Outcomes after CABG compared with FFR-guided PCI in patients presenting with acute coronary syndrome
Selected in JACC: Cardiovascular Interventions by R. Sava , N. Ryan
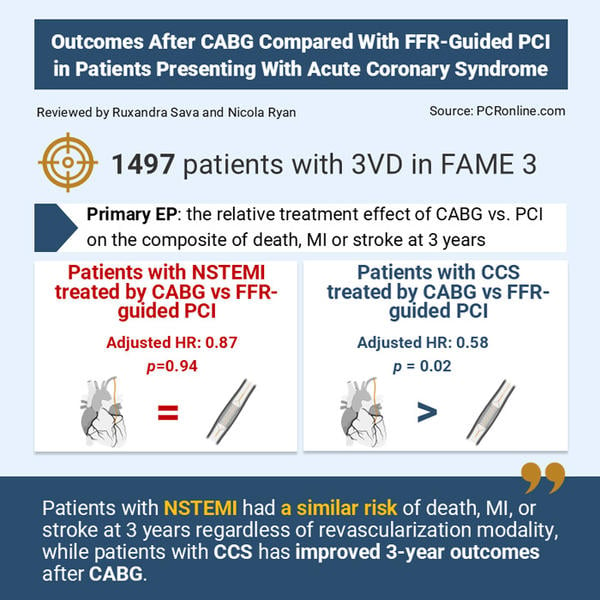
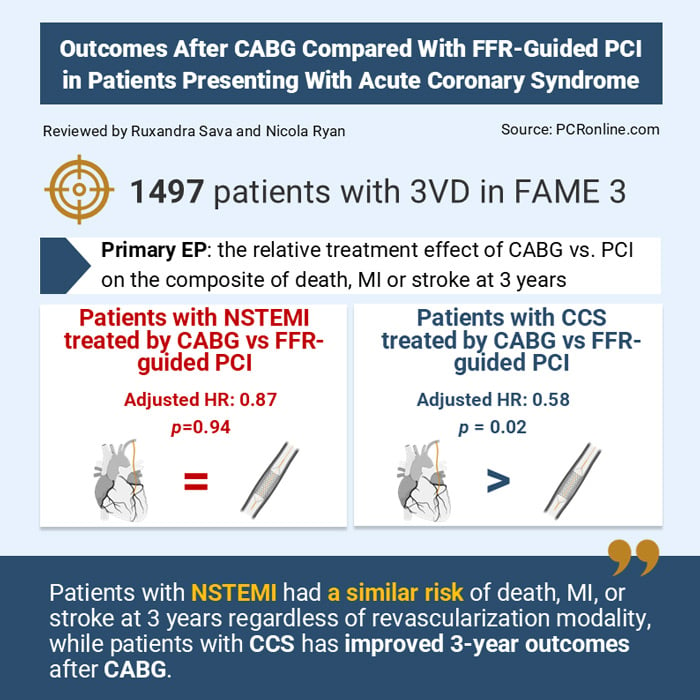
This prespecified analysis of the Fractional Flow Reserve versus Angiography for Multivessel Evaluation (FAME 3) trial examined the impact on cardiovascular outcomes of treatment by CABG versus FFR-guided PCI in patients with three vessel disease (3-VD), stratified by acute (NSTEMI) or chronic coronary syndrome (CCS) presentation.
References
Authors
Kuniaki Takahashi, Hisao Otsuki, Frederik M. Zimmermann, Victoria Y. Ding, Zsolt Piroth, Keith G. Oldroyd, Olaf Wendler, Michael J. Reardon, Manisha Desai, Y. Joseph Woo, Alan C. Yeung, Bernard De Bruyne, Nico H.J. Pijls, William F. Fearon, and the FAME 3 Trial Investigators
Reference
J Am Coll Cardiol Intv. 2025 Apr, 18 (7) 838–848
Published
2025 Apr, 18
Link
Read the abstractReviewers
Our Comment
Reviewed by Ruxandra Sava and Nicola Ryan
Source: PCRonline.com
Why this study – the rationale/objective?
While treatment with CABG has consistently outperformed PCI in randomised clinical trials (RCT) enrolling patients with multivessel coronary artery disease, it remains uncertain whether this effect extends to patients presenting with an acute coronary event, such as non-ST elevation myocardial infarction (NSTEMI). Indeed, most trials have typically included patients with chronic coronary syndrome.
This prespecified analysis of the Fractional Flow Reserve versus Angiography for Multivessel Evaluation (FAME 3) trial examined the impact on cardiovascular outcomes of treatment by CABG versus FFR-guided PCI in patients with three-vessel disease (3-VD), stratified by acute (NSTEMI) or chronic coronary syndrome (CCS) presentation.
