in context of low-complexity procedures, where IVI does not probably translate into an improvement of clinical outcomes, as demonstrated for complex coronary scenarios (bifurcation lesions, left main disease, etc.).







No comments yet!