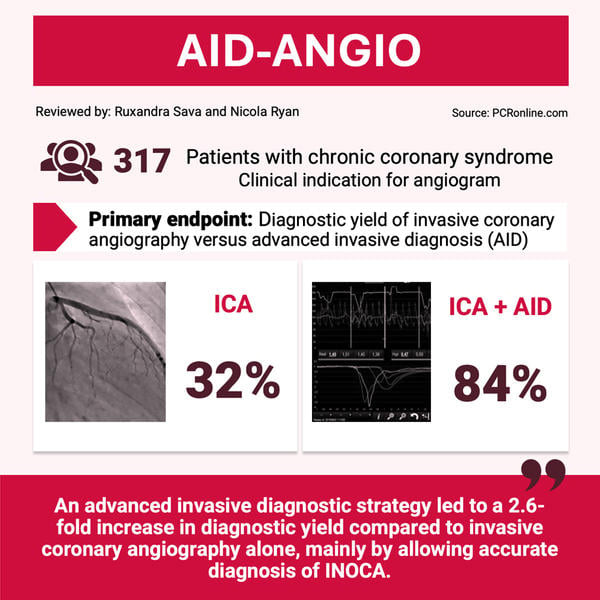
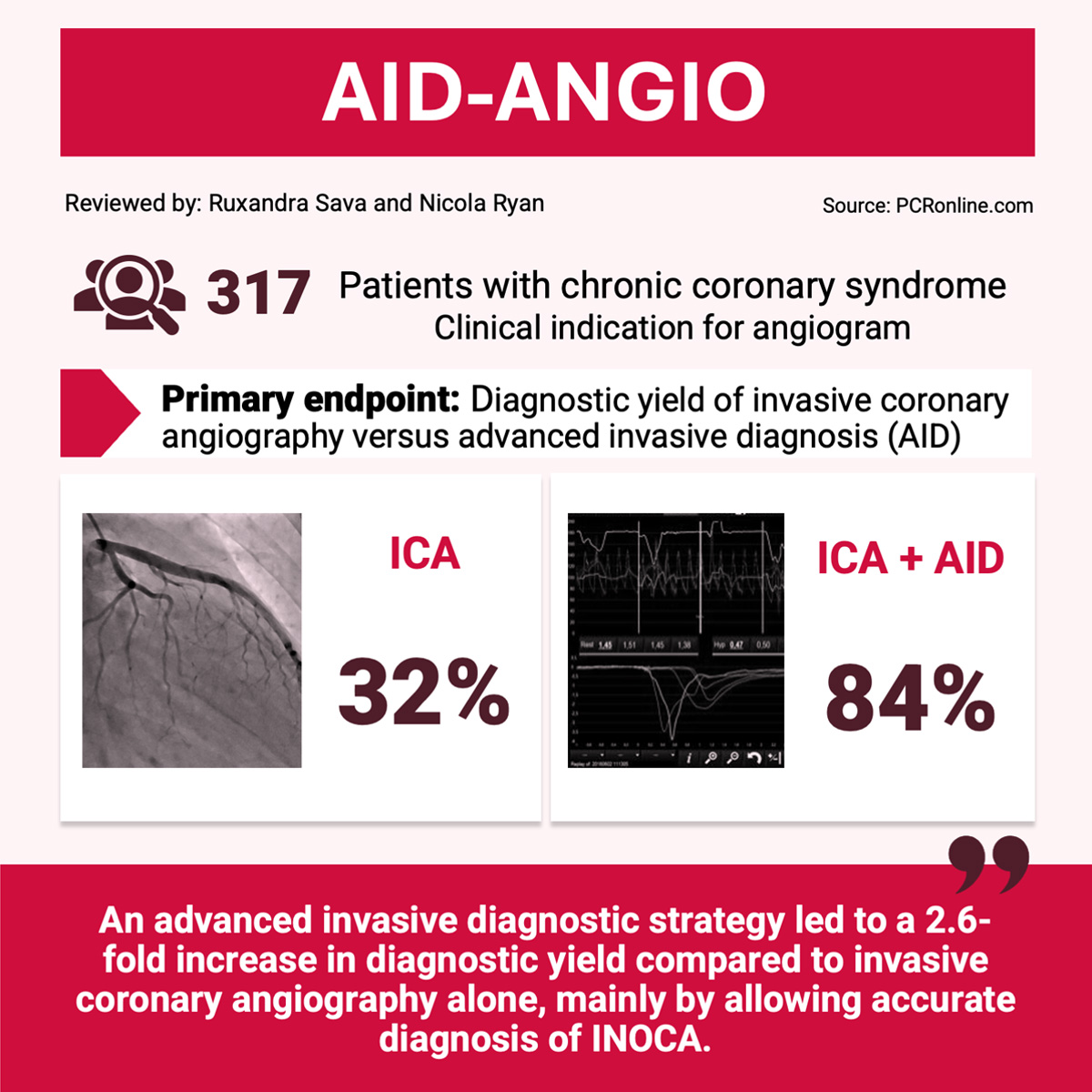
Comprehensive diagnosis in chronic coronary syndromes combining angiography and intracoronary testing: the AID-ANGIO study
Selected in EuroIntervention Journal by R. Sava , N. Ryan
The authors hypothesized that enriching invasive coronary angiography (ICA) with an advanced invasive diagnosis (AID) strategy would increase the diagnostic yield of obstructive and non-obstructive coronary artery disease (INOCA).
References
Authors
Adrián Jerónimo, José G. Paredes-Vázquez, Alejandro Travieso, Asad Shabbir, Pilar Jiménez-Quevedo, Fernando Macaya-Ten, Luis Nombela-Franco, Iván J. Núñez-Gil, Pablo Salinas, Juan Carlos Gómez-Polo, Daniel García-Arribas, Isidre Vilacosta, Javier García Pérez-Velasco, Eva García-Romo, Alberto García-Lledó, Juan Manuel Grande-Ingelmo, Inmaculada Fernández-Rozas, Javier Alonso-Belló, Alejandro Curcio, Antonio I. Fernández-Ortiz, Julián P. Villacastín, Hernán Mejía-Rentería, Nieves Gonzalo, Javier Escaned
Reference
10.4244/EIJ-D-24-00499 • Jan 6, 2025
Published
Jan 6, 2025
Link
Read the abstractReviewers
Our Comment
Designed by Ruxandra Sava & Nicola Ryan - Source: PCRonline
Why this study – the rationale/objective?
Invasive coronary angiography (ICA) is considered the gold standard to identify obstructive coronary artery disease, however the diagnostic yield in chronic coronary syndrome (CCS) is low. The authors hypothesized that enriching ICA with an advanced invasive diagnosis (AID) strategy would increase the diagnostic yield of obstructive and non-obstructive coronary artery disease (INOCA).
How was it executed – the methodology?
This was an observational, all-comers, prospective study performed at 4 hospitals in Madrid, Spain, enrolling patients with CCS referred for further evaluation.
There were minimal exclusion criteria: patients with congestive heart failure, severe left ventricular dysfunction, previous coronary artery bypass graft, and those treated with PCI within the last 3 months. Obstructive coronary artery disease was classified as an epicardial stenosis ≥ 90 %, with lesser stenosis being considered intermediate.
The AID strategy consisted of the following:
- Coronary physiology using the PressureWire X Guidewire (Abbott), capable of both pressure and thermodilution measurements, with the CoroFlow Cardiovascular System (Coroventis)
- Intermediate stenosis were evaluated with FFR +/- iFR
- Endothelial-independent coronary microvascular dysfunction (CMD) testing: thermodilution measurement of coronary flow reserve (CFR, abnormal < 2.0) and/or the index of microcirculatory resistance (IMR, increased >= 25) after hyperemia induction by intravenous adenosine at 140 μg/kg/min.
- Endothelial-dependent coronary function: testing for epicardial or microvascular spasm with sequential boluses of intracoronary acetylcholine (LM: 2, 20, 100 and 200 µg, RCA: 2, 20 and 80 µg)
To evaluate the impact of ICA and AID on decision making, the following protocol was employed:
- Step 1: referring cardiologists were shown the ICA, and were asked to judge the presence of obstructive CAD
- Step 2: referring cardiologists were asked to integrate the results of previous clinical data (including non-invasive ischemia testing, available in 61 % of patients) with the ICA and establish a diagnosis of obstructive CAD, INOCA or no ischemia, as well as a treatment plan
- Step 3: referring and interventional cardiologists (Ischemia Team) case review and definitive diagnosis based on clinical, ICA and AID findings.
- The primary outcome was the diagnostic yield of ICA alone (without considering clinical history and results of non-invasive ischemia testing) versus ICA performed together with an AID strategy.
- The secondary outcomes focused on the proportion of patients in which INOCA and its endotypes were specified by using a diagnostic strategy based on clinical data and ICA, vs ICA and AID, as well as the impact of performing AID on treatment decisions.
What is the main result?
From 365 consecutive patients, 317 fulfilled inclusion criteria, 44.2 % were women, with a mean age of 66 years. Almost two thirds of patients had undergone a non-invasive ischaemia test or CTCA prior to enrollment.
- Addition of AID vs ICA alone led to a diagnosis of myocardial ischemia in 84.2 % vs 32.2 % (p < 0.001)
- ICA alone revealed obstructive CAD in 102 patients (32.2 %), intermediate stenosis in 74 patients (23.3 %), and no stenosis in 141 patients (44.5 %)
- Integrating prior clinical information and ICA findings lead to a diagnosis of obstructive CAD in 126 patients (39.7 %), INOCA in 165 patients (52.1 %) and no ischemia in 26 patients (8.2 %).
- Integrating AID, obstructive CAD was diagnosed in 39.1 % and INOCA in 45.1 % (22.4 % microvascular dysfunction, 54.5 % vasomotor disorders and 23.1 % mixed), 15.8 % had no evident cause of myocardial ischemia.
- Using AID led to change in management strategy in 190 patients (59.9 %).
- A tentative diagnosis of INOCA was made in 165 patients post ICA prior to integrating the AID; this diagnosis was refuted in 78.2 % of cases due to either INOCA not being confirmed on AID (35.7 %) or an incorrect endotype identified (64.3 %)
Critical reading and the relevance for clinical practice
The AID-ANGIO study builds upon our knowledge of the limitations of coronary angiography alone in obtaining a diagnosis in patients with chronic coronary syndrome. Similar to prior studies, slightly over a third of patients had obstructive coronary artery disease using ICA alone, potentially leaving two thirds of patients without a definitive diagnosis leaving the catheterization laboratory. Whilst, in daily clinical practice, the angiography result is never interpreted in isolation and clinical and prior non-invasive tests are integrated into decision making, this is reflected in the similar diagnostic yield for obstructive CAD diagnosed in 39.7 % of patients, based on clinical history and ICA, vs. 39.1 % using AID. This is likely due to positive non-invasive ischemia testing leading to an intermediate coronary stenosis being classified as significant, similarly to invasive testing.
An important finding of this study is that INOCA occurred in 45.1 % of patients presenting with CCS, with a similar prevalence in patients with no obstructive CAD and physiologically non-significant coronary lesions. The 2024 ESC Guidelines for the management of chronic coronary syndromes1 have recommended the use of invasive coronary testing (I, B) in patients with non-obstructive disease. Whilst INOCA was suspected based on integration of clinical data and ICA in 165 patients (52.1 %), in 78 % of these cases there was a discrepancy between this and the AID results. Integration of AID lead to refuting the diagnosis of INOCA (35.7 %) or reclassification of the INOCA endotype (64.3 %).
Overall, a small percentage of patients had no cause identified for their clinical angina and or myocardial ischaemia on non-invasive testing and or presence of CAD on CCTA (15.8 %). It is unclear from the data provided what clinical symptoms and or non-invasive investigations lead to these patients being referred for invasive angiography.
As with all studies, there are a number of limitations, this study used a cutpoint of 2.0 for CFR, the COVADIS group2 recognizing a grey zone between 2.0-2.5, and the ESC INOCA consensus document recommending a 2.5 threshold3. There is a potential that some patients falling into the 2.0-2.5 range may have been classified as “normal”.
A significant limitation in the field of INOCA, is the absence of robust outcome data following treatment initiation. The CorMica trial demonstrated improvement in quality of life and decreased healthcare usage following stratified medical therapy, however data supporting the use of specific therapies in INOCA are limited and is an area that requires significant further research. However, INOCA phenotyping is a critical step in the right direction allowing an understanding of the true prevalence within the general population, as well as allowing initiation of stratified treatment, which has been associated with improvement in angina and quality of life4. Finally, from a patient perspective obtaining a specific diagnosis allows them to manage and advocate for their own health.
Catheterisation laboratory time pressures are commonly cited as a reason to avoid further testing however the AID added only a mean of 15 minutes to the procedure. Furthermore, concerns exist with regard to the safety of AID, in particular spasm provocation with Acetyl Choline, overall there were 8 cases of transient atrial fibrillation after acetylcholine provocation and one episode of ventricular fibrillation due to extensive epicardial spasm treated with electrical cardioversion and intracoronary nitrates, with no fatalities.
This study supports the clinical value of invasive coronary testing in a real world population, with further research required to determine the optimal treatment strategy once a diagnosis has been made.
Related interview
To dive deeper, don't miss this video where Christopher Cook interviews Javier Escaned, exploring the AID-ANGIO study's purpose, methodology, and key outcomes!
References
- Vrints C, Andreotti F, Koskinas KC, Rossello X, Adamo M, Ainslie J, Banning AP, Budaj A, Buechel RR, Chiariello GA, Chieffo A, Christodorescu RM, Deaton C, Doenst T, Jones HW, Kunadian V, Mehilli J, Milojevic M, Piek JJ, Pugliese F, Rubboli A, Semb AG, Senior R, Ten Berg JM, Van Belle E, Van Craenenbroeck EM, Vidal-Perez R, Winther S; ESC Scientific Document Group. 2024 ESC Guidelines for the management of chronic coronary syndromes. Eur Heart J. 2024 Sep 29;45(36):3415-3537. doi: 10.1093/eurheartj/ehae177. PMID: 39210710.
- Rahman H, Demir OM, Ryan M, McConkey H, Scannell C, Ellis H, Webb A, Chiribiri A, Perera D. Optimal Use of Vasodilators for Diagnosis of Microvascular Angina in the Cardiac Catheterization Laboratory. Circ Cardiovasc Interv. 2020 Jun;13(6):e009019. doi: 10.1161/CIRCINTERVENTIONS.120.009019. Epub 2020 Jun 10. PMID: 32519879; PMCID: PMC7299228.
- Kunadian V, Chieffo A, Camici PG, Berry C, Escaned J, Maas AHEM, Prescott E, Karam N, Appelman Y, Fraccaro C, Buchanan GL, Manzo-Silberman S, Al-Lamee R, Regar E, Lansky A, Abbott JD, Badimon L, Duncker DJ, Mehran R, Capodanno D, Baumbach A. An EAPCI Expert Consensus Document on Ischaemia with Non-Obstructive Coronary Arteries in Collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation Endorsed by Coronary Vasomotor Disorders International Study Group. EuroIntervention. 2021 Jan 20;16(13):1049-1069. doi: 10.4244/EIJY20M07_01. PMID: 32624456; PMCID: PMC9707543.
- Ford TJ, Stanley B, Good R, Rocchiccioli P, McEntegart M, Watkins S, Eteiba H, Shaukat A, Lindsay M, Robertson K, Hood S, McGeoch R, McDade R, Yii E, Sidik N, McCartney P, Corcoran D, Collison D, Rush C, McConnachie A, Touyz RM, Oldroyd KG, Berry C. Stratified Medical Therapy Using Invasive Coronary Function Testing in Angina: The CorMicA Trial. J Am Coll Cardiol. 2018 Dec 11;72(23 Pt A):2841-2855. doi: 10.1016/j.jacc.2018.09.006. Epub 2018 Sep 25. PMID: 30266608.





No comments yet!