How was it executed - the methodology
The FAME 3 trial was an international, non-inferiority trial in which patients with angiographically-defined 3-VD were randomised to FFR-guided PCI versus CABG.
Patients with significant left main involvement, recent or present STEMI and those with a left ventricular ejection fraction < 30 % were excluded.
The primary outcome, including all-cause death myocardial infarction (MI), repeat revascularisation or stroke at one year, did not demonstrate non-inferiority1. However, at three3 and five years2, the rate of the key pre-specified secondary endpoint of all-cause death, MI and stroke was similar regardless of revascularisation technique. The exclusion of the repeat revascularisation variable was motivated by a desire to remove the inherent clinical subjectivity associated with this decision.
For this pre-specified analysis, cumulative indices of outcomes were evaluated up to three years using the Kaplan-Meier estimator. Confounding variables were accounted for by multivariable analysis. The relative effect of treatment of CABG or FFR-guided PCI in patients presenting with NSTEMI or CCS was studied by the interaction term in a Cox proportional hazard model.
What is the main result?
Out of 1,497 patients, 587 (39.2 %) presented with NSTEMI. These patients were slightly younger and had lower comorbidity burden than patients presenting with CCS. However, they were more likely to have previously suffered an ACS (58.6 % vs 17.1 %, p < 0.001).
When compared to patients presenting with CCS, patients with NSTEMI:
- Had a similar risk of the composite outcome of death, MI and stroke at 3 years, both in unadjusted (11.8 % vs 10.0 %, HR 1.19, 95 % CI 0.87-1.64, p = 0.27) and adjusted analysis (HR 1.20, 95 % CI 0.81-1.77, p = 0.37).
- Had a higher rate of MI in unadjusted analysis (7.3 % vs 4.7 %, unadjusted HR 1.58; 95 % CI 1.03-2.42; p = 0.04), a rate that became non-significant after adjustment (adjusted HR: 1.68, 95 % CI 0.99-2.87, p = 0.06). This difference was mostly driven by an increased frequency of peri-procedural MI.
- There was no significant difference between the groups in terms of the original study primary endpoint of MI, repeat revascularisation, stroke or death, neither in unadjusted nor in adjusted analysis.
The relative treatment effect of FFR-guided PCI versus CABG:
- In patients treated for NSTEMI, the risk of death, MI or stroke at 3 years was similar, regardless of treatment by FFR-guided PCI or CABG (11.8 % vs 11.8 %, adjusted HR 0.98, 95 % CI 0.6-1.6, p = 0.94).
- In patients treated for CCS, the risk of death, MI or stroke at 3 years was significantly lower in patients treated by CABG (7.6 % vs 12.4 %, adjusted HR 0.58, 95 % CI 0.38-0.9, p = 0.02, p for interaction = 0.02).
Critical reading and the relevance for clinical practice
This pre-specified sub-analysis of the FAME 3 randomised trial, whilst only hypothesis generating as the trial failed to meet its primary endpoint, suggests that ischemia-guided PCI may lead to comparable clinical outcomes to CABG in patients with 3-VD and NSTEMI. In contrast and aligned with prior data in patients presenting with CCS, CABG was associated with improved 3-year rates of death, MI or stroke.
The strengths of the study include randomised allocation to PCI or CABG, the collection of data regarding anatomical CAD severity, as well as that of protocol-mandated FFR measurement, which may reduce the number of implanted stents as well as peri-procedural MI. However, the study presents significant limitations. FAME 3’s primary endpoint at one year was negative, which raises questions regarding the trial’s overall power to show significant benefit, especially in a subgroup analysis. An additional criticism is the low rate of intravascular imaging, which at 12 % reflects clinical use, but not state-of-the-art PCI.
NSTEMI patients differ significantly from those presenting with CCS. In this analysis, they had increased rates of both prior MI and MI during follow-up. Given they commonly present with plaque and/or haemodynamic instability, revascularisation timing is likely a key factor impacting outcomes in this patient population. Considering that surgical revascularisation acutely, is often delayed by numerous system and patient-related factors, PCI emerges as an attractive alternative. This is supported by the current study, showing shorter treatment delays with PCI versus CABG (2 vs 7 days, p < 0.001), as well as an early initial separation of outcome curves in the detriment of CABG in NSTEMI patients, but not in CCS patients.
Prior studies have shown that the benefit conferred by CABG vs PCI in multi-vessel CAD is largely derived from reduced rates of repeat revascularisation5 and spontaneous myocardial infarction (MI)6. The current analysis confirms these findings in CCS patients, who had lower rates of spontaneous MI after CABG (1.5 % vs 5.7 %, p < 0.001).
However, this did not hold true for NSTEMI patients, which presented with similar rates of spontaneous MI (5.2 % vs 4.3 %, p = 0.61) and of repeat revascularisation (7.5 % vs 10.9 %, p = 0.15) regardless of revascularisation by CABG or PCI, respectively.
One of the possible reasons is that lesion complexity was lower in this group. Indeed, the mean SYNTAX anatomical score was lower in NSTEMI patients treated by PCI (25.1 ± 6.8 vs 26.5 ± 7.2, p = 0.009) and numerically more of these patients fell within the low SYNTAX category (38.2 % vs 32 % in NSTEMI vs CCS patients, respectively). The functional SYNTAX score, defined as the SYNTAX score of all coronary arteries with an FFR < 0.88, was also significantly lower in those presenting with NSTEMI (21.7 ± 8.3 vs 23.3 ± 8.5, 0.01). These findings are aligned with prior data demonstrating non-significant differences in MACCE in patients treated by PCI for three vessel disease with low SYNTAX scores, even when first generation DES were used8.
Finally, differing antiplatelet regimens after NSTEMI may have impacted results, with DAPT being prescribed at discharge much more often in those treated by PCI vs CABG (96.7 % vs 57.3 %, p < 0.001).
Although direct comparisons cannot be made between registry and randomised controlled trials, the recently published SWEDEHEART analysis including 57,097 patients offers real-world context. While this study showed a benefit of CABG in NSTEMI patients, with lower rates of all-cause death, MI and repeat revascularisation, the survival benefit was more important in patients aged < 70 years of age and those with left ventricular ejection fraction < 35 %, consistent with prior literature.
Interpreted in context, the present study raises the hypothesis that, in carefully selected NSTEMI patients such as those with low complexity CAD, ischemia-driven PCI has the potential to achieve similar outcomes to CABG. Improvements in PCI techniques, notably by enhanced use of intravascular imaging for procedural guidance and optimisation, may improve outcomes even more. Contradictory evidence demonstrates that clinical equipoise persists, and randomised controlled trials using state-of-the-art PCI combining intravascular imaging and physiology are required to determine if modern PCI techniques can achieve similar outcomes to CABG in patients with NSTEMI and 3-VD.
References
- Fearon WF, Zimmermann FM, Bruyne BD, et al. Fractional Flow Reserve–Guided PCI as Compared with Coronary Bypass Surgery. N Engl J Med. 2022;386(2):128-137. doi:10.1056/NEJMoa2112299
- Fearon WF, Zimmermann FM, Ding VY, et al. Outcomes after fractional flow reserve-guided percutaneous coronary intervention versus coronary artery bypass grafting (FAME 3): 5-year follow-up of a multicentre, open-label, randomised trial. The Lancet. 2025;405(10488):1481-1490. doi:10.1016/S0140-6736(25)00505-7
- Zimmermann FM, Ding VY, Pijls NHJ, et al. Fractional Flow Reserve–Guided PCI or Coronary Bypass Surgery for 3-Vessel Coronary Artery Disease: 3-Year Follow-Up of the FAME 3 Trial. Circulation. 2023;148(12):950-958. doi:10.1161/CIRCULATIONAHA.123.065770
- Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a pooled analysis of individual patient data - The Lancet. Accessed April 29, 2025. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)30423-9/abstract
- Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous Coronary Intervention versus Coronary-Artery Bypass Grafting for Severe Coronary Artery Disease. N Engl J Med. 2009;360(10):961-972. doi:10.1056/NEJMoa0804626
- Omerovic E, Råmunddal T, Petursson P, et al. Percutaneous vs. surgical revascularization of non-ST-segment elevation myocardial infarction with multivessel disease: the SWEDEHEART registry. Eur Heart J. 2024;46(6):518-531. doi:10.1093/eurheartj/ehae700
- Nam CW, Mangiacapra F, Entjes R, et al. Functional SYNTAX Score for Risk Assessment in Multivessel Coronary Artery Disease. J Am Coll Cardiol. 2011;58(12):1211-1218. doi:10.1016/j.jacc.2011.06.020
- Mohr FW, Morice MC, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. The Lancet. 2013;381(9867):629-638. doi:10.1016/S0140-6736(13)60141-5
- Banning AP, Serruys P, De Maria GL, et al. Five-year outcomes after state-of-the-art percutaneous coronary revascularization in patients with de novo three-vessel disease: final results of the SYNTAX II study. Eur Heart J. 2022;43(13):1307-1316. doi:10.1093/eurheartj/ehab703






No comments yet